Korean Circ J.
2020 Oct;50(10):890-903. 10.4070/kcj.2020.0083.
Long-term Patient Prognostication by Coronary Flow Reserve and Index of Microcirculatory Resistance: International Registry of Comprehensive Physiologic Assessment
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea
- 3Department of Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea
- 4Division of Cardiology, Ulsan Hospital, Ulsan, Korea and Department of Cardiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 5Division of Cardiovascular Medicine, Tsuchiura Kyodo General Hospital, Ibaraki, Japan
- 6Department of Cardiovascular Medicine, Tokyo Medical and Dental University, Tokyo, Japan
- 7Cardiovascular Institute, Hospital Clinico San Carlos, Madrid, Spain
- 8Centro Nacional de Investigaciónes Cardiovasculares Carlos III (CNIC), Madrid, Spain
- 9Department of Internal Medicine and Cardiovascular Center, Seoul National University Hospital, Seoul, Korea
- 10Institute on Aging, Seoul National University, Seoul, Korea
- KMID: 2507006
- DOI: http://doi.org/10.4070/kcj.2020.0083
Abstract
- Background and Objectives
Recent guideline recommends evaluation using of coronary flow reserve (CFR) and index of microcirculatory resistance (IMR) in patients with functionally insignificant stenosis. We evaluated clinical implications of CFR and IMR in patients with high fractional flow reserve (FFR) and deferred revascularization.
Methods
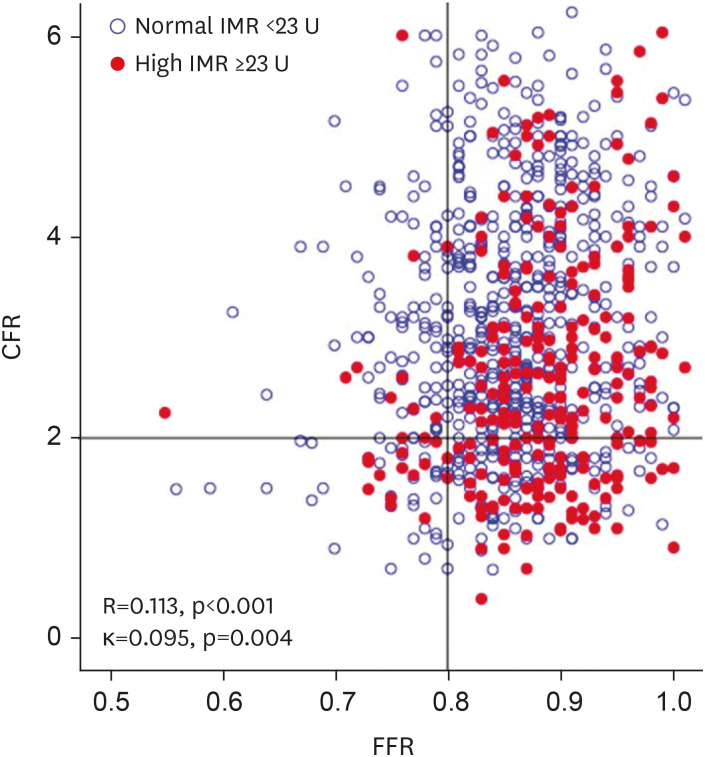
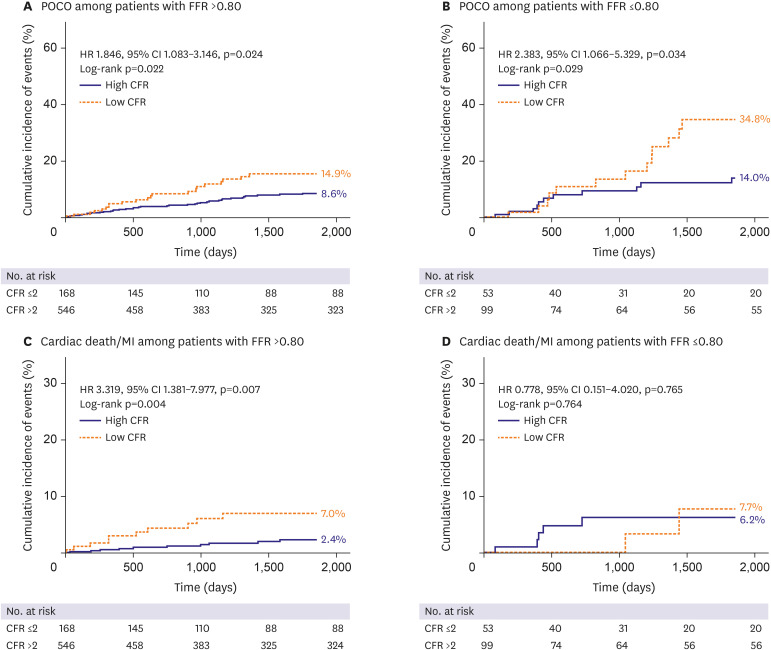
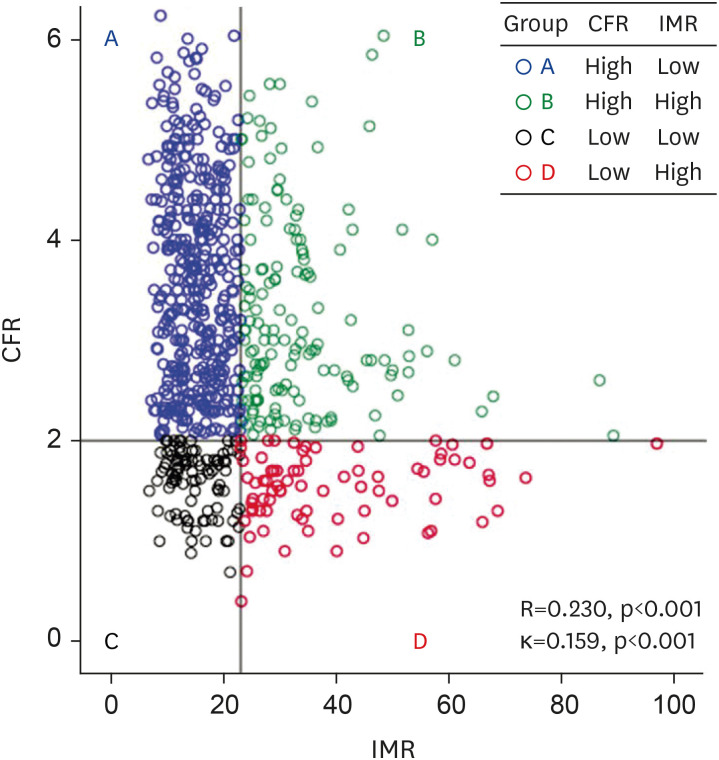
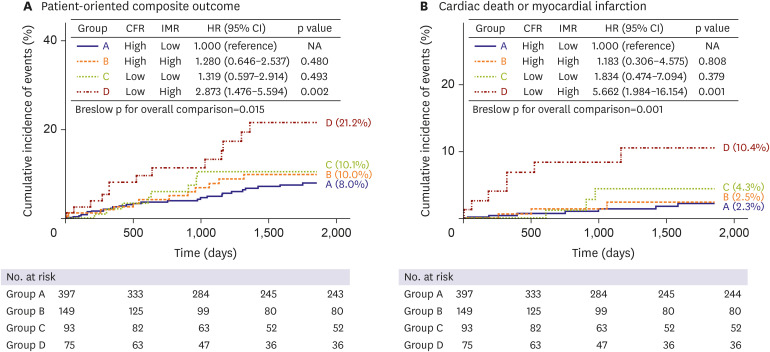
A total of 867 patients (1,152 vessels) consigned to deferred revascularization who underwent comprehensive physiologic assessments were enrolled. Patients with high FFR (>0.80) were categorized by CFR (≤2) and IMR (≥23 U). Clinical outcome was assessed by patient-oriented composite outcome (POCO), a composite of any death, myocardial infarction (MI), and revascularization at 5 years.
Results
Patients with low CFR (≤2) showed significantly greater risk of POCO than those with high CFR (>2) in both high-FFR (p=0.024) and low-FFR (p=0.034) groups. In patients with high FFR, those with low CFR and high IMR (overt microvascular disease) displayed the greatest risk of POCO overall (p=0.015), surpassing those with high CFR and low IMR (HR, 2.873; 95% CI, 1.476–5.594; p=0.002) and showing significantly greater risk of cardiac death or MI (HR, 5.662; 95% CI, 1.984–16.154; p=0.001). Overt microvascular disease was independently associated with POCO in the high-FFR population (HR, 2.282; 95% CI, 1.176–4.429; p=0.015).
Conclusion
Among patients with deferred revascularization, those with low CFR showed significantly greater risk of POCO than those with high CFR, regardless of FFR. In patients with high FFR, those with overt microvascular disease showed significantly greater risk of POCO and cardiac death or MI at 5-year, compared with the others.
Keyword
Figure
Cited by 2 articles
-
Coronary Microvascular Dysfunction: Is It Distinct Clinical Entity or Common Physiologic Pathway?
Jung-Min Ahn
Korean Circ J. 2020;50(10):904-906. doi: 10.4070/kcj.2020.0352.Would a Noninvasive Coronary Physiology Become a Standard and Popular Approach?
Yun-Kyeong Cho, Chang-Wook Nam
Korean Circ J. 2021;51(2):140-142. doi: 10.4070/kcj.2020.0511.
Reference
-
1. Hachamovitch R, Berman DS, Kiat H, Cohen I, Friedman JD, Shaw LJ. Value of stress myocardial perfusion single photon emission computed tomography in patients with normal resting electrocardiograms: an evaluation of incremental prognostic value and cost-effectiveness. Circulation. 2002; 105:823–829. PMID: 11854122.
Article2. Xaplanteris P, Fournier S, Pijls NH, et al. Five-year outcomes with PCI guided by fractional flow reserve. N Engl J Med. 2018; 379:250–259. PMID: 29785878.
Article3. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2018; 39:3759. PMID: 30403801.4. Lee JM, Jung JH, Hwang D, et al. Coronary flow reserve and microcirculatory resistance in patients with intermediate coronary stenosis. J Am Coll Cardiol. 2016; 67:1158–1169. PMID: 26965536.
Article5. Lee JM, Choi KH, Hwang D, et al. Prognostic implication of thermodilution coronary flow reserve in patients undergoing fractional flow reserve measurement. JACC Cardiovasc Interv. 2018; 11:1423–1433. PMID: 30093048.6. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020; 41:407–477. PMID: 31504439.7. Hamaya R, Yonetsu T, Kanaji Y, et al. Diagnostic and prognostic efficacy of coronary flow capacity obtained using pressure-temperature sensor-tipped wire-derived physiological indices. JACC Cardiovasc Interv. 2018; 11:728–737. PMID: 29605243.
Article8. Echavarria-Pinto M, Escaned J, Macías E, et al. Disturbed coronary hemodynamics in vessels with intermediate stenoses evaluated with fractional flow reserve: a combined analysis of epicardial and microcirculatory involvement in ischemic heart disease. Circulation. 2013; 128:2557–2566. PMID: 24141255.9. Mejía-Rentería H, Lee JM, Lauri F, et al. Influence of microcirculatory dysfunction on angiography-based functional assessment of coronary stenoses. JACC Cardiovasc Interv. 2018; 11:741–753. PMID: 29673505.
Article10. Johnson NP, Kirkeeide RL, Gould KL. Is discordance of coronary flow reserve and fractional flow reserve due to methodology or clinically relevant coronary pathophysiology? JACC Cardiovasc Imaging. 2012; 5:193–202. PMID: 22340827.
Article11. De Bruyne B, Fearon WF, Pijls NH, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med. 2014; 371:1208–1217. PMID: 25176289.
Article12. Lee JM, Layland J, Jung JH, et al. Integrated physiologic assessment of ischemic heart disease in real-world practice using index of microcirculatory resistance and fractional flow reserve: insights from the International Index of Microcirculatory Resistance Registry. Circ Cardiovasc Interv. 2015; 8:e002857. PMID: 26499500.
Article13. Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011; 123:2736–2747. PMID: 21670242.14. Authors/Task Force members. Windecker S, Kolh P, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014; 35:2541–2619. PMID: 25173339.15. Ahn JM, Park DW, Shin ES, et al. Fractional flow reserve and cardiac events in coronary artery disease: data from a prospective IRIS-FFR Registry (Interventional Cardiology Research Incooperation Society Fractional Flow Reserve). Circulation. 2017; 135:2241–2251. PMID: 28356440.16. Lee JM, Koo BK, Shin ES, et al. Clinical implications of three-vessel fractional flow reserve measurement in patients with coronary artery disease. Eur Heart J. 2018; 39:945–951. PMID: 29020260.
Article17. Li J, Elrashidi MY, Flammer AJ, et al. Long-term outcomes of fractional flow reserve-guided vs. angiography-guided percutaneous coronary intervention in contemporary practice. Eur Heart J. 2013; 34:1375–1383. PMID: 23344979.
Article18. van de Hoef TP, van Lavieren MA, Damman P, et al. Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ Cardiovasc Interv. 2014; 7:301–311. PMID: 24782198.
Article19. van de Hoef TP, Bax M, Damman P, et al. Impaired coronary autoregulation is associated with long-term fatal events in patients with stable coronary artery disease. Circ Cardiovasc Interv. 2013; 6:329–335. PMID: 23899871.
Article20. Meuwissen M, Chamuleau SA, Siebes M, et al. The prognostic value of combined intracoronary pressure and blood flow velocity measurements after deferral of percutaneous coronary intervention. Catheter Cardiovasc Interv. 2008; 71:291–297. PMID: 18288725.
Article21. Johnson NP, Gould KL. Integrating noninvasive absolute flow, coronary flow reserve, and ischemic thresholds into a comprehensive map of physiological severity. JACC Cardiovasc Imaging. 2012; 5:430–440. PMID: 22498334.
Article22. Ng MK, Yeung AC, Fearon WF. Invasive assessment of the coronary microcirculation: superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation. 2006; 113:2054–2061. PMID: 16636168.23. de Bruyne B, Bartunek J, Sys SU, Pijls NH, Heyndrickx GR, Wijns W. Simultaneous coronary pressure and flow velocity measurements in humans. Feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation. 1996; 94:1842–1849. PMID: 8873658.24. Murthy VL, Naya M, Taqueti VR, et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation. 2014; 129:2518–2527. PMID: 24787469.
Article25. Taqueti VR, Ridker PM. Inflammation, coronary flow reserve, and microvascular dysfunction: moving beyond cardiac syndrome X. JACC Cardiovasc Imaging. 2013; 6:668–671. PMID: 23764095.26. Camici PG, Olivotto I, Rimoldi OE. The coronary circulation and blood flow in left ventricular hypertrophy. J Mol Cell Cardiol. 2012; 52:857–864. PMID: 21924273.
Article27. Crea F, Camici PG, Bairey Merz CN. Coronary microvascular dysfunction: an update. Eur Heart J. 2014; 35:1101–1111. PMID: 24366916.
Article28. Förstermann U, Sessa WC. Nitric oxide synthases: regulation and function. Eur Heart J. 2012; 33:829–837. PMID: 21890489.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Physiologic Evaluation of Microvascular Damage in Culprit Vessel After Successful Primary Percutaneous Coronary Intervention for ST-elevation Myocardial Infarction Patients
- Physiologic Assessment of Coronary Artery Disease: Focus on Fractional Flow Reserve
- Short-Term Effect of High Dose of Vitamin C on Coronary Flow Velocity and Coronary Flow Reserve in Healthy Young Non-Smoker Men
- Physiologic Assessment after Coronary Stent Implantation
- Association between Cardiac Troponin Level and Coronary Flow Reserve in Patients without Coronary Artery Disease: Insight from a Thermodilution Technique Using an Intracoronary Pressure Wire