Cancer Res Treat.
2020 Jan;52(1):301-308. 10.4143/crt.2019.194.
Time Trends for Prostate Cancer Incidence from 2003 to 2013 in South Korea: An Age-Period-Cohort Analysis
- Affiliations
-
- 1Department of Urology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- 2Department of Statistics, Graduate School of Chung-Ang University, Seoul, Korea
- KMID: 2501222
- DOI: http://doi.org/10.4143/crt.2019.194
Abstract
- Purpose
Prostate cancer (PCa) incidence is affected by aging phenomenon and performance of screening test. In United States, PCa incidence is affected by period effect of U.S. Preventive Services Task Force (USPSTF) recommendation. However, no study has reported the effect of USPSTF recommendation or aging phenomenon on PCa incidence in South Korea. Thus, the objective of this study was to investigate effects of age, period, and birth cohort on PCa incidence using age-period-cohort analysis.
Materials and Methods
Annual report of cancer statistics between 2003 and 2013 from National Health Insurance Service (NHIS) in South Korea for the number of PCa patients and Korean Statistical Information Service (KOSIS) data between 2003 and 2013 from national statistics in South Korea for the number of Korean male population were used. Age-period-cohort models were used to investigate effects of age, period, and birth cohort on PCa incidence.
Results
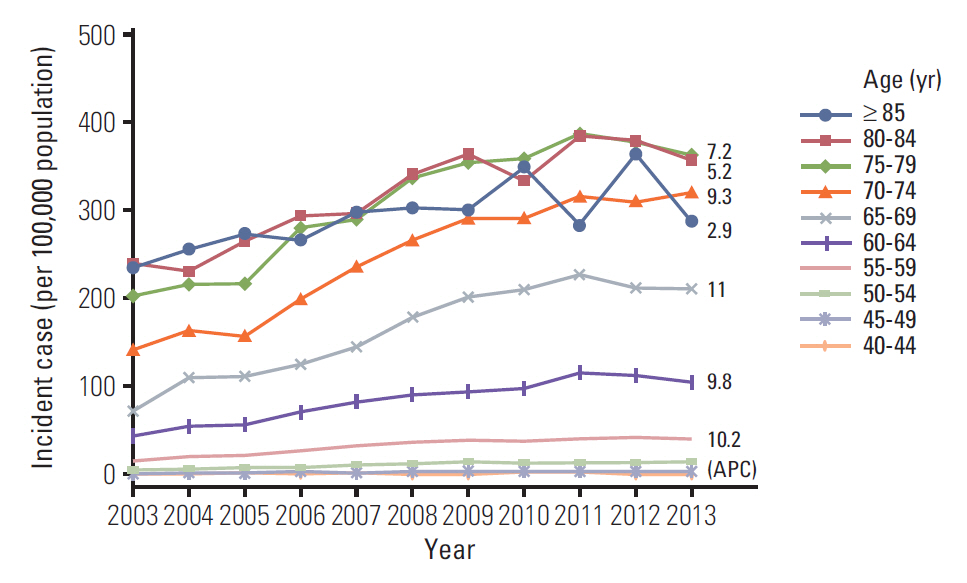
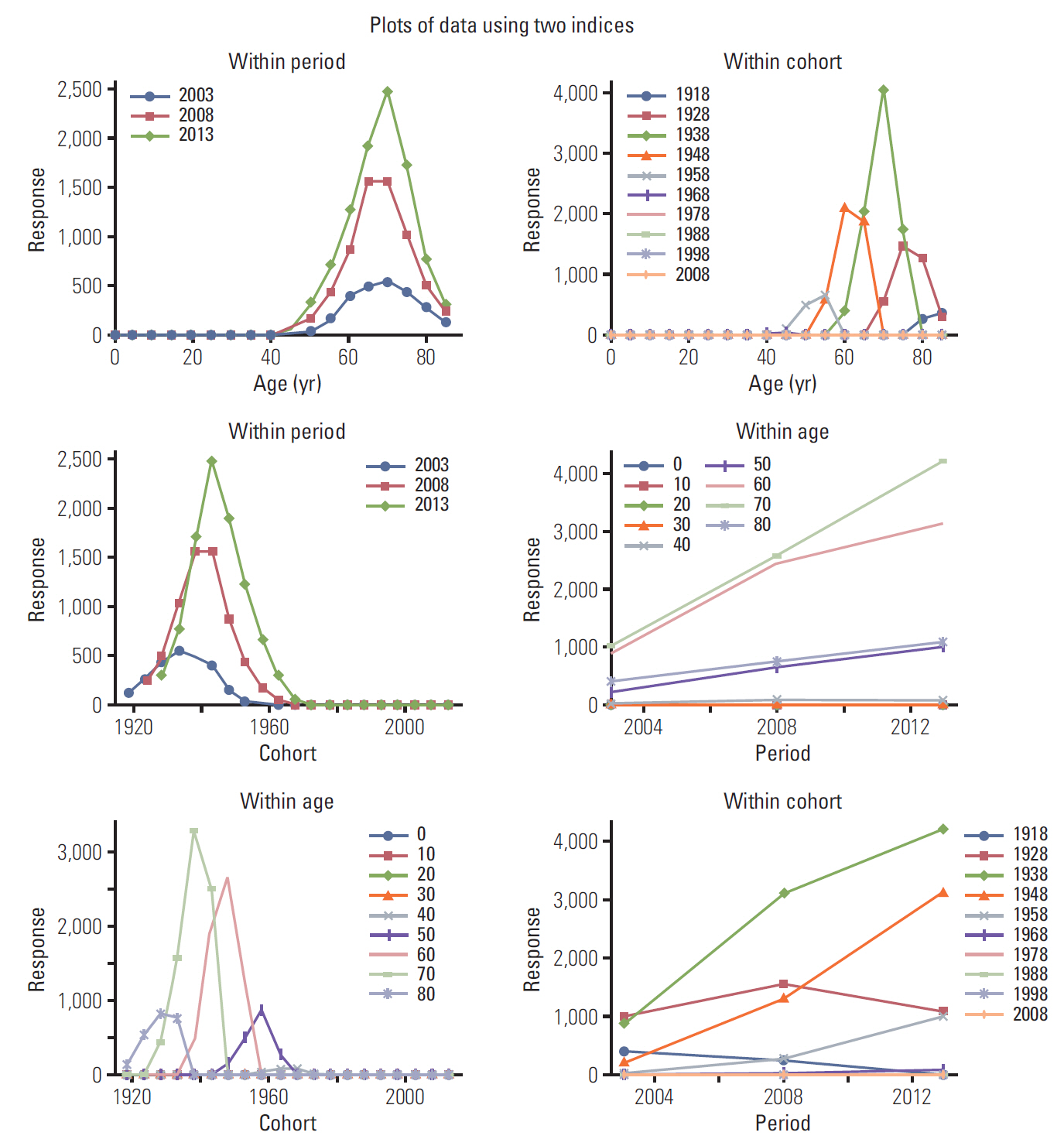
Overall PCa incidence in South Korea was increased 8.8% in annual percentage (95% confidential interval, 6.5 to 11.2; p < 0.001). It showed an increasing pattern from 2003 to 2011 but a decreasing pattern from 2011 to 2013. Age increased the risk of PCa incidence. However, the speed of increase was slower with increasing age. PCa incidence was increased 1.4 times in 2008 compared to that in 2003 or 2013. Regarding cohort effect, the risk of PCa incidence started to increase from 1958 cohort.
Conclusion
PCa incidence was affected by period of specific year. There was a positive cohort effect on PCa incidence associated with age structural change.
Keyword
Figure
Cited by 1 articles
-
A Web-Based Decision Aid for Informed Prostate Cancer Screening: Development and Pilot Evaluation
Wonyoung Jung, In Young Cho, Keun Hye Jeon, Yohwan Yeo, Jae Kwan Jun, Mina Suh, Ansuk Jeong, Jungkwon Lee, Dong Wook Shin
J Korean Med Sci. 2023;38(46):e360. doi: 10.3346/jkms.2023.38.e360.
Reference
-
References
1. Joung JY, Lim J, Oh CM, Jung KW, Cho H, Kim SH, et al. Current trends in the incidence and survival rate of urological cancers in Korea. Cancer Res Treat. 2017; 49:607–15.
Article2. Braga SF, de Souza MC, Cherchiglia ML. Time trends for prostate cancer mortality in Brazil and its geographic regions: an age-period-cohort analysis. Cancer Epidemiol. 2017; 50:53–9.
Article3. Song W, Jeon HG. Incidence of kidney, bladder, and prostate cancers in Korea: an update. Korean J Urol. 2015; 56:422–8.
Article4. Kim JH, Kim SY, Yun SJ, Chung JI, Choi H, Yu HS, et al. Medical travel among non-Seoul residents to seek prostate cancer treatment in medical facilities of Seoul. Cancer Res Treat. 2019; 51:53–64.
Article5. Lee EY, Kim HC, Rhee Y, Youm Y, Kim KM, Lee JM, et al. The Korean urban rural elderly cohort study: study design and protocol. BMC Geriatr. 2014; 14:33.
Article6. Barocas DA, Mallin K, Graves AJ, Penson DF, Palis B, Winchester DP, et al. Effect of the USPSTF grade D recommendation against screening for prostate cancer on incident prostate cancer diagnoses in the United States. J Urol. 2015; 194:1587–93.
Article7. Hoffman RM, Meisner AL, Arap W, Barry M, Shah SK, Zeliadt SB, et al. Trends in United States prostate cancer incidence rates by age and stage, 1995-2012. Cancer Epidemiol Biomarkers Prev. 2016; 25:259–63.
Article8. Gejerman G, Ciccone P, Goldstein M, Lanteri V, Schlecker B, Sanzone J, et al. US Preventive Services Task Force prostatespecific antigen screening guidelines result in higher Gleason score diagnoses. Investig Clin Urol. 2017; 58:423–8.
Article9. Kelly SP, Anderson WF, Rosenberg PS, Cook MB. Past, current, and future incidence rates and burden of metastatic prostate cancer in the United States. Eur Urol Focus. 2018; 4:121–7.
Article10. Bibbins-Domingo K, Grossman DC, Curry SJ. The US Preventive Services Task Force 2017 Draft recommendation statement on screening for prostate cancer: an invitation to review and comment. JAMA. 2017; 317:1949–50.11. Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2014; 23:2296–302.
Article12. Niclis C, Pou SA, Bengio RH, Osella AR, Diaz Mdel P. Prostate cancer mortality trends in Argentina 1986-2006: an age-period-cohort and joinpoint analysis. Cad Saude Publica. 2011; 27:123–30.
Article13. Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol. 2012; 61:1079–92.
Article14. Kakehi Y, Sugimoto M, Taoka R; Committee for establishment of the evidenced-based clinical practice guideline for prostate cancer of the Japanese Urological Association. Evidenced-based clinical practice guideline for prostate cancer (summary: Japanese Urological Association, 2016 edition). Int J Urol. 2017; 24:648–66.
Article15. Kimura T, Egawa S. Epidemiology of prostate cancer in Asian countries. Int J Urol. 2018; 25:524–31.
Article16. Moyer VA; U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012; 157:120–34.
Article17. Lin K, Lipsitz R, Miller T, Janakiraman S; U.S. Preventive Services Task Force. Benefits and harms of prostate-specific antigen screening for prostate cancer: an evidence update for the U.S. Preventive Services Task Force. Ann Intern Med. 2008; 149:192–9.
Article18. Chi BH, Chang IH. Prostate cancer: recent trends in Korea. Urol Int. 2010; 85:88–93.
Article19. Park SK, Sakoda LC, Kang D, Chokkalingam AP, Lee E, Shin HR, et al. Rising prostate cancer rates in South Korea. Prostate. 2006; 66:1285–91.
Article20. Yi KH. The revised 2016 Korean Thyroid Association guidelines for thyroid nodules and cancers: differences from the 2015 American Thyroid Association guidelines. Endocrinol Metab (Seoul). 2016; 31:373–8.
Article21. Choi KM, Park HS, Han JH, Lee JS, Lee J, Ryu OH, et al. Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens. 2006; 24:1515–21.
Article22. Heo J, Jeon SY, Oh CM, Hwang J, Oh J, Cho Y. The unrealized potential: cohort effects and age-period-cohort analysis. Epidemiol Health. 2017; 39:e2017056.
Article23. Sung H, Rosenberg PS, Chen WQ, Hartman M, Lim WY, Chia KS, et al. Female breast cancer incidence among Asian and Western populations: more similar than expected. J Natl Cancer Inst. 2015; 107:djv107.
Article24. Bao PP, Zheng Y, Wu CX, Huang ZZ, Gao YT, Jin F, et al. Cancer incidence in urban Shanghai, 1973-2010: an updated trend and age-period-cohort effects. BMC Cancer. 2016; 16:284.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Age-Period-Cohort Analysis of Thyroid Cancer Incidence in Korea
- Temporal Changes of Lung Cancer Mortality in Korea
- Region-Based Analysis of Prevalence and Incidence of Parkinson's Disease: Analysis of the National Sample Cohort in South Korea
- Long Term Trends and the Future Gastric Cancer Mortality in Korea : 1983~2013
- Trends and Age-Period-Cohort Effects on the Incidence and Mortality Rate of Cervical Cancer in Korea