J Stroke.
2021 Jan;23(1):91-102. 10.5853/jos.2020.01788.
Safety and Angiographic Efficacy of Intra-Arterial Fibrinolytics as Adjunct to Mechanical Thrombectomy: Results from the INFINITY Registry
- Affiliations
-
- 1a University Institute of Diagnostic and Interventional Neuroradiology, University Hospital Bern, Inselspital, University of Bern, Bern, Switzerland
- 2University Institute of Diagnostic and Interventional and Pediatric Radiology, University Hospital Bern, Inselspital, University of Bern, Bern, Switzerland
- 3Institute for Diagnostic and Interventional Radiology, Faculty of Medicine and University Hospital Cologne, Cologne, Germany
- 4Department of Neurology, University Hospital Bern, Inselspital, University of Bern, Bern, Switzerland
- 5Department of Interventional Neuroradiology, University Hospital Strasbourg, Strasbourg, France
- 6Department of Neuroradiology, University Hospital Göttingen, Göttingen, Germany
- 7Department of Neuroradiology, University Hospital Basel, Basel, Switzerland
- 8Department of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 9Department of Neuroradiology, University Hospital Essen, Essen, Germany
- 10Department of Neuroradiology, University Hospital Helsinki, Helsinki, Finland
- 11Department of Radiology, University Hospital Rostock, Rostock, Germany
- 12Department of Neuroradiology, University Hospital Knappschaftskrankenhaus Bochum, Bochum, Germany
- 13Institute of Clinical Radiology University Hospital of Muenster, Muenster, Germany
- 14Department of Radiology, University Hospital Munich, Ludwig Maximilian University, Munich, Germany
- 15Department of Neurology, University Hospital Helsinki, Helsinki, Finland
- 16Department of Neuroradiology, University Hospital Bonn, Bonn, Germany
- KMID: 2512358
- DOI: http://doi.org/10.5853/jos.2020.01788
Abstract
- Background and Purpose
Data on safety and efficacy of intra-arterial (IA) fibrinolytics as adjunct to mechanical thrombectomy (MT) are sparse.
Methods
INtra-arterial FIbriNolytics In ThrombectomY (INFINITY) is a retrospective multi-center observational registry of consecutive patients with anterior circulation large-vessel occlusion ischemic stroke treated with MT and adjunctive administration of IA fibrinolytics (alteplase [tissue plasminogen activator, tPA] or urokinase [UK]) at 10 European centers. Primary outcome was the occurrence of symptomatic intracranial hemorrhage (sICH) according to the European Cooperative Acute Stroke Study II definition. Secondary outcomes were mortality and modified Rankin Scale (mRS) scores at 3 months.
Results
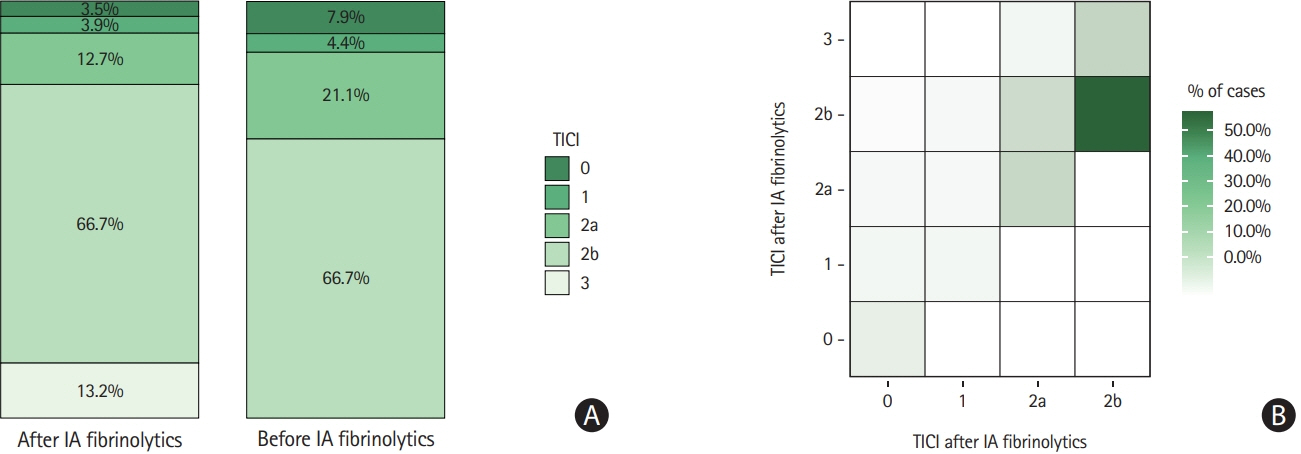
Of 5,612 patients screened, 311 (median age, 74 years; 44.1% female) received additional IA after or during MT (194 MT+IA tPA, 117 MT+IA UK). IA fibrinolytics were mostly administered for rescue of thrombolysis in cerebral infarction (TICI) 0-2b after MT (80.4%, 250/311). sICH occurred in 27 of 308 patients (8.8%), with an increased risk in patients with initial TICI0/1 (adjusted odds ratio [aOR], 2.3; 95% confidence interval [CI], 1.1 to 5.0 per TICI grade decrease) or in those with intracranial internal carotid artery occlusions (aOR, 3.7; 95% CI, 1.2 to 12.5). In patients with attempted rescue of TICI0-2b and available angiographic follow-up, 116 of 228 patients (50.9%) showed any angiographic reperfusion improvement after IA fibrinolytics, which was associated with mRS ≤2 (aOR, 3.1; 95% CI, 1.4 to 6.9).
Conclusions
Administration of IA fibrinolytics as adjunct to MT is performed rarely, but can improve reperfusion, which is associated with better outcomes. Despite a selection bias, an increased risk of sICH seems possible, which underlines the importance of careful patient selection.
Keyword
Figure
Cited by 1 articles
-
Intra-Arterial Thrombolysis to Improve Final Thrombolysis in Cerebral Infarction Score after Thrombectomy: A Case-Series Analysis
Antonio De Mase, Paolo Candelaresi, Emanuele Spina, Flavio Giordano, Stefano Barbato, Giovanna Servillo, Elio Prestipino, Alessandra Fasolino, Gianluigi Guarnieri, Giuseppe Leone, Massimo Muto, Mario Muto, Vincenzo Andreone
Neurointervention. 2023;18(2):123-128. doi: 10.5469/neuroint.2023.00052.
Reference
-
References
1. Rizvi A, Seyedsaadat SM, Murad MH, Brinjikji W, Fitzgerald ST, Kadirvel R, et al. Redefining 'success': a systematic review and meta-analysis comparing outcomes between incomplete and complete revascularization. J Neurointerv Surg. 2019; 11:9–13.
Article2. Liebeskind DS, Bracard S, Guillemin F, Jahan R, Jovin TG, Majoie CB, et al. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg. 2019; 11:433–438.
Article3. Kaesmacher J, Dobrocky T, Heldner MR, Bellwald S, Mosimann PJ, Mordasini P, et al. Systematic review and metaanalysis on outcome differences among patients with TICI2b versus TICI3 reperfusions: success revisited. J Neurol Neurosurg Psychiatry. 2018; 89:910–917.
Article4. Kaesmacher J, Gralla J, Mosimann PJ, Zibold F, Heldner MR, Piechowiak E, et al. Reasons for reperfusion failures in stentretriever-based thrombectomy: registry analysis and proposal of a classification system. AJNR Am J Neuroradiol. 2018; 39:1848–1853.
Article5. Leischner H, Flottmann F, Hanning U, Broocks G, Faizy TD, Deb-Chatterji M, et al. Reasons for failed endovascular recanalization attempts in stroke patients. J Neurointerv Surg. 2019; 11:439–442.
Article6. Hill MD, Goyal M, Menon BK, Nogueira RG, McTaggart RA, Demchuk AM, et al. Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): a multicentre, double-blind, randomised controlled trial. Lancet. 2020; 395:878–887.7. Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Yoo J. Stenting as a rescue treatment after failure of mechanical thrombectomy for anterior circulation large artery occlusion. Stroke. 2016; 47:2360–2363.
Article8. Meyer L, Fiehler J, Thomalla G, Krause LU, Lowens S, Rothaupt J, et al. Intracranial stenting after failed thrombectomy in patients with moderately severe stroke: a multicenter cohort study. Front Neurol. 2020; 11:97.
Article9. Chang Y, Kim BM, Bang OY, Baek JH, Heo JH, Nam HS, et al. Rescue stenting for failed mechanical thrombectomy in acute ischemic stroke: a multicenter experience. Stroke. 2018; 49:958–964.10. Grossberg JA, Rebello LC, Haussen DC, Bouslama M, Bowen M, Barreira CM, et al. Beyond large vessel occlusion strokes: distal occlusion thrombectomy. Stroke. 2018; 49:1662–1668.11. Goyal M, Ospel JM, Menon BK, Hill MD. MeVO: the next frontier? J Neurointerv Surg. 2020; 12:545–547.
Article12. Kaesmacher J, Maegerlein C, Zibold F, Wunderlich S, Zimmer C, Friedrich B. Improving mTICI2b reperfusion to mTICI2c/3 reperfusions: a retrospective observational study assessing technical feasibility, safety and clinical efficacy. Eur Radiol. 2018; 28:274–282.
Article13. Yang M, Huo X, Gao F, Wang A, Ma N, Shi H, et al. Low-dose rescue tirofiban in mechanical thrombectomy for acute cerebral large-artery occlusion. Eur J Neurol. 2020; 27:1056–1061.
Article14. Zaidi SF, Castonguay AC, Jumaa MA, Malisch TW, Linfante I, Marden FA, et al. Intraarterial thrombolysis as rescue therapy for large vessel occlusions. Stroke. 2019; 50:1003–1006.
Article15. Anadani M, Ajinkya S, Alawieh A, Vargas J, Chatterjee A, Turk A, et al. Intra-arterial tissue plasminogen activator is a safe rescue therapy with mechanical thrombectomy. World Neurosurg. 2019; 123:e604–e608.
Article16. Kaesmacher J, Bellwald S, Dobrocky T, Meinel TR, Piechowiak EI, Goeldlin M, et al. Safety and efficacy of intra-arterial urokinase after failed, unsuccessful, or incomplete mechanical thrombectomy in anterior circulation large-vessel occlusion stroke. JAMA Neurol. 2020; 77:318–326.
Article17. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article18. Kellert L, Wollenweber FA, Thomalla G, Nolte CH, Fiehler J, Ringleb PA, et al. Thrombolysis management in thrombectomy patients: real-life data from German stroke centres. Eur Stroke J. 2017; 2:356–360.
Article19. Heiferman DM, Li DD, Pecoraro NC, Smolenski AM, Tsimpas A, Ashley WW Jr. Intra-arterial alteplase thrombolysis during mechanical thrombectomy for acute ischemic stroke. J Stroke Cerebrovasc Dis. 2017; 26:3004–3008.
Article20. Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. 1998; 352:1245–1251.21. Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934; 26:404–413.
Article22. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after largevessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article23. Castonguay AC, Jumaa MA, Zaidat OO, Haussen DC, Jadhav A, Salahuddin H, et al. Insights into intra-arterial thrombolysis in the modern era of mechanical thrombectomy. Front Neurol. 2019; 10:1195.
Article24. Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016; 15:1138–1147.
Article25. Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999; 282:2003–2011.26. Lee M, Hong KS, Saver JL. Efficacy of intra-arterial fibrinolysis for acute ischemic stroke: meta-analysis of randomized controlled trials. Stroke. 2010; 41:932–937.27. Cappellari M, Mangiafico S, Saia V, Pracucci G, Nappini S, Nencini P, et al. IER-SICH nomogram to predict symptomatic intracerebral hemorrhage after thrombectomy for stroke. Stroke. 2019; 50:909–916.
Article28. Lee YB, Yoon W, Lee YY, Kim SK, Baek BH, Kim JT, et al. Predictors and impact of hemorrhagic transformations after endovascular thrombectomy in patients with acute large vessel occlusions. J Neurointerv Surg. 2019; 11:469–473.
Article29. Kaesmacher J, Kaesmacher M, Maegerlein C, Zimmer C, Gersing AS, Wunderlich S, et al. Hemorrhagic transformations after thrombectomy: risk factors and clinical relevance. Cerebrovasc Dis. 2017; 43:294–304.
Article30. Hassan AE, Abd-Allah F, Chaudhry SA, Adil MM, Rostambeigi N, Qureshi AI. A critical analysis of intra-arterial thrombolytic doses in acute ischemic stroke treatment. Neurocrit Care. 2014; 21:119–123.
Article31. Kadir RRA, Bayraktutan U. Urokinase plasminogen activator: a potential thrombolytic agent for ischaemic stroke. Cell Mol Neurobiol. 2020; 40:347–355.
Article32. Tan Q, Chen Q, Niu Y, Feng Z, Li L, Tao Y, et al. Urokinase, a promising candidate for fibrinolytic therapy for intracerebral hemorrhage. J Neurosurg. 2017; 126:548–557.
Article33. Renú A, Blasco J, Millán M, Martí-Fàbregas J, Cardona P, Oleaga L, et al. The chemical optimization of cerebral embolectomy trial: study protocol. Int J Stroke. 2019; Dec. 18. [Epub]. https://doi.org/10.1177/1747493019895656.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intra-Arterial Thrombolysis to Improve Final Thrombolysis in Cerebral Infarction Score after Thrombectomy: A Case-Series Analysis
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Adjuvant Tirofiban Injection Through Deployed Solitaire Stent As a Rescue Technique After failed Mechanical Thrombectomy in Acute Stroke
- Paradigm Shift in Intra-Arterial Mechanical Thrombectomy for Acute Ischemic Stroke : A Review of Randomized Controlled Trials after 2015
- Mechanical Solitaire Thrombectomy with Low-Dose Booster Tirofiban Injection