Clin Exp Otorhinolaryngol.
2021 Feb;14(1):76-81. 10.21053/ceo.2019.01382.
MicroRNAs Related to Cognitive Impairment After Hearing Loss
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Chung-Ang University College of Medicine, Seoul, Korea
- 2Department of Otorhinolaryngology, Gyeongsang National University Changwon Hospital, Gyeongsang National University College of Medicine, Changwon, Korea
- 3Department of Biochemistry, Chonnam National University Medical School, Hwasun, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2512884
- DOI: http://doi.org/10.21053/ceo.2019.01382
Abstract
Objectives
. Our research group has previously demonstrated that hearing loss might be a risk factor for synaptic loss within the hippocampus and impairment of cognition using an animal model of Alzheimer disease. In this study, after inducing hearing loss in a rat model of Alzheimer disease, the associations of various microRNAs (miRNAs) with cognitive impairment were investigated.
Methods
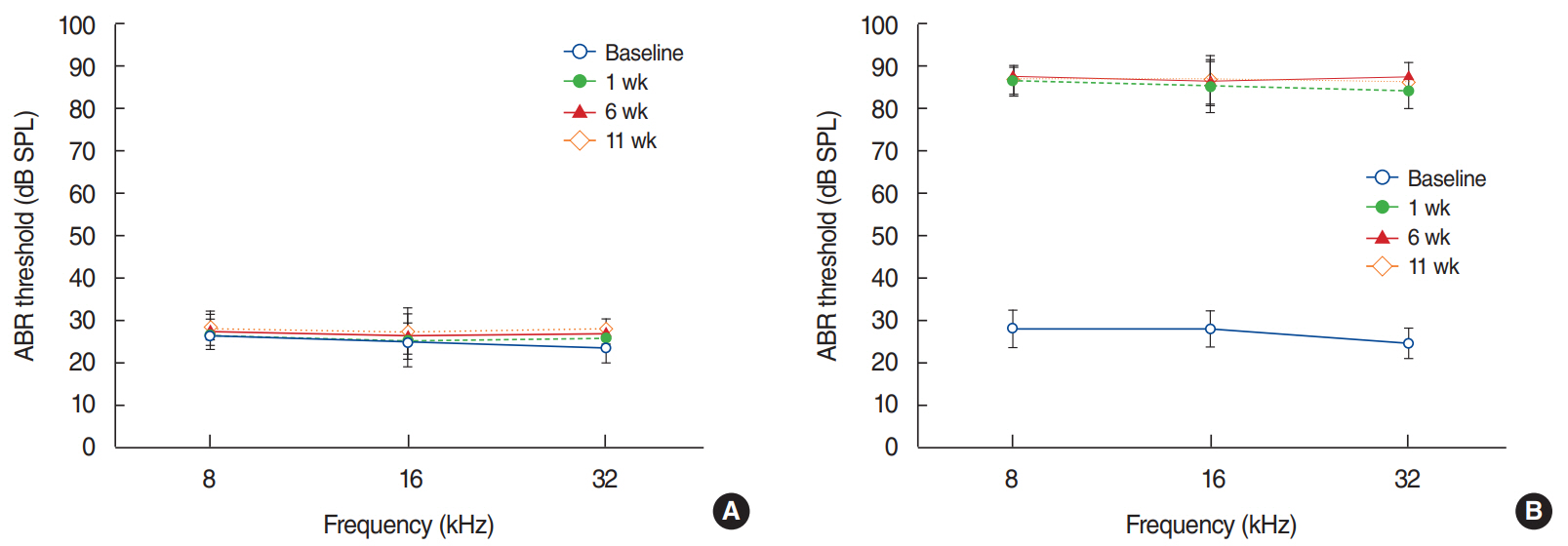
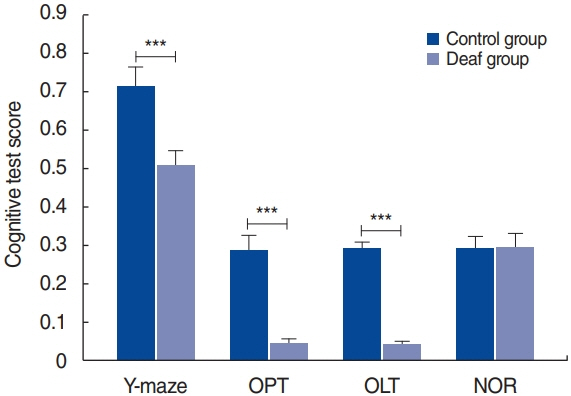
. Rats were divided randomly into two experimental groups: the control group, which underwent sham surgery and subthreshold amyloid-β infusion and the deaf group, which underwent bilateral cochlear ablation and subthreshold amyloid-β infusion. All rats completed several cognitive function assessments 11 weeks after surgery, including the object-in-place task (OPT), the novel object recognition task (NOR), the object location task (OLT), and the Y-maze test. After the rats completed these tests, hippocampus tissue samples were assessed using miRNA microarrays. Candidate miRNAs were selected based on the results and then validated with quantitative reverse transcriptionpolymerase chain reaction (qRT-PCR) analyses.
Results
. The deaf group showed considerably lower scores on the OPT, OLT, and Y-maze test than the control group. The microarray analysis revealed that miR-29b-3p, -30e-5p, -153-3p, -376a-3p, -598-3p, -652-5p, and -873-3p were candidate miRNAs, and qRT-PCR showed significantly higher levels of miR-376a-3p and miR-598-3p in the deaf group.
Conclusion
. These results indicate that miR-376a-3p and miR-598-3p were related to cognitive impairment after hearing loss.
Keyword
Figure
Cited by 1 articles
-
The Use of MicroRNAs for the Early Diagnosis of Dementia in Patients Affected by Hearing Loss
Cha Dong Yeo, Moo Kyun Park
Clin Exp Otorhinolaryngol. 2021;14(1):3-4. doi: 10.21053/ceo.2021.00017.
Reference
-
1. GBD 2016 Dementia Collaborators. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019; Jan. 18(1):88–106.2. Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E. Alzheimer’s disease. Lancet. 2011; Mar. 377(9770):1019–31.
Article3. Cao J, Hou J, Ping J, Cai D. Advances in developing novel therapeutic strategies for Alzheimer’s disease. Mol Neurodegener. 2018; Dec. 13(1):64.
Article4. Chang M, Kim HJ, Mook-Jung I, Oh SH. Hearing loss as a risk factor for cognitive impairment and loss of synapses in the hippocampus. Behav Brain Res. 2019; Oct. 372:112069.
Article5. Tran TT, Srivareerat M, Alkadhi KA. Chronic psychosocial stress triggers cognitive impairment in a novel at-risk model of Alzheimer’s disease. Neurobiol Dis. 2010; Mar. 37(3):756–63.
Article6. Hollins SL, Cairns MJ. MicroRNA: small RNA mediators of the brains genomic response to environmental stress. Prog Neurobiol. 2016; Aug. 143:61–81.
Article7. Campbell K, Booth SA. MicroRNA in neurodegenerative drug discovery: the way forward? Expert Opin Drug Discov. 2015; Jan. 10(1):9–16.
Article8. Esteller M. Non-coding RNAs in human disease. Nat Rev Genet. 2011; Nov. 12(12):861–74.
Article9. Gebert LF, Rebhan MA, Crivelli SE, Denzler R, Stoffel M, Hall J. Miravirsen (SPC3649) can inhibit the biogenesis of miR-122. Nucleic Acids Res. 2014; Jan. 42(1):609–21.
Article10. Huang Z, Chen W, Du Y, Guo Q, Mao Y, Zhou X, et al. Serum miR-16 as a potential biomarker for human cancer diagnosis: results from a large-scale population. J Cancer Res Clin Oncol. 2019; Mar. 145(3):787–96.
Article11. Ng PC, Chan KY, Yuen TP, Sit T, Lam HS, Leung KT, et al. Plasma miR-1290 is a novel and specific biomarker for early diagnosis of necrotizing enterocolitis-biomarker discovery with prospective cohort evaluation. J Pediatr. 2019; Feb. 205:83–90. e10.
Article12. Parizadeh SM, Jafarzadeh-Esfehani R, Ghandehari M, Goldani F, Parizadeh SM, Hassanian SM, et al. MicroRNAs as potential diagnostic and prognostic biomarkers in hepatocellular carcinoma. Curr Drug Targets. 2019; 20(11):1129–40.
Article13. Rezayi M, Farjami Z, Hosseini ZS, Ebrahimi N, Abouzari-Lotf E. MicroRNA-based biosensors for early detection of cancers. Curr Pharm Des. 2018; 24(39):4675–80.
Article14. Weis A, Marquart L, Calvopina DA, Genz B, Ramm GA, Skoien R. Serum microRNAs as biomarkers in hepatitis C: preliminary evidence of a microRNA panel for the diagnosis of hepatocellular carcinoma. Int J Mol Sci. 2019; Feb. 20(4):864.
Article15. Mun SK, Han KH, Baek JT, Ahn SW, Cho HS, Chang MY. Losartan prevents maladaptive auditory-somatosensory plasticity after hearing loss via transforming growth factor-β signaling suppression. Clin Exp Otorhinolaryngol. 2019; Feb. 12(1):33–9.
Article16. Chang MY, Park S, Choi JJ, Kim YK, Suh MW, Lee JH, et al. MicroRNAs 218a-5p, 219a-5p, and 221-3p regulate vestibular compensation. Sci Rep. 2017; Aug. 7(1):8701.
Article17. Paxinos G, Watson C. The rat brain in stereotaxic coordinates. Burlington (MA): Academic Press;2006.18. Gallacher J, Ilubaera V, Ben-Shlomo Y, Bayer A, Fish M, Babisch W, et al. Auditory threshold, phonologic demand, and incident dementia. Neurology. 2012; Oct. 79(15):1583–90.
Article19. Kiely KM, Gopinath B, Mitchell P, Luszcz M, Anstey KJ. Cognitive, health, and sociodemographic predictors of longitudinal decline in hearing acuity among older adults. J Gerontol A Biol Sci Med Sci. 2012; Sep. 67(9):997–1003.
Article20. Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. Arch Neurol. 2011; Feb. 68(2):214–20.
Article21. Lin FR, Yaffe K, Xia J, Xue QL, Harris TB, Purchase-Helzner E, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013; Feb. 173(4):293–9.
Article22. Brennan S, Keon M, Liu B, Su Z, Saksena NK. Panoramic visualization of circulating microRNAs across neurodegenerative diseases in humans. Mol Neurobiol. 2019; 56(11):7380–407.
Article23. Boese AS, Saba R, Campbell K, Majer A, Medina S, Burton L, et al. MicroRNA abundance is altered in synaptoneurosomes during prion disease. Mol Cell Neurosci. 2016; Mar. 71:13–24.
Article24. Huang Q, Wang C, Hou Z, Wang G, Lv J, Wang H, et al. Serum microRNA-376 family as diagnostic and prognostic markers in human gliomas. Cancer Biomark. 2017; 19(2):137–44.
Article25. Osei J, Kelly W, Toffolo K, Donahue K, Levy B, Bard J, et al. Thymosin beta 4 induces significant changes in the plasma miRNA profile following severe traumatic brain injury in the rat lateral fluid percussion injury model. Expert Opin Biol Ther. 2018; Jul. 18(sup1):159–64.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Hearing Difficulty, Masticatory Difficulty, and Risk of Cognitive Impairment: Analysis of the Korean Longitudinal Study of Aging Data (2006-2020)
- Association between age-related hearing loss and cognitive decline
- The Effect of Visual and Hearing Impairment on Depression and Cognitive Function in Community-dwelling Elderly: The Korean Longitudinal Study of Aging 2008
- Hearing Screening for Older Adults With Cognitive Impairment: A Systematic Review
- Influence of Cochlear Implantation on Cognitive Function in Elderly Patients