Korean Circ J.
2014 May;44(3):141-147. 10.4070/kcj.2014.44.3.141.
Association between Cardiac Troponin Level and Coronary Flow Reserve in Patients without Coronary Artery Disease: Insight from a Thermodilution Technique Using an Intracoronary Pressure Wire
- Affiliations
-
- 1Regional Cardiocerebrovascular Center, Dong-A University Hospital, Busan, Korea. kimyd@dau.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2145474
- DOI: http://doi.org/10.4070/kcj.2014.44.3.141
Abstract
- BACKGROUND AND OBJECTIVES
Cardiac troponins are associated with increased mortality, even among patients with no coronary artery disease. Elevated cardiac troponin levels are frequently observed in patients without significant coronary lesions, although the mechanism underlying this finding is unclear. The aim of our study was to evaluate the association between the levels of cardiac troponin and coronary flow reserve (CFR).
SUBJECTS AND METHODS
We evaluated serum cardiac troponin-I in 19 patients (9 female; age 61.9+/-10.9 year-old). All patients had an ejection fraction >40% and angiographically normal coronary arteries. Simultaneous measurements of fractional flow reserve (FFR), the index of microcirculatory resistance (IMR), and CFR measurements using an intracoronary temperature- and pressure-sensing guidewire under basal conditions and during maximal hyperemia were performed in three vessels: the left anterior descending artery (LAD), left circumflex artery (LCX) and right coronary artery (RCA).
RESULTS
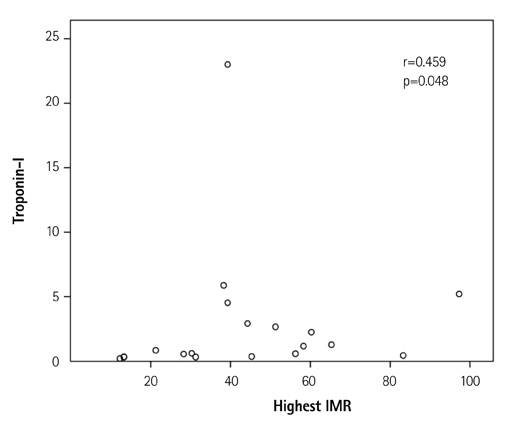
All patients were followed for a median of 13 months. FFR, IMR, and CFR measurements were performed successfully in all subjects. Mean CFRs of LAD, LCX, and RCA were 1.98+/-1.20, 2.75+/-2.11, and 4.44+/-2.51, respectively. Mean IMRs of LAD, LCX and RCA were 33.28+/-18.78, 29.11+/-26.70, and 30.55+/-23.65, respectively. There was a poor correlation between CFR and troponin-I values in each vessel. In selecting the lowest value of CFR in each patient as the corresponding value, the lowest CFR was not associated with troponin-I levels (r=-0.219, p=0.367).
CONCLUSION
In patients without significant coronary lesions, the correlation between CFR and troponin-I level was not significant using a thermodilution technique. Further study of a larger population with longer-term follow-up may be needed to more fully understand microvascular dysfunction.
MeSH Terms
Figure
Reference
-
1. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012; 60:1581–1598.2. Leonardi S, Thomas L, Neely ML, et al. Comparison of the prognosis of spontaneous and percutaneous coronary intervention-related myocardial infarction. J Am Coll Cardiol. 2012; 60:2296–2304.3. Agewall S, Giannitsis E, Jernberg T, Katus H. Troponin elevation in coronary vs. non-coronary disease. Eur Heart J. 2011; 32:404–411.4. Eggers KM, Lagerqvist B, Venge P, Wallentin L, Lindahl B. Persistent cardiac troponin I elevation in stabilized patients after an episode of acute coronary syndrome predicts long-term mortality. Circulation. 2007; 116:1907–1914.5. Leung DY, Leung M. Non-invasive/invasive imaging: significance and assessment of coronary microvascular dysfunction. Heart. 2011; 97:587–595.6. Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007; 356:830–840.7. Coffman JD, Gregg DE. Reactive hyperemia characteristics of the myocardium. Am J Physiol. 1960; 199:1143–1149.8. De Bruyne B, Pijls NH, Smith L, Wievegg M, Heyndrickx GR. Coronary thermodilution to assess flow reserve: experimental validation. Circulation. 2001; 104:2003–2006.9. Barbato E, Aarnoudse W, Aengevaeren WR, et al. Validation of coronary flow reserve measurements by thermodilution in clinical practice. Eur Heart J. 2004; 25:219–223.10. Eggers KM, Lind L, Ahlström H, et al. Prevalence and pathophysiological mechanisms of elevated cardiac troponin I levels in a population-based sample of elderly subjects. Eur Heart J. 2008; 29:2252–2258.11. van den Bos EJ, Constantinescu AA, van Domburg RT, Akin S, Jordaens LJ, Kofflard MJ. Minor elevations in troponin I are associated with mortality and adverse cardiac events in patients with atrial fibrillation. Eur Heart J. 2011; 32:611–617.12. Layland JJ, Whitbourn RJ, Burns AT, et al. The index of microvascular resistance identifies patients with periprocedural myocardial infarction in elective percutaneous coronary intervention. Heart. 2012; 98:1492–1497.13. Merx MW, Weber C. Sepsis and the heart. Circulation. 2007; 116:793–802.14. Nakanishi K, Fukuda S, Shimada K, et al. Prognostic value of coronary flow reserve on long-term cardiovascular outcomes in patients with chronic kidney disease. Am J Cardiol. 2013; 112:928–932.15. Cortigiani L, Rigo F, Gherardi S, et al. Coronary flow reserve during dipyridamole stress echocardiography predicts mortality. JACC Cardiovasc Imaging. 2012; 5:1079–1085.16. Beleslin B, Ostojic M, Djordjevic-Dikic A, et al. The value of fractional and coronary flow reserve in predicting myocardial recovery in patients with previous myocardial infarction. Eur Heart J. 2008; 29:2617–2624.17. Løgstrup BB, Høfsten DE, Christophersen TB, et al. Association between coronary flow reserve, left ventricular systolic function, and myocardial viability in acute myocardial infarction. Eur J Echocardiogr. 2010; 11:665–670.18. Takashio S, Yamamuro M, Izumiya Y, et al. Coronary microvascular dysfunction and diastolic load correlate with cardiac troponin T release measured by a highly sensitive assay in patients with nonischemic heart failure. J Am Coll Cardiol. 2013; 62:632–640.19. Sicari R, Rigo F, Cortigiani L, Gherardi S, Galderisi M, Picano E. Additive prognostic value of coronary flow reserve in patients with chest pain syndrome and normal or near-normal coronary arteries. Am J Cardiol. 2009; 103:626–631.20. Ng MK, Yeung AC, Fearon WF. Invasive assessment of the coronary microcirculation: superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation. 2006; 113:2054–2061.21. Kern MJ, Lerman A, Bech JW, et al. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory: a scientific statement from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Circulation. 2006; 114:1321–1341.22. Lim HS, Yoon MH, Tahk SJ, et al. Usefulness of the index of microcirculatory resistance for invasively assessing myocardial viability immediately after primary angioplasty for anterior myocardial infarction. Eur Heart J. 2009; 30:2854–2860.23. Oh JH, Kim C, Ahn J, et al. The relationship between microcirculatory resistance and fractional flow reserve in patients with acute Myocardial infarction. Korean Circ J. 2013; 43:534–540.24. Fearon WF, Shah M, Ng M, et al. Predictive value of the index of microcirculatory resistance in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2008; 51:560–565.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Pressure Wire in Coronary Artery Disease
- Coronary Flow Velocity Pattern in Patients with Myocardial Bridging of Coronary Artery
- Myocardial Contrast Echocardiography for the Assessment of Coronary Blood Flow Reserve
- Physiologic approach for coronary intervention
- Relation Between Vascular Resistance and Intimal Thickness in Patients with Coronary Artery Disease