Cancer Res Treat.
2021 Jan;53(1):223-232. 10.4143/crt.2020.546.
Adherence to Cancer Prevention Guidelines and Endometrial Cancer Risk: Evidence from a Systematic Review and Dose-Response Meta-analysis of Prospective Studies
- Affiliations
-
- 1Department of Clinical Epidemiology, Shengjing Hospital of China Medical University, Shenyang, China
- 2Clinical Research Center, Shengjing Hospital of China Medical University, Shenyang, China
- 3Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang, China
- KMID: 2510664
- DOI: http://doi.org/10.4143/crt.2020.546
Abstract
- Purpose
The evidence of adherence to cancer prevention guidelines and endometrial cancer (EC) risk has been limited and controversial. This study summarizes and quantifies the relationship between adherence to cancer prevention guidelines and EC risk.
Materials and Methods
The online databases PubMed, Web of Science, and EMBASE were searched for relevant publications up to June 2, 2020. This study had been registered at PROSPERO. The registration number is CRD42020149966. Study quality evaluation was performed based on the Newcastle-Ottawa Scale. The I2 statistic was used to estimate heterogeneity among studies. Egger’s and Begg’s tests assessed potential publication bias. Summary hazard ratios (HRs) and 95% confidence intervals (CIs) for the relationship between adherence to cancer prevention guidelines score was assigned to participants by summarizing individual scores for each lifestyle-related factor. The scores ranged from least healthy (0) to most healthy (20) and the EC risk was calculated using a randomeffects model.
Results
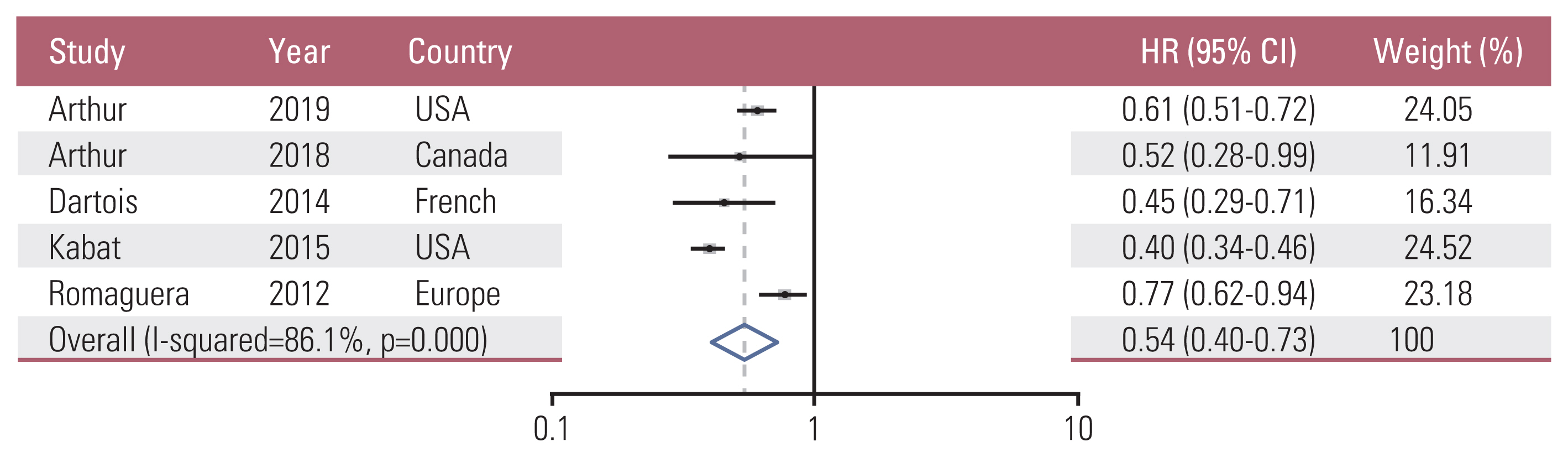
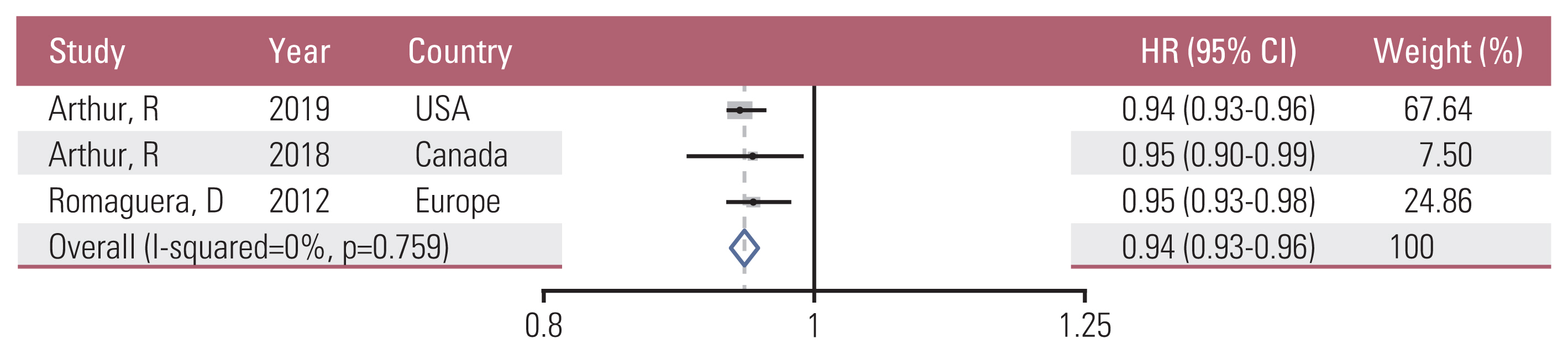
Five prospective studies (four cohort studies and one case‑cohort study) consisted of 4,470 EC cases, where 597,047 participants were included. Four studies had a low bias risk and one study had a high bias risk. Summary EC HR for the highest vs. lowest score of adherence to cancer prevention guidelines was 0.54 (95% CI, 0.40 to 0.73) and had a high heterogeneity (I2=86.1%). For the dose-response analysis, an increment of 1 significantly reduced the risk of EC by 6%. No significant publication bias was detected.
Conclusion
This study suggested that adherence to cancer prevention guidelines was negatively related to EC risk.
Keyword
Figure
Reference
-
References
1. Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010; 46:765–81.
Article2. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.
Article3. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.
Article4. Sorosky JI. Endometrial cancer. Obstet Gynecol. 2012; 120:383–97.
Article5. Constantine GD, Kessler G, Graham S, Goldstein SR. Increased incidence of endometrial cancer following the Women’s Health Initiative: an assessment of risk factors. J Womens Health (Larchmt). 2019; 28:237–43.
Article6. Avgerinos KI, Spyrou N, Mantzoros CS, Dalamaga M. Obesity and cancer risk: emerging biological mechanisms and perspectives. Metabolism. 2019; 92:121–35.
Article7. Linkov F, Goughnour SL, Adambekov S, Edwards RP, Donnellan N, Bovbjerg DH. Lifestyle interventions to reduce the risk of obesity-associated gynecologic malignancies: a focus on endometrial cancer. Berger M, Klopp A, Lu K, editors. Focus on gynecologic malignancies. Energy balance and cancer. 13. Cham: Springer;2018. p. 137–65.
Article8. Gierach GL, Chang SC, Brinton LA, Lacey JV Jr, Hollenbeck AR, Schatzkin A, et al. Physical activity, sedentary behavior, and endometrial cancer risk in the NIH-AARP Diet and Health Study. Int J Cancer. 2009; 124:2139–47.
Article9. Kawachi A, Shimazu T, Budhathoki S, Sawada N, Yamaji T, Iwasaki M, et al. Association of BMI and height with the risk of endometrial cancer, overall and by histological subtype: a population-based prospective cohort study in Japan. Eur J Cancer Prev. 2019; 28:196–202.
Article10. Dunneram Y, Greenwood DC, Cade JE. Diet, menopause and the risk of ovarian, endometrial and breast cancer. Proc Nutr Soc. 2019; 78:438–48.
Article11. Pronk NP, Anderson LH, Crain AL, Martinson BC, O’Connor PJ, Sherwood NE, et al. Meeting recommendations for multiple healthy lifestyle factors: prevalence, clustering, and predictors among adolescent, adult, and senior health plan members. Am J Prev Med. 2004; 27:25–33.12. Arthur R, Brasky TM, Crane TE, Felix AS, Kaunitz AM, Shadyab AH, et al. Associations of a healthy lifestyle index with the risks of endometrial and ovarian cancer among women in the Women’s Health Initiative Study. Am J Epidemiol. 2019; 188:261–73.
Article13. Arthur R, Kirsh VA, Kreiger N, Rohan T. A healthy lifestyle index and its association with risk of breast, endometrial, and ovarian cancer among Canadian women. Cancer Causes Control. 2018; 29:485–93.
Article14. Dartois L, Fagherazzi G, Boutron-Ruault MC, Mesrine S, Clavel-Chapelon F. Association between five lifestyle habits and cancer risk: results from the E3N cohort. Cancer Prev Res (Phila). 2014; 7:516–25.
Article15. Thomson CA, McCullough ML, Wertheim BC, Chlebowski RT, Martinez ME, Stefanick ML, et al. Nutrition and physical activity cancer prevention guidelines, cancer risk, and mortality in the women’s health initiative. Cancer Prev Res (Phila). 2014; 7:42–53.
Article16. Kabat GC, Matthews CE, Kamensky V, Hollenbeck AR, Rohan TE. Adherence to cancer prevention guidelines and cancer incidence, cancer mortality, and total mortality: a prospective cohort study. Am J Clin Nutr. 2015; 101:558–69.
Article17. Romaguera D, Vergnaud AC, Peeters PH, van Gils CH, Chan DS, Ferrari P, et al. Is concordance with World Cancer Research Fund/American Institute for Cancer Research guidelines for cancer prevention related to subsequent risk of cancer? Results from the EPIC study. Am J Clin Nutr. 2012; 96:150–63.
Article18. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: University of Ottawa;2013.19. Gong TT, Wu QJ, Lin B, Ruan SK, Kushima M, Takimoto M. Observational studies on the association between post-diagnostic metformin use and survival in ovarian cancer: a systematic review and meta-analysis. Front Oncol. 2019; 9:458.
Article20. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986; 7:177–88.
Article21. Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992; 135:1301–9.
Article22. Chang SC, Lacey JV Jr, Brinton LA, Hartge P, Adams K, Mouw T, et al. Lifetime weight history and endometrial cancer risk by type of menopausal hormone use in the NIH-AARP diet and health study. Cancer Epidemiol Biomarkers Prev. 2007; 16:723–30.
Article23. Lee SC, Kaunitz AM, Sanchez-Ramos L, Rhatigan RM. The oncogenic potential of endometrial polyps: a systematic review and meta-analysis. Obstet Gynecol. 2010; 116:1197–205.
Article24. Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012; 62:30–67.
Article25. Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, McTiernan A, et al. American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2006; 56:254–81.
Article26. Giovannucci E. Insulin, insulin-like growth factors and colon cancer: a review of the evidence. J Nutr. 2001; 131:3109S–20S.
Article27. Lee C, Kim SJ, Na JY, Park CS, Lee SY, Kim IH, et al. Alterations in promoter usage and expression levels of insulin-like growth factor-II and H19 genes in cervical and endometrial cancer. Cancer Res Treat. 2003; 35:314–22.
Article28. Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008; 371:569–78.
Article29. Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Manson JE, Li J, et al. A prospective evaluation of insulin and insulin-like growth factor-I as risk factors for endometrial cancer. Cancer Epidemiol Biomarkers Prev. 2008; 17:921–9.
Article30. Giovannucci E. Nutrition, insulin, insulin-like growth factors and cancer. Horm Metab Res. 2003; 35:694–704.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to review and assess a systematic review and meta-analysis article: a methodological study (secondary publication)
- Systematic Review and Meta-analysis in Digestive Cancer Research
- Meta-epidemiology
- Systematic review and meta-analysis of cancer risks in relation to environmental waste incinerator emissions: a meta-analysis of case-control and cohort studies
- Serum vitamin D status and metabolic syndrome: a systematic review and dose-response meta-analysis