Ann Hepatobiliary Pancreat Surg.
2025 May;29(2):127-139. 10.14701/ahbps.25-012.
Is it time to define the scope of safety for robotic resection in perihilar cholangiocarcinoma surgery? A propensity score matching based analysis of a single center experience
- Affiliations
-
- 1Department of Hepato-Pancreato-Biliary Surgery, Moscow Clinical Scientific Center, Moscow, Russia
- 2Department of Interventional Radiology, Moscow Clinical Scientific Center, Moscow, Russia
- 3Moscow Clinical Scientific Center, Moscow, Russia
- KMID: 2568261
- DOI: http://doi.org/10.14701/ahbps.25-012
Abstract
- Backgrounds/Aims
Robotic surgery for perihilar cholangiocarcinoma is in the developmental and exploratory phase. The objective of this study was to compare the short-term outcomes and survival rates of robotic versus open resection for perihilar cholangiocarcinoma in a single center, and to determine the reliable scope of robotic interventions.
Methods
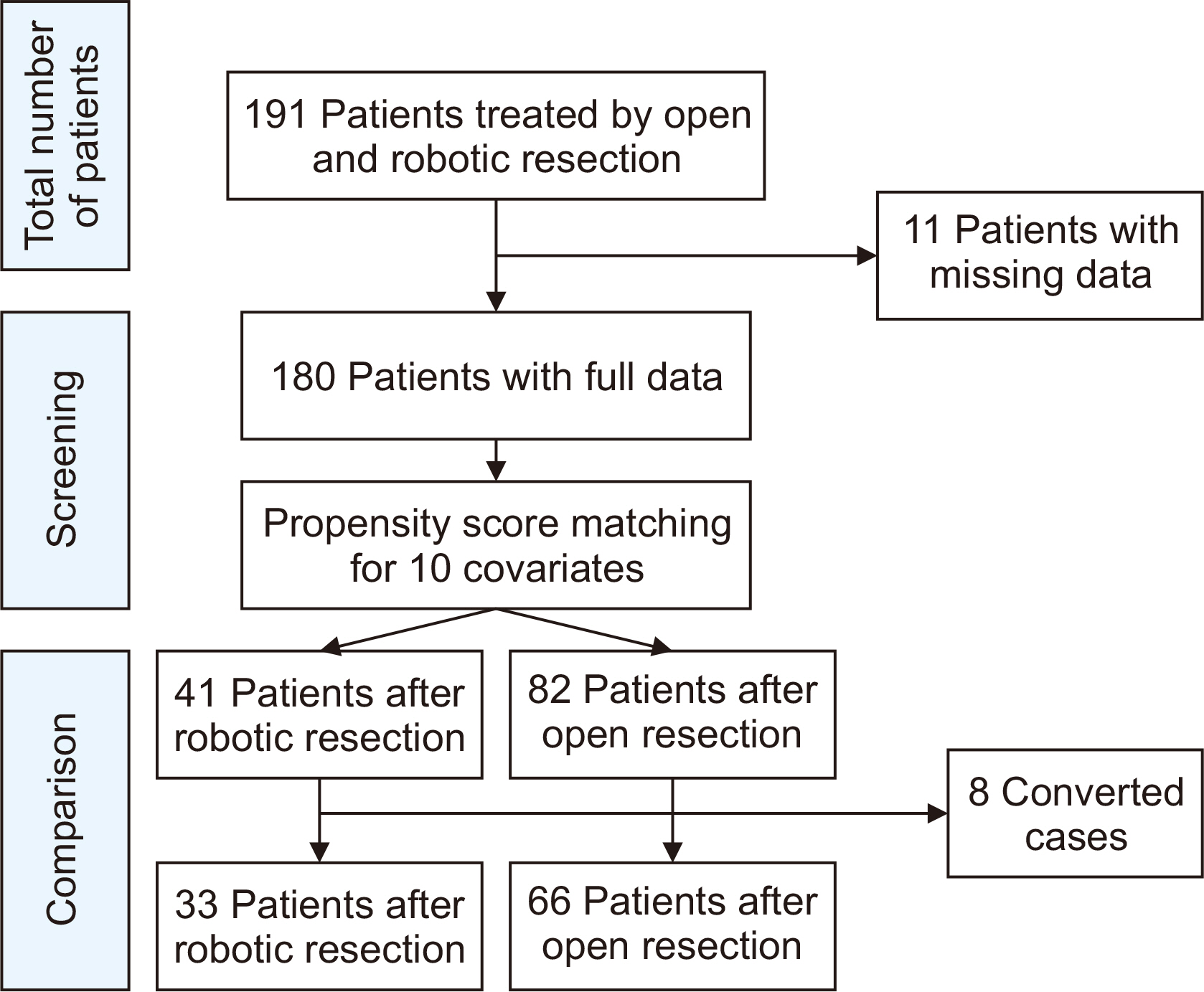
A comparative analysis of outcomes from open and robotic resections at a single center was conducted using propensity score matching (PSM). The balance of covariates was assessed using standardized mean differences, and the robotic resection procedures adhered to the standards of open surgery.
Results
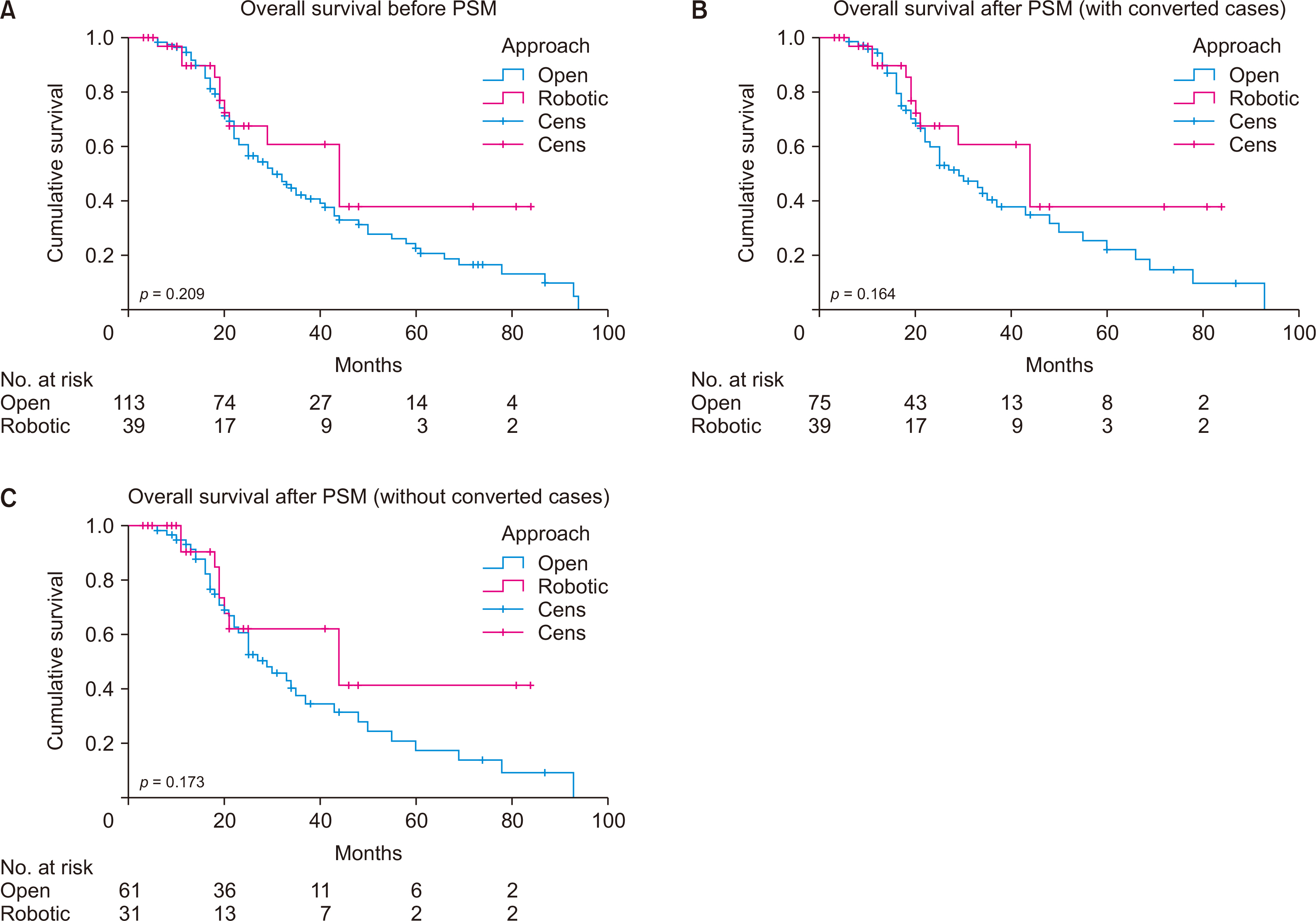
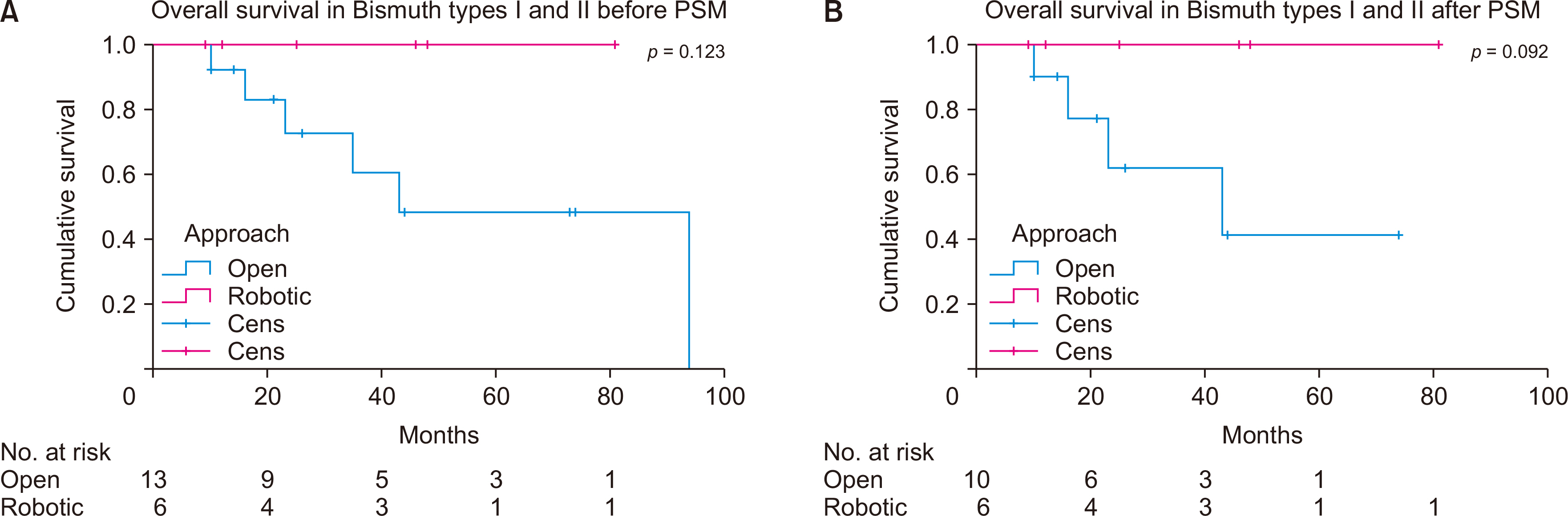
PSM was effectively applied between 41 robotic and 82 open resections. No differences were observed in blood loss, overall and severe morbidity, 90-day mortality, or length of hospital stay. Robotic resections were longer but resulted in better immediate oncological outcomes. Median overall survival for the robotic and open groups was 44 and 30 months (p = 0.259) before PSM and 44 and 29 months (p = 0.164) after PSM respectively. Conversion was required in 8 cases. A subgroup analysis excluding conversions revealed no differences in immediate and long-term outcomes. All patients undergoing robotic resection for Bismuth types I and II were alive at a mean follow-up of 37 months.
Conclusions
The robotic approach is comparable to open resection regarding immediate outcomes and survival in select patients with perihilar cholangiocarcinoma. For patients with Bismuth type I and II tumors and early (stages I and II) TNM stages, robotic resection is a reliable treatment option when aligned with the principles of open surgery.
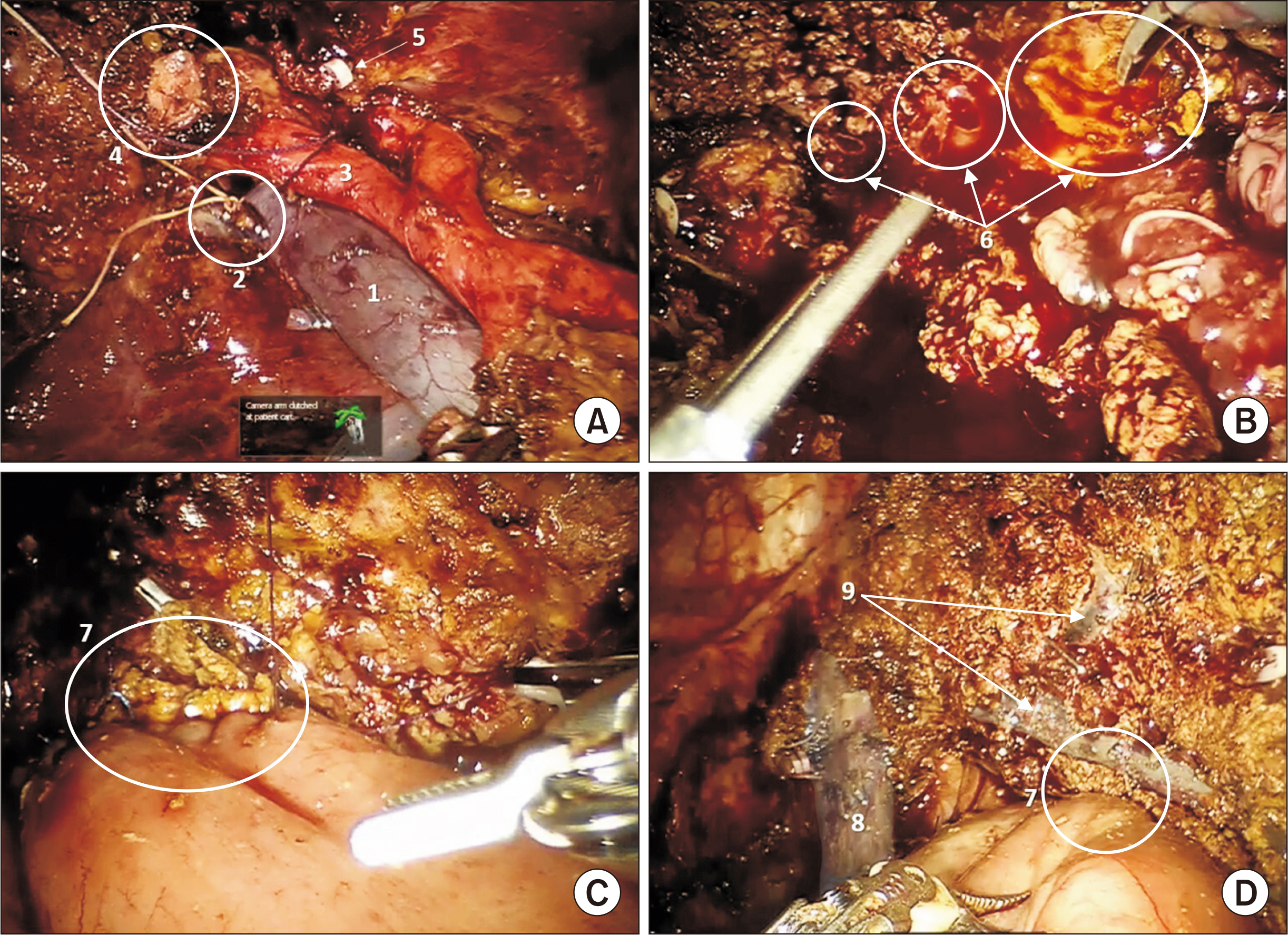
Figure
Reference
-
References
1. Hu HJ, Wu ZR, Jin YW, Ma WJ, Yang Q, Wang JK, et al. 2019; Minimally invasive surgery for hilar cholangiocarcinoma: state of art and future perspectives. ANZ J Surg. 89:476–480. DOI: 10.1111/ans.14765. PMID: 30136376.
Article2. Franken LC, van der Poel MJ, Latenstein AEJ, Zwart MJ, Roos E, Busch OR, et al. 2019; Minimally invasive surgery for perihilar cholangiocarcinoma: a systematic review. J Robot Surg. 13:717–727. DOI: 10.1007/s11701-019-00964-9. PMID: 31049774. PMCID: PMC6842355.
Article3. Feng F, Cao X, Liu X, Qin J, Zhang S, Li Q, et al. 2019; Laparoscopic resection for Bismuth type III and IV hilar cholangiocarcinoma: How to improve the radicality without direct palpation. J Surg Oncol. 120:1379–1385. DOI: 10.1002/jso.25739. PMID: 31691290.
Article4. Ratti F, Fiorentini G, Cipriani F, Catena M, Paganelli M, Aldrighetti L. 2020; Perihilar cholangiocarcinoma: are we ready to step towards minimally invasiveness? Updates Surg. 72:423–433. DOI: 10.1007/s13304-020-00752-3. PMID: 32221907.
Article5. Zhang Y, Dou C, Wu W, Liu J, Jin L, Hu Z, et al. 2020; Total laparoscopic versus open radical resection for hilar cholangiocarcinoma. Surg Endosc. 34:4382–4387. DOI: 10.1007/s00464-019-07211-0. PMID: 31664578.
Article6. Wang M, Qin T, Zhang H, Li J, Deng X, Zhang Y, et al. 2023; Laparoscopic versus open surgery for perihilar cholangiocarcinoma: a multicenter propensity score analysis of short- term outcomes. BMC Cancer. 23:394. DOI: 10.1186/s12885-023-10783-9. PMID: 37138243. PMCID: PMC10157952.
Article7. Jingdong L, Yongfu X, Yang G, Jian X, Xujian H, Jianhua L, et al. 2021; Minimally invasive surgery for hilar cholangiocarcinoma: a multicenter retrospective analysis of 158 patients. Surg Endosc. 35:6612–6622. DOI: 10.1007/s00464-020-08161-8. PMID: 33258033.
Article8. Qin T, Wang M, Zhang H, Li J, Deng X, Zhang Y, et al. Minimally Invasive Pancreas Treatment Group in the Pancreatic Disease Branch of China's International Exchange and Promotion Association for Medicine and Healthcare. 2023; The long-term outcome of laparoscopic resection for perihilar cholangiocarcinoma compared with the open approach: a real-world multicentric analysis. Ann Surg Oncol. 30:1366–1378. DOI: 10.1245/s10434-022-12647-1. PMID: 36273058. PMCID: PMC9589740.
Article9. Lippert T, Ross S, Pattilachan T, Christodoulou M, Gratsianskiy D, Rosemurgy A, et al. 2024; Initial clinical outcomes of robotic resection for perihilar cholangiocarcinoma: Is it safe and effective? J Surg Oncol. 130:102–108. DOI: 10.1002/jso.27676. PMID: 38739865.
Article10. Sucandy I, Marques HP, Lippert T, Magistri P, Coelho JS, Ross SB, et al. 2024; Clinical outcomes of robotic resection for perihilar cholangiocarcinoma: a first, multicenter, trans-atlantic, expert-center, collaborative study. Ann Surg Oncol. 31:81–89. DOI: 10.1245/s10434-023-14307-4. PMID: 37718337.
Article11. Efanov M, Alikhanov R, Zamanov E, Melekhina O, Kulezneva Y, Kazakov I, et al. 2021; Combining E-PASS model and disease specific risk factors to predict severe morbidity after liver and bile duct resection for perihilar cholangiocarcinoma. HPB (Oxford). 23:387–393. DOI: 10.1016/j.hpb.2020.07.009. PMID: 32792305.
Article12. Nakanishi Y, Tsuchikawa T, Okamura K, Nakamura T, Tamoto E, Noji T, et al. 2016; Risk factors for a high Comprehensive Complication Index score after major hepatectomy for biliary cancer: a study of 229 patients at a single institution. HPB (Oxford). 18:735–741. DOI: 10.1016/j.hpb.2016.06.013. PMID: 27593590. PMCID: PMC5011079.
Article13. Haga Y, Miyamoto A, Wada Y, Takami Y, Takeuchi H. 2016; Value of E-PASS models for predicting postoperative morbidity and mortality in resection of perihilar cholangiocarcinoma and gallbladder carcinoma. HPB (Oxford). 18:271–278. DOI: 10.1016/j.hpb.2015.09.001. PMID: 27017167. PMCID: PMC4814599.
Article14. Andrade C. 2020; Mean difference, standardized mean difference (SMD), and their use in meta-analysis: as simple as it gets. J Clin Psychiatry. 81:20f13681. DOI: 10.4088/JCP.20f13681.
Article15. Liu QD, Chen JZ, Xu XY, Zhang T, Zhou NX. 2012; Incidence of port-site metastasis after undergoing robotic surgery for biliary malignancies. World J Gastroenterol. 18:5695–5701. DOI: 10.3748/wjg.v18.i40.5695. PMID: 23155309. PMCID: PMC3484337.
Article16. Xu Y, Wang H, Ji W, Tang M, Li H, Leng J, et al. 2016; Robotic radical resection for hilar cholangiocarcinoma: perioperative and long-term outcomes of an initial series. Surg Endosc. 30:3060–3070. DOI: 10.1007/s00464-016-4925-7. PMID: 27194255.
Article17. Magistri P, Pang NQ, Guidetti C, Caracciolo D, Odorizzi R, Catellani B, et al. 2023; Robotic approach for perihilar cholangiocarcinoma: from Bismuth 1 to vascular resection. Eur J Surg Oncol. 49:107002. DOI: 10.1016/j.ejso.2023.107002. PMID: 37599146.
Article18. Cillo U, D'Amico FE, Furlanetto A, Perin L, Gringeri E. 2021; Robotic hepatectomy and biliary reconstruction for perihilar cholangiocarcinoma: a pioneer western case series. Updates Surg. 73:999–1006. DOI: 10.1007/s13304-021-01041-3. PMID: 33861401. PMCID: PMC8184707.
Article19. Huang XT, Xie JZ, Cai JP, Chen W, Chen LH, Liang LJ, et al. 2023; Evaluation of the short-term outcomes of robotic-assisted radical resection for perihilar cholangiocarcinoma: a propensity-scored matching analysis. Gastroenterol Rep (Oxf). 11:goad018. DOI: 10.1093/gastro/goad018. PMID: 37051578. PMCID: PMC10085544.
Article20. Liu J, Dou C, Chen J, Lu Y, Liang L, Wei F, et al. 2024; Evaluation of the outcomes of biliary-enteric reconstruction in robotic radical resection of hilar cholangiocarcinoma: a single-center propensity score matching analysis. Sci Rep. 14:14836. DOI: 10.1038/s41598-024-65875-8. PMID: 38937559. PMCID: PMC11211424.
Article21. Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. 2013; Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg. 258:129–140. DOI: 10.1097/SLA.0b013e3182708b57. PMID: 23059502.22. Donati M, Stavrou GA, Oldhafer KJ. 2011; Laparoscopic resections for hilar cholangiocarcinomas: a critical appraisal. Dig Surg. 28:277–278. author reply 279–280. DOI: 10.1159/000329583. PMID: 21778727.
Article23. Nagino M. 2022; Perihilar cholangiocarcinoma: a surgeon's perspective. iLIVER. 1:12–24. DOI: 10.1016/j.iliver.2022.03.004.
Article24. Xiong J, Nunes QM, Huang W, Wei A, Ke N, Mai G, et al. 2015; Major hepatectomy in Bismuth types I and II hilar cholangiocarcinoma. J Surg Res. 194:194–201. DOI: 10.1016/j.jss.2014.10.029. PMID: 25454973.
Article25. Jena SS, Mehta NN, Nundy S. 2023; Surgical management of hilar cholangiocarcinoma: controversies and recommendations. Ann Hepatobiliary Pancreat Surg. 27:227–240. DOI: 10.14701/ahbps.23-028. PMID: 37408334. PMCID: PMC10472117.
Article26. Li J, Xiong Y, Yang G, Zhang L, Riaz M, Xu J, et al. 2021; Complete laparoscopic radical resection of hilar cholangiocarcinoma: technical aspects and long-term results from a single center. Wideochir Inne Tech Maloinwazyjne. 16:62–75. DOI: 10.5114/wiitm.2020.97363. PMID: 33786118. PMCID: PMC7991938.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Applications of propensity score matching: a case series of articles published in Annals of Coloproctology
- Gallbladder neck cancer and perihilar cholangiocarcinoma - siblings, cousins or look alikes?
- Short-term and Long-term Clinical Outcomes of Combined Caudate Lobectomy for Intrahepatic Cholangiocarcinoma Involving the Hepatic Hilus: A Propensity Score Analysis
- Comparative analysis of postoperative outcomes of single-incision cholecystectomy: Propensity score matching of robotic surgery using the da Vinci SP system and da Vinci Xi system vs. laparoscopic surgery
- Spontaneous rupture of intrahepatic bile duct following portal vein embolization in a patient with perihilar cholangiocarcinoma: a case of successful curative resection