Prog Med Phys.
2019 Dec;30(4):155-159. 10.14316/pmp.2019.30.4.155.
Radiological Characteristics of Materials Used in 3-Dimensional Printing with Various Infill Densities
- Affiliations
-
- 1Department of Radiation Oncology, Veterans Health Service Medical Center, Seoul, Korea. mumuki79@gmail.com
- KMID: 2468177
- DOI: http://doi.org/10.14316/pmp.2019.30.4.155
Abstract
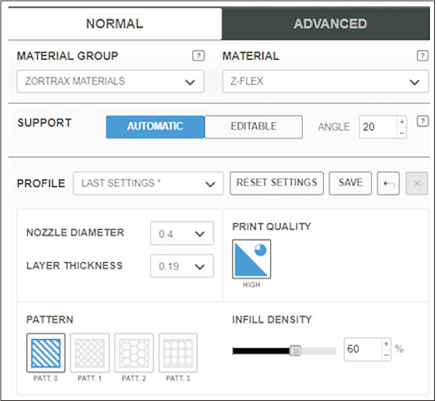
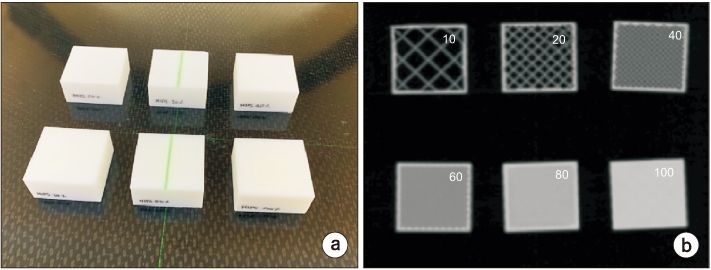
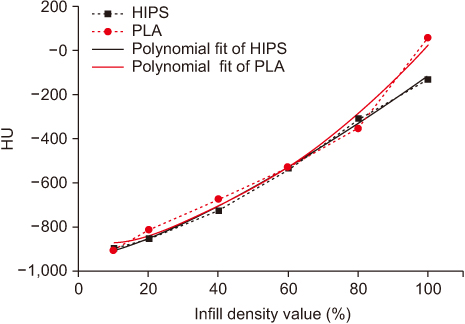
- Radiological properties of newly introduced and existing 3-dimensional (3D) printing materials were evaluated by measuring their Hounsfield units (HUs) at varying infill densities. The six materials for 3D printing which consisted of acrylonitrile butadiene styrene (ABS), a unique ABS plastic blend manufactured by Zortrax (ULTRAT), high impact polystyrene (HIPS), polyethylene terephthalate glycol (PETG), polylactic acid (PLA), and a thermoplastic polyester elastomer manufactured by Zortrax (FLEX) were used. We used computed tomography (CT) imaging to determine the HU values of each material, and thus assess its suitability for various applications in radiation oncology. We found that several material and infill density combinations resembled the HU values of fat, soft tissues, and lungs; however, none of the tested materials exhibited HU values similar to that of bone. These results will help researchers and clinicians develop more appropriate instruments for improving the quality of radiation therapy. Using optimized infill densities will help improve the quality of radiation therapy by producing customized instruments for each field of radiation therapy.
MeSH Terms
Figure
Reference
-
1. Jones EL, Tonino Baldion A, Thomas C, Burrows T, Byrne N, Newton V, et al. Introduction of novel 3D-printed superficial applicators for high-dose-rate skin brachytherapy. Brachytherapy. 2017; 16:409–414.
Article2. Ricotti R, Vavassori A, Bazani A, Ciardo D, Pansini F, Spoto R, et al. 3D-printed applicators for high dose rate brachytherapy: dosimetric assessment at different infill percentage. Phys Med. 2016; 32:1698–1706.
Article3. Zhao Y, Moran K, Yewondwossen M, Allan J, Clarke S, Rajaraman M, et al. Clinical applications of 3-dimensional printing in radiation therapy. Med Dosim. 2017; 42:150–155.
Article4. Park SY, Kang S, Park JM, An HJ, Oh DH, Kim JI. Development and dosimetric assessment of a patient-specific elastic skin applicator for high-dose-rate brachytherapy. Brachytherapy. 2019; 18:224–232.
Article5. Madamesila J, McGeachy P, Villarreal Barajas JE, Khan R. Characterizing 3D printing in the fabrication of variable density phantoms for quality assurance of radiotherapy. Phys Med. 2016; 32:242–247.
Article6. Park SY, Kim JI, Joo YH, Lee JC, Park JM. Total body irradiation with a compensator fabricated using a 3D optical scanner and a 3D printer. Phys Med Biol. 2017; 62:3735–3756.
Article7. Park SY, Choi CH, Park JM, Chun M, Han JH, Kim JI. A patient-specific polylactic acid bolus made by a 3D printer for breast cancer radiation therapy. PLoS One. 2016; 11:e0168063.
Article8. Choi CH, Kim JI, Park JM. A 3D-printed patient-specific applicator guide for use in high-dose-rate interstitial brachytherapy for tongue cancer: a phantom study. Phys Med Biol. 2019; 64:135002.
Article9. Mitsouras D, Liacouras P, Imanzadeh A, Giannopoulos AA, Cai T, Kumamaru KK, et al. Medical 3D printing for the radiologist. Radiographics. 2015; 35:1965–1988.
Article10. Kadoya N, Abe K, Nemoto H, Sato K, Ieko Y, Ito K, et al. Evaluation of a 3D-printed heterogeneous anthropomorphic head and neck phantom for patient-specific quality assurance in intensity-modulated radiation therapy. Radiol Phys Technol. 2019; 12:351–356.
Article11. Ehler ED, Barney BM, Higgins PD, Dusenbery KE. Patient specific 3D printed phantom for IMRT quality assurance. Phys Med Biol. 2014; 59:5763–5773.
Article12. Yea JW, Park JW, Kim SK, Kim DY, Kim JG, Seo CY, et al. Feasibility of a 3D-printed anthropomorphic patient-specific head phantom for patient-specific quality assurance of intensity-modulated radiotherapy. PLoS One. 2017; 12:e0181560.
Article13. Lee CL, Dietrich MC, Desai UG, Das A, Yu S, Xiang HF, et al. A 3D-printed patient-specific phantom for external beam radiation therapy of prostate cancer. J Eng Sci Med Diagn Ther. 2018; 1:041004.
Article14. Oh SA, Kim MJ, Kang JS, Hwang HS, Kim YJ, Kim SH, et al. Feasibility of fabricating variable density phantoms using 3D printing for quality assurance (QA) in radiotherapy. Prog Med Phys. 2017; 28:106–110.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Feasibility of Fabricating Variable Density Phantoms Using 3D Printing for Quality Assurance (QA) in Radiotherapy
- Three-Dimensional Printing Technology in Orthopedic Surgery
- Current Advances in Three-Dimensional Tissue/Organ Printing
- Application of Three-Dimensional Printing in the Fracture Management
- Emergence of Three-Dimensional Printing Technology and Its Utility in Spine Surgery