Prog Med Phys.
2019 Dec;30(4):104-111. 10.14316/pmp.2019.30.4.104.
Dosimetric Effects of Air Pocket during Magnetic Resonance-Guided Adaptive Radiation Therapy for Pancreatic Cancer
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea. hjooon.an@gmail.com
- 2Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea.
- 3Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea.
- 4Robotics Research Laboratory for Extreme Environments, Advanced Institutes of Convergence Technology, Suwon, Korea.
- KMID: 2468171
- DOI: http://doi.org/10.14316/pmp.2019.30.4.104
Abstract
- PURPOSE
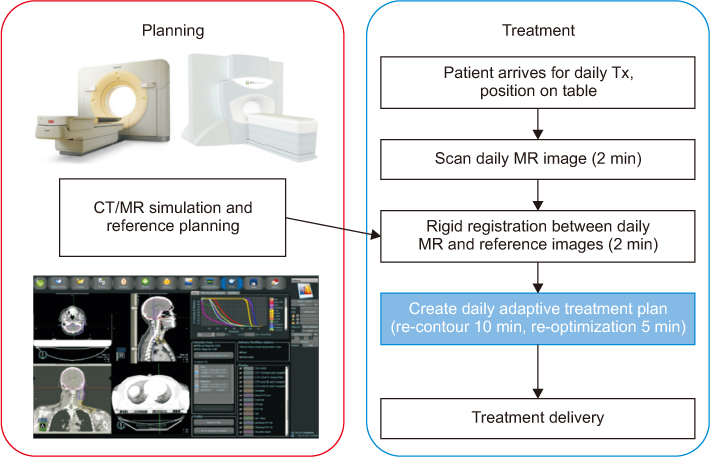
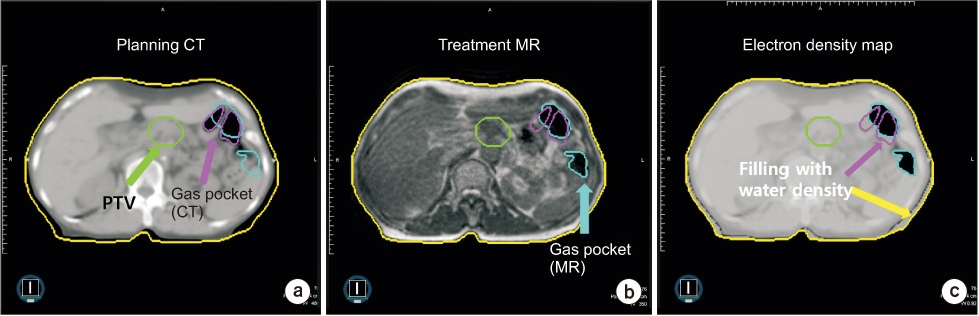
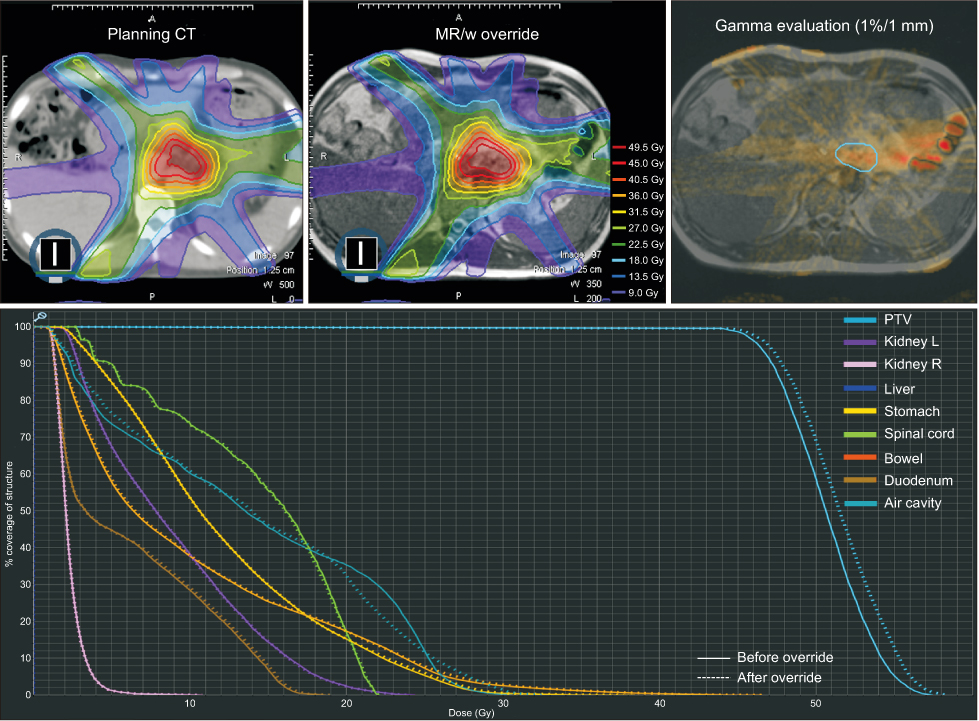
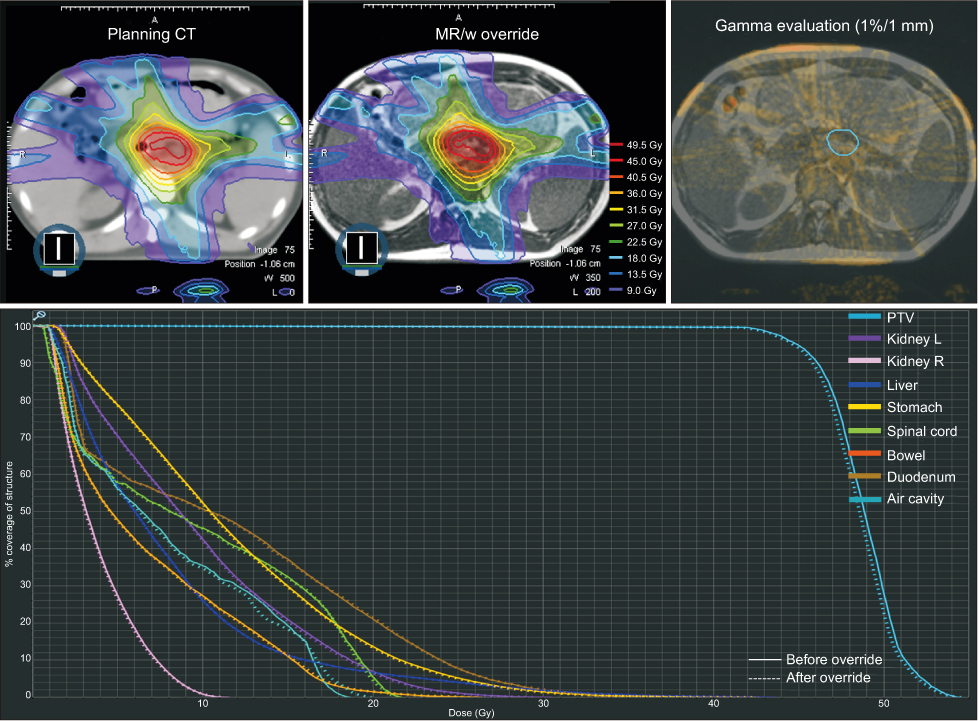
Online magnetic resonance-guided adaptive radiotherapy (MRgART), an emerging technique, is used to address the change in anatomical structures, such as treatment target region, during the treatment period. However, the electron density map used for dose calculation differs from that for daily treatment, owing to the variation in organ location and, notably, air pockets. In this study, we evaluate the dosimetric effect of electron density override on air pockets during online ART for pancreatic cancer cases.
METHODS
Five pancreatic cancer patients, who were treated with MRgART at the Seoul National University Hospital, were enrolled in the study. Intensity modulated radiation therapy plans were generated for each patient with 60Co beams on a ViewrayTM system, with a 45 Gy prescription dose for stereotactic body radiation therapy. During the treatment, the electron density map was modified based on the daily MR image. We recalculated the dose distribution on the plan, and the dosimetric parameters were obtained from the dose volume histograms of the planning target volume (PTV) and organs at risk.
RESULTS
The average dose difference in the PTV was 0.86Gy, and the observed difference at the maximum dose was up to 2.07 Gy. The variation in air pockets during treatment resulted in an under- or overdose in the PTV.
CONCLUSIONS
We recommend the re-contouring of the air pockets to deliver an accurate radiation dose to the target in MRgART, even though it is a time-consuming method.
Keyword
Figure
Cited by 1 articles
-
Dosimetric Evaluation of Synthetic Computed Tomography Technique on Position Variation of Air Cavity in Magnetic Resonance-Guided Radiotherapy
Hyeongmin Jin, Hyun Joon An, Eui Kyu Chie, Jong Min Park, Jung-in Kim
Prog Med Phys. 2022;33(4):142-149. doi: 10.14316/pmp.2022.33.4.142.
Reference
-
1. Hidalgo M. Pancreatic cancer. N Engl J Med. 2010; 362:1605–1617.
Article2. Wang F, Kumar P. The role of radiotherapy in management of pancreatic cancer. J Gastrointest Oncol. 2011; 2:157–167.3. Boldrini L, Cusumano D, Cellini F, Azario L, Mattiucci GC, Valentini V. Online adaptive magnetic resonance guided radiotherapy for pancreatic cancer: state of the art, pearls and pitfalls. Radiat Oncol. 2019; 14:71.
Article4. Rudra S, Jiang N, Rosenberg SA, Olsen JR, Roach MC, Wan L, et al. Using adaptive magnetic resonance image-guided radiation therapy for treatment of inoperable pancreatic cancer. Cancer Med. 2019; 8:2123–2132.
Article5. Berger T, Petersen JBB, Lindegaard JC, Fokdal LU, Tanderup K. Impact of bowel gas and body outline variations on total accumulated dose with intensity-modulated proton therapy in locally advanced cervical cancer patients. Acta Oncol. 2017; 56:1472–1478.
Article6. Estabrook NC, Corn JB, Ewing MM, Cardenes HR, Das IJ. Dosimetric impact of gastrointestinal air column in radiation treatment of pancreatic cancer. Br J Radiol. 2018; 91:20170512.
Article7. Onal C, Guler OC, Dolek Y. The impact of air pockets around the vaginal cylinder on vaginal vault brachytherapy. Br J Radiol. 2015; 88:20140694.
Article8. Hunt A, Hansen VN, Oelfke U, Nill S, Hafeez S. Adaptive radiotherapy enabled by MRI guidance. Clin Oncol (R Coll Radiol). 2018; 30:711–719.
Article9. Keall P, Poulsen P, Booth JT. See, think, and act: real-time adaptive radiotherapy. Semin Radiat Oncol. 2019; 29:228–235.
Article10. Klein EE, Chin LM, Rice RK, Mijnheer BJ. The influence of air cavities on interface doses for photon beams. Int J Radiat Oncol Biol Phys. 1993; 27:419–427.
Article11. Paudel MR, Kim A, Sarfehnia A, Ahmad SB, Beachey DJ, Sahgal A, et al. Experimental evaluation of a GPU-based Monte Carlo dose calculation algorithm in the Monaco treatment planning system. J Appl Clin Med Phys. 2016; 17:230–241.
Article12. Bohoudi O, Bruynzeel AME, Senan S, Cuijpers JP, Slotman BJ, Lagerwaard FJ, et al. Fast and robust online adaptive planning in stereotactic MR-guided adaptive radiation therapy (SMART) for pancreatic cancer. Radiother Oncol. 2017; 125:439–444.
Article13. Spieler B, Patel NV, Breto AL, Ford J, Stoyanova R, Zavala-Romero O, et al. Automatic segmentation of abdominal anatomy by artificial intelligence (AI) in adaptive radiotherapy of pancreatic cancer. Int J Radiat Oncol Biol Phys. 2019; 105:E130–E131.
Article14. Men K, Zhang T, Chen X, Chen B, Tang Y, Wang S, et al. Fully automatic and robust segmentation of the clinical target volume for radiotherapy of breast cancer using big data and deep learning. Phys Med. 2018; 50:13–19.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dosimetric Evaluation of Synthetic Computed Tomography Technique on Position Variation of Air Cavity in Magnetic Resonance-Guided Radiotherapy
- Dosimetric evaluation of magnetic resonance imaging-guided adaptive radiation therapy in pancreatic cancer by extent of re-contouring of organs-at-risk
- Image-guided radiation therapy in lymphoma management
- Adjuvant Therapy of Pancreatic Cancer
- Management for locally advanced cervical cancer: new trends and controversial issues