J Korean Soc Radiol.
2020 Jan;81(1):243-247. 10.3348/jksr.2020.81.1.243.
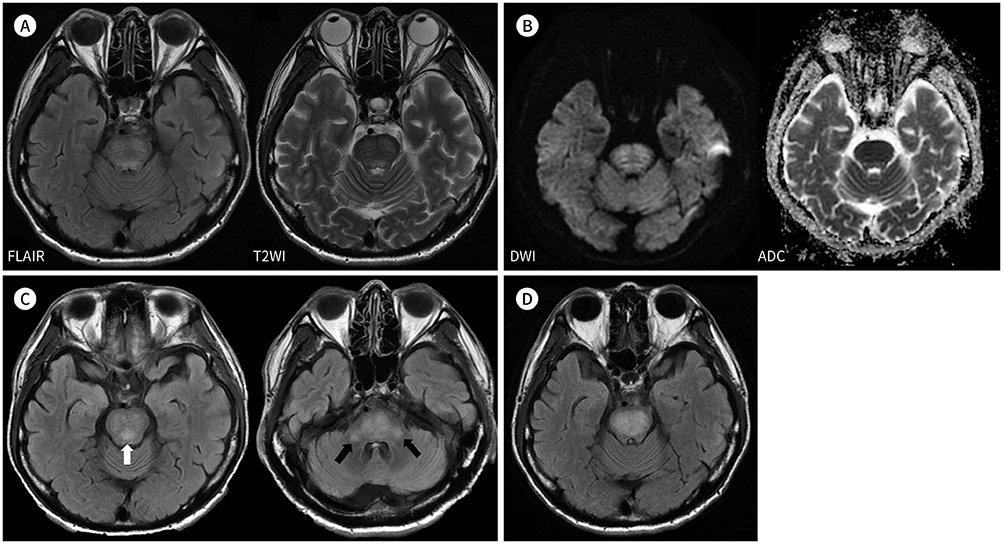
Serial Magnetic Resonance Imaging Findings in Hyperglycemia-Related Osmotic Demyelination Syndrome: A Case Report
- Affiliations
-
- 1Department of Radiology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea. nhpark@mjh.or.kr
- KMID: 2469201
- DOI: http://doi.org/10.3348/jksr.2020.81.1.243
Abstract
- We report a rare case of hyperglycemia-related osmotic demyelination syndrome (ODS) with focus on the imaging findings. A 61-year-old man with diabetes was admitted for general weakness and severe thirst. A few days later, he complained of dysarthria, dysphasia, and dysmetria. Laboratory examinations showed significant hyperglycemia, but normal electrolyte levels. Brain MRI revealed T2-signal abnormalities that were symmetrical, non-space occupying, and located in the central pons with a peripheral sparing pattern, which were suggestive of ODS. In addition, subsequent MRI revealed progression of signal hyperintensity; however, the patient's symptoms improved.
MeSH Terms
Figure
Reference
-
1. O'Malley G, Moran C, Draman MS, King T, Smith D, Thompson CJ, et al. Central pontine myelinolysis complicating treatment of the hyperglycaemic hyperosmolar state. Ann Clin Biochem. 2008; 45:440–443.2. Burns JD, Kosa SC, Wijdicks EF. Central pontine myelinolysis in a patient with hyperosmolar hyperglycemia and consistently normal serum sodium. Neurocrit Care. 2009; 11:251–254.
Article3. Adams RD, Victor M, Mancall EL. Central pontine myelinolysis: a hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Arch Neurol Psychiatry. 1959; 81:154–172.4. Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry. 2004; 75 Suppl 3:iii22–iii28.
Article5. Hirosawa T, Shimizu T. Osmotic demyelination syndrome due to hyperosmolar hyperglycemia. Cleve Clin J Med. 2018; 85:511–513.
Article6. Saini M, Mamauag MJ, Singh R. Central pontine myelinolysis: a rare presentation secondary to hyperglycaemia. Singapore Med J. 2015; 56:e71–e73.
Article7. Chang YM. Central pontine myelinolysis associated with diabetic hyperglycemia. JSM Clin Case Rep. 2014; 2:1059.8. Rodríguez-Velver KV, Soto-Garcia AJ, Zapata-Rivera MA, Montes-Villarreal J, Villarreal-Pérez JZ, Rodríguez-Gutiérrez R. Osmotic demyelination syndrome as the initial manifestation of a hyperosmolar hyperglycemic state. Case Rep Neurol Med. 2014; 2014:652523.
Article9. Linyu N, Das BR, Mossang K, Singh SR, Prasad L, Naorem S. Osmotic demyelination syndrome occurs early in the course of hyperosmolar Hyperglycemic state. IOSR-JDMS. 2017; 16:25–22.10. Osborn AG, Salzman KL, Jhaveri MD, Barkovich AJ. Diagnostic imaging: brain. 3rd ed. Philadelphia: Elsevier;2015.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cortical Laminar Necrosis associated with Osmotic Demyelination Syndrome
- Osmotic Demyelination Syndrome with Recent Chemotherapy in Normonatremic Patient: A Case Report
- Characteristic Magnetic Resonance Imaging Findings of Osmotic Demyelination Syndrome in a Patient with Minimal Hyponatremia
- A Case of Osmotic Demyelination Presenting with Severe Hypernatremia
- Dynamic Contrast-Enhanced MR Imaging of Tietze’s Syndrome: a Case Report