Neonatal Med.
2020 May;27(2):45-50. 10.5385/nm.2020.27.2.45.
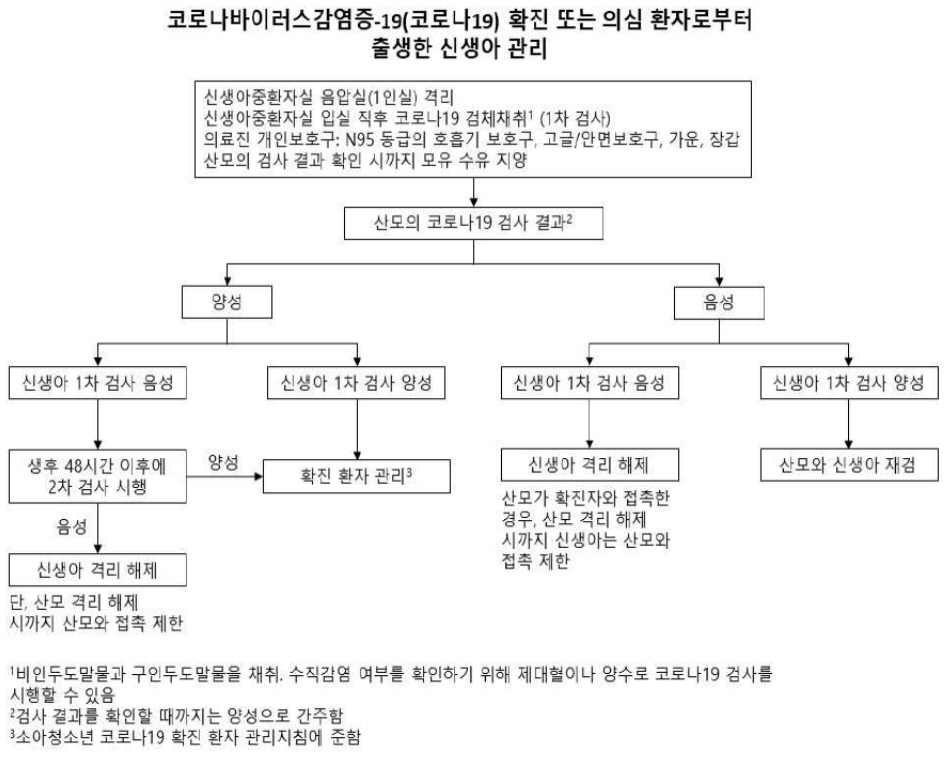
Response Guidelines for Newborn Infants Born to Mothers with Suspected or Confirmed Coronavirus Disease 2019
- Affiliations
-
- 1Department of Pediatrics, Dongguk University Ilsan Hospital, Goyang, Korea
- KMID: 2503158
- DOI: http://doi.org/10.5385/nm.2020.27.2.45
Abstract
- Since December 2019, the coronavirus disease 2019 (COVID-19) has been spreading rapidly worldwide. With the increase in the number of infections, the numbers of pregnant women and newborn infants with COVID-19 are also increasing. Accord ing to the limited recent studies, COVID-19 appears to be mainly transmitted to newborn infants by the mother’s droplets or direct contact with the mother, and no clear evidence supports the vertical transmission from the mother to the newborn infant. To date, the likelihood of severe outcomes in newborn infants born to mothers with confirmed COVID-19 is relatively very low, but the possibility should be considered. The present response guidelines address the management of newborn infants born to mothers with suspected or confirmed COVID-19. The management covers precautions for birth attendants or medical staffs, testing for COVID-19, isolation, neonatal care, breastfeeding, and mother/baby contact. These response guidelines can be revised in accordance with further updates on COVID-19 and should be adapted to each local health-care facility.
Keyword
Figure
Cited by 1 articles
-
Response Guidelines for Coronavirus Disease 2019 in Newborn Infants: A 2021 Update
Do-Hyun Kim
J Korean Soc Matern Child Health. 2021;25(3):162-168. doi: 10.21896/jksmch.2021.25.3.162.
Reference
-
1. The Korean Society of Pediatric Infectious Diseases. COVID-19 response guidelines (newborn, infant, child and adolescent) [Internet]. Seoul: The Korean Society of Pediatric Infectious Diseases;2020. [cited 2020 May 16]. Available from: http://www.kspid.or.kr/.2. Schwartz DA. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmis sion of SARS-CoV-2: maternal coronavirus infections and pregnancy outcomes. Arch Pathol Lab Med. 2020; Mar. 17. [Epub]. https://doi.org/10.5858/arpa.2020-0901-SA.3. Schwartz DA, Graham AL. Potential maternal and infant outcomes from (Wuhan) coronavirus 2019-nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020; 12:194.4. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020; 395:809–15.5. Zeng L, Xia S, Yuan W, Yan K, Xiao F, Shao J, et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. 2020; e200878.6. Maxwell C, McGeer A, Tai KFY, Sermer M. No. 225: Management guidelines for obstetric patients and neonates born to mothers with suspected or probable severe acute respiratory syndrome (SARS). J Obstet Gynaecol Can. 2017; 39:e130–7.7. Korea Center for Disease Control and Prevention. Coronavirus disease (COVID-19) response guidelines 7th edition [Internet]. Sejong: Ministry of Health and Welfare;2020. [cited 2020 May 16]. Available from: http://ncov.mohw.go.kr/.8. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19): considerations for inpatient obstetric healthcare settings [Internet]. Atlanta: CDC;2020. [cited 2020 May 16]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/inpatient-obstetric-healthcare-guidance. html.9. American Academy of Pediatrics. AAP issues guidance on infants born to mothers with suspected or confirmed COVID-19 [Internet]. Itasca: AAP;2020. [cited May 16]. Available from: https://www.aappublications.org/news/2020/04/02/infantcovidguidance040220.10. Provincial Infectious Diseases Advisory Committee (PIDAC). Best practice for infection prevention and control in perinatology: in all health care settings that provide obstetrical and newborn care [Internet]. Toronto: Public Health Ontario;c2020. [cited 2020 Apr 1]. Available from: https://www.publichealthontario.ca/-/media/documents/bp-ipac-perinatology.pdf?la=en.11. Bryant K. Healthcare-associated infections in newborn nurseries and neonatal intensive care units. In : Glen MC, editor. Hospital epidemiology and infection control. 4th ed. Philadelphia: Lippincott Williams & Wilkins;2012. p. 738–56.12. RPA Newborn Care Infection QI subcommittee and adapted material from the Provincial Infectious Diseases Advi sory Committee Ontario. Women and babies: infection prevention and control in NICU [Internet]. Camperdown: NSW Government;2015. [cited 2020 May 16]. Available from: https://www.slhd.nsw.gov.au/rpa/neonatal%5Ccontent/pdf/guidelines/Inf ectionControlGuidelineMar2015.pdf.13. Lee SJ, Na S. Recent trend about pregnant women with suspected or confirmed coronavirus disease 2019 (COVID-19) infection. Perinatology. 2020; 31:1–6.14. Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020; 222:415–26.15. Favre G, Pomar L, Qi X, Nielsen-Saines K, Musso D, Baud D. Guidelines for pregnant women with suspected SARS-CoV-2 infection. Lancet Infect Dis. 2020; Mar. 3. [Epub]. https://doi. org/10.1016/S1473-3099(20)30157-2.16. Poon LC, Yang H, Lee JCS, Copel JA, Leung TY, Zhang Y, et al. ISUOG Interim Guidance on 2019 novel coronavirus infection during pregnancy and puerperium: information for healthcare professionals. Ultrasound Obstet Gynecol. 2020; 55:700–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Response Guidelines for Coronavirus Disease 2019 in Newborn Infants: A 2021 Update
- No title available
- Outcomes of Late-Preterm and Term Infants Born to SARS-CoV-2-Positive Mothers
- Recent Trend about Pregnant Women with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) Infection
- Postnatal Outcome of Neonatal Thyroid Function Born to Mother with Thyroid Dysfunction