Nutr Res Pract.
2020 Jun;14(3):230-241. 10.4162/nrp.2020.14.3.230.
Effect of nutritional supplement formula on catch-up growth in young children with nonorganic faltering growth: a prospective multicenter study
- Affiliations
-
- 1Department of Pediatrics, Korea University Guro Hospital, Korea University College of Medicine, Seoul 08308, Korea
- 2Department of Pediatrics, Severance Hospital, Yonsei University College of Medicine, Seoul 03722, Korea
- 3Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu 41404, Korea
- 4Department of Pediatrics, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Gyeongsang Institute of Sciences, Jinju 52727, Korea
- 5Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam 13620, Korea
- KMID: 2502483
- DOI: http://doi.org/10.4162/nrp.2020.14.3.230
Abstract
- BACKGROUND/OBJECTIVES
Inadequate nutrition in infants and young children affects physical growth and neurocognitive development. Therefore, early nutritional intervention is important to promote catch-up growth in young children with faltering growth. The aim of this study was to evaluate the effect of nutritional supplementation with a pediatric concentrated and balanced nutritional supplement formula on promoting growth and improving nutritional status in children with nonorganic faltering growth.
SUBJECTS/METHODS
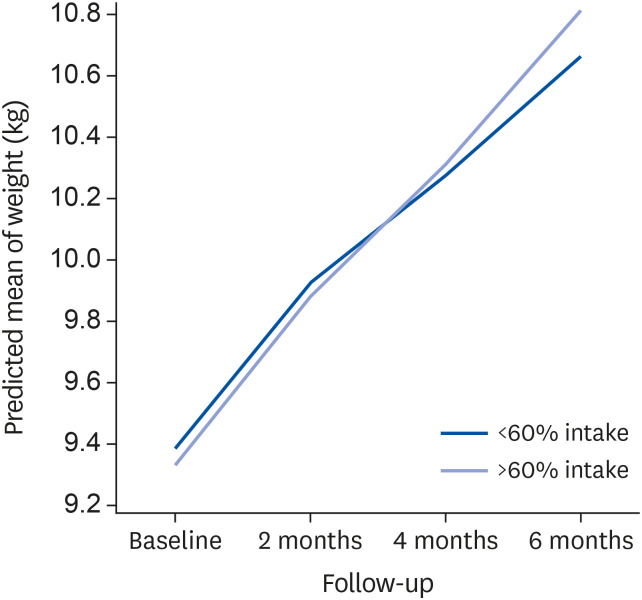
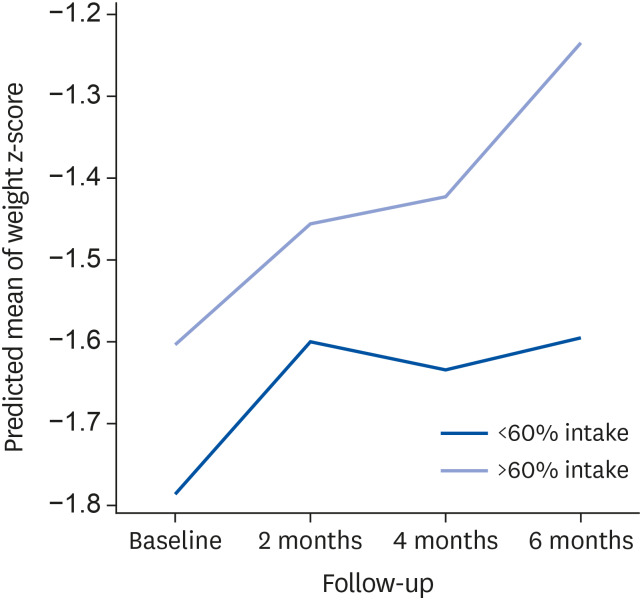
Children aged 12–36 months whose body weight-for-age was < 5th percentile on the Korean Growth Charts were enrolled. Children born premature or having organic diseases were excluded. Children were instructed to consume 400 mL of formula per day in addition to their regular diet for 6 months. Pediatricians and dietitians educated the parents and examined the subjects every 2 months. Anthropometric parameters were measured at baseline and at 2, 4, and 6 months, and laboratory tests were done at baseline and 6 months. The good consumption group included children who consumed ≥ 60% of the recommended dose of formula.
RESULTS
Total 82 children completed the 6-month intervention. At baseline, there were no significant differences in all variables between the good consumption and poor consumption groups. Weight and weight z-scores were significantly improved in the good consumption group compared to the poor consumption group at the end of the intervention (P = 0.009, respectively). The good consumption group showed a significant trend for gaining weight (P < 0.05) and weight z-score (P < 0.05) compared to the poor consumption group during 6 months of formula intake. The concentration of blood urea nitrogen was significantly increased in the good consumption group (P = 0.001).
CONCLUSIONS
Nutritional supplementation with a concentrated and balanced pediatric nutritional formula along with dietary education might be an effective approach to promote catch-up growth in children with nonorganic faltering growth.
Figure
Reference
-
1. National Guideline Alliance (UK). Faltering Growth: Recognition and Management. NICE Guideline. London: National Institute for Health and Care Excellence;2017.2. Cherry R. Growth faltering/failure to thrive. In : Wyllie R, Hyams JS, Kay M, editors. Pediatric Gastrointestinal and Liver Disease. 5th ed. Philadelphia: Elsevier;2016. p. 137–143.3. Olsen EM. Failure to thrive: still a problem of definition. Clin Pediatr (Phila). 2006; 45:1–6. PMID: 16429209.
Article4. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, Lee JH, Kim SC, Lim D, Yang SW, Oh K, Moon JS. Committee for the Development of Growth Standards for Korean Children and Adolescents. Committee for School Health and Public Health Statistics, the Korean Pediatric Society. Division of Health and Nutrition Survey, Korea Centers for Disease Control and Prevention. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–149. PMID: 29853938.
Article5. UNICEF. WHO. The World Bank project. 2011 joint child malnutrition estimates - levels and trends [Internet]. Geneva: WHO;2012. cited 2020 February 25. Available from: https://www.who.int/nutgrowthdb/estimates2011/en/.6. Olsen EM, Petersen J, Skovgaard AM, Weile B, Jørgensen T, Wright CM. Failure to thrive: the prevalence and concurrence of anthropometric criteria in a general infant population. Arch Dis Child. 2007; 92:109–114. PMID: 16531456.
Article7. Shrimpton R, Victora CG, de Onis M, Lima RC, Blössner M, Clugston G. Worldwide timing of growth faltering: implications for nutritional interventions. Pediatrics. 2001; 107:E75. PMID: 11331725.
Article8. Larson-Nath C, Biank VF. Clinical review of failure to thrive in pediatric patients. Pediatr Ann. 2016; 45:e46–9. PMID: 26878182.
Article9. Carruth BR, Skinner J, Houck K, Moran J 3rd, Coletta F, Ott D. The phenomenon of “picky eater”: a behavioral marker in eating patterns of toddlers. J Am Coll Nutr. 1998; 17:180–186. PMID: 9550462.
Article10. Spitz RA. Hospitalism; an inquiry into the genesis of psychiatric conditions in early childhood. Psychoanal Study Child. 1945; 1:53–74. PMID: 21004303.11. Block RW, Krebs NF. American Academy of Pediatrics Committee on Child Abuse and Neglect. American Academy of Pediatrics Committee on Nutrition. Failure to thrive as a manifestation of child neglect. Pediatrics. 2005; 116:1234–1237. PMID: 16264015.
Article12. Estrem HH, Pados BF, Park J, Knafl KA, Thoyre SM. Feeding problems in infancy and early childhood: evolutionary concept analysis. J Adv Nurs. 2017; 73:56–70. PMID: 27601073.
Article13. Williams KE, Field DG, Seiverling L. Food refusal in children: a review of the literature. Res Dev Disabil. 2010; 31:625–633. PMID: 20153948.
Article14. Sharp WG, Jaquess DL, Morton JF, Herzinger CV. Pediatric feeding disorders: a quantitative synthesis of treatment outcomes. Clin Child Fam Psychol Rev. 2010; 13:348–365. PMID: 20844951.
Article15. Lebenthal Y, Yackobovitch-Gavan M, Lazar L, Shalitin S, Tenenbaum A, Shamir R, Phillip M. Effect of a nutritional supplement on growth in short and lean prepubertal children: a prospective, randomized, double-blind, placebo-controlled study. J Pediatr. 2014; 165:1190–1193.e1. PMID: 25241181.
Article16. Yackobovitch-Gavan M, Lebenthal Y, Lazar L, Shalitin S, Demol S, Tenenbaum A, Shamir R, Phillip M. Effect of Nutritional supplementation on growth in short and lean prepubertal children after 1 year of intervention. J Pediatr. 2016; 179:154–159.e1. PMID: 27697330.
Article17. Lundeen EA, Behrman JR, Crookston BT, Dearden KA, Engle P, Georgiadis A, Penny ME, Stein AD. Young Lives Determinants and Consequences of Child Growth Project Team. Growth faltering and recovery in children aged 1–8 years in four low- and middle-income countries: Young Lives. Public Health Nutr. 2014; 17:2131–2137. PMID: 24477079.
Article18. Kim JE. Nutritional state of children in the Democratic People's Republic of Korea (DPRK): based on the DPRK final report of the national nutrition survey 2012. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:135–139. PMID: 25349828.
Article19. Mitchell WG, Gorrell RW, Greenberg RA. Failure-to-thrive: a study in a primary care setting. Epidemiology and follow-up. Pediatrics. 1980; 65:971–977. PMID: 7367142.20. Larson-Nath CM, Goday PS. Failure to thrive: a prospective study in a pediatric gastroenterology clinic. J Pediatr Gastroenterol Nutr. 2016; 62:907–913. PMID: 26720767.21. Daniel M, Kleis L, Cemeroglu AP. Etiology of failure to thrive in infants and toddlers referred to a pediatric endocrinology outpatient clinic. Clin Pediatr (Phila). 2008; 47:762–765. PMID: 18467671.
Article22. Kerzner B, Milano K, MacLean WC Jr, Berall G, Stuart S, Chatoor I. A practical approach to classifying and managing feeding difficulties. Pediatrics. 2015; 135:344–353. PMID: 25560449.
Article23. Fewtrell MS, Morley R, Abbott RA, Singhal A, Stephenson T, MacFadyen UM, Clements H, Lucas A. Catch-up growth in small-for-gestational-age term infants: a randomized trial. Am J Clin Nutr. 2001; 74:516–523. PMID: 11566651.
Article24. Clarke SE, Evans S, Macdonald A, Davies P, Booth IW. Randomized comparison of a nutrient-dense formula with an energy-supplemented formula for infants with faltering growth. J Hum Nutr Diet. 2007; 20:329–339. PMID: 17635310.
Article25. Ramstack M, Listernick R. Safety and efficacy of a new pediatric enteral product in the young child. JPEN J Parenter Enteral Nutr. 1991; 15:89–92. PMID: 1901114.
Article26. Alarcon PA, Lin LH, Noche M Jr, Hernandez VC, Cimafranca L, Lam W, Comer GM. Effect of oral supplementation on catch-up growth in picky eaters. Clin Pediatr (Phila). 2003; 42:209–217. PMID: 12739919.
Article27. Rivera JA, Hotz C, González-Cossío T, Neufeld L, García-Guerra A. The effect of micronutrient deficiencies on child growth: a review of results from community-based supplementation trials. J Nutr. 2003; 133:4010S–4020S. PMID: 14672304.
Article28. Brown KH, Peerson JM, Rivera J, Allen LH. Effect of supplemental zinc on the growth and serum zinc concentrations of prepubertal children: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2002; 75:1062–1071. PMID: 12036814.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between short stature at 3 years old and height, weight, and body mass index changes for 6 years after birth: a retrospective, nationwide, population-based study of children born 2011–2014 in Korea
- Post-discharge Nutrition
- Comparison of the growth and nutritional status of low birth weight and normal birth weight children
- The Usefulness of Birth Weight Z-Score as a Predictor of Catch Up Growth in Preterm Infants
- Nutritional Strategies for Optimal Growth of Small for Gestational Age Infants: Updates