Prog Med Phys.
2022 Dec;33(4):142-149. 10.14316/pmp.2022.33.4.142.
Dosimetric Evaluation of Synthetic Computed Tomography Technique on Position Variation of Air Cavity in Magnetic Resonance-Guided Radiotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea
- 2Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 3Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2537883
- DOI: http://doi.org/10.14316/pmp.2022.33.4.142
Abstract
- Purpose
This study seeks to compare the dosimetric parameters of the bulk electron density (ED) approach and synthetic computed tomography (CT) image in terms of position variation of the air cavity in magnetic resonance-guided radiotherapy (MRgRT) for patients with pancreatic cancer.
Methods
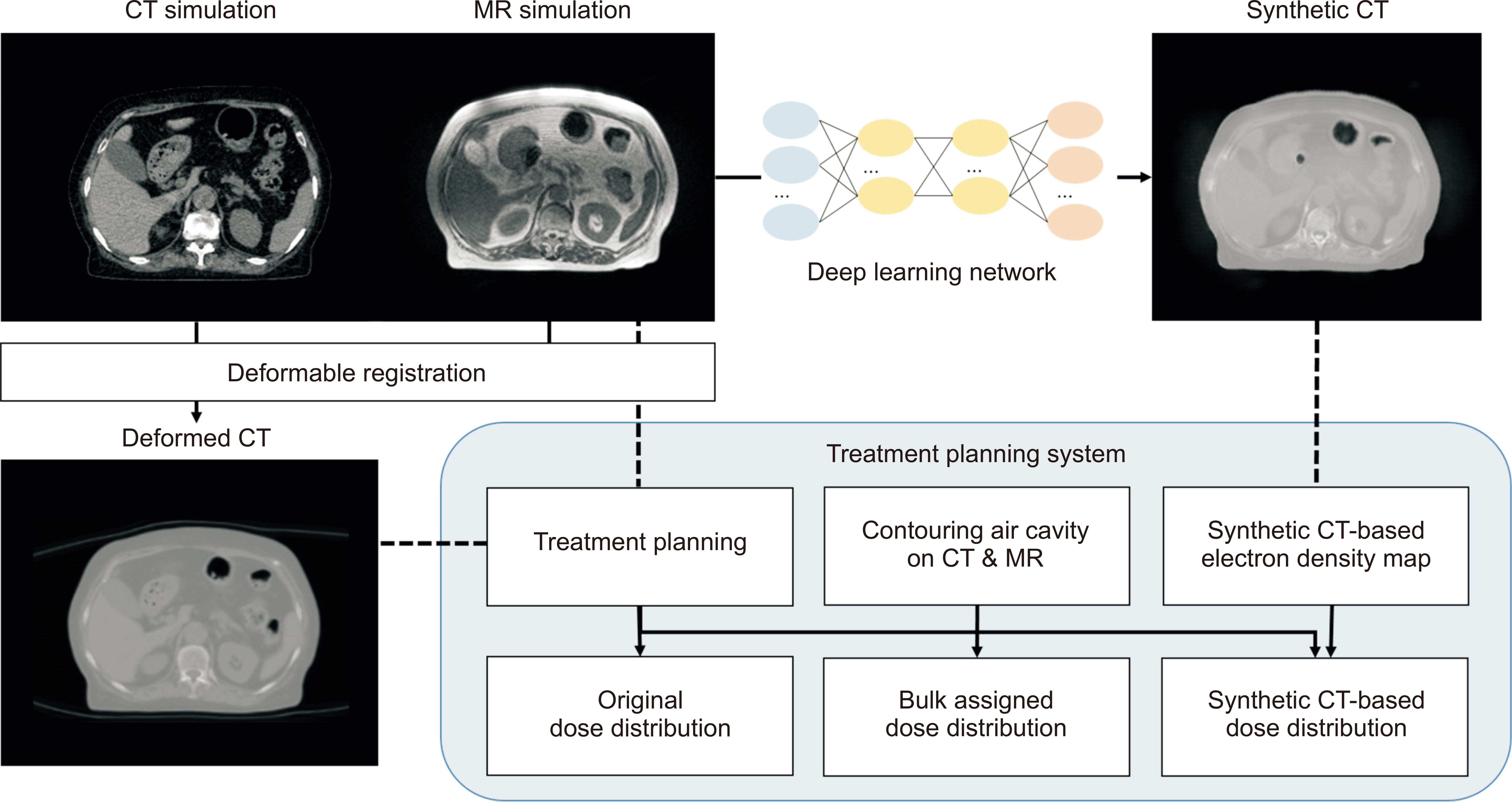
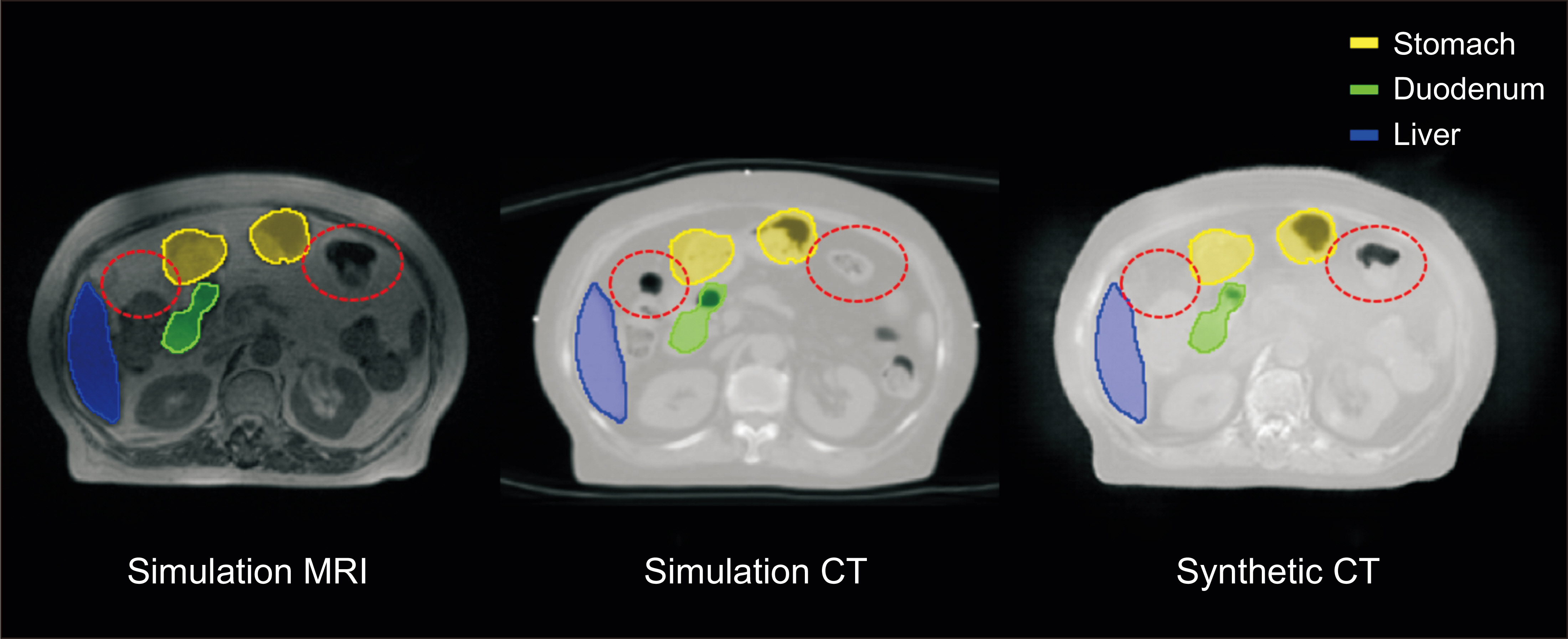
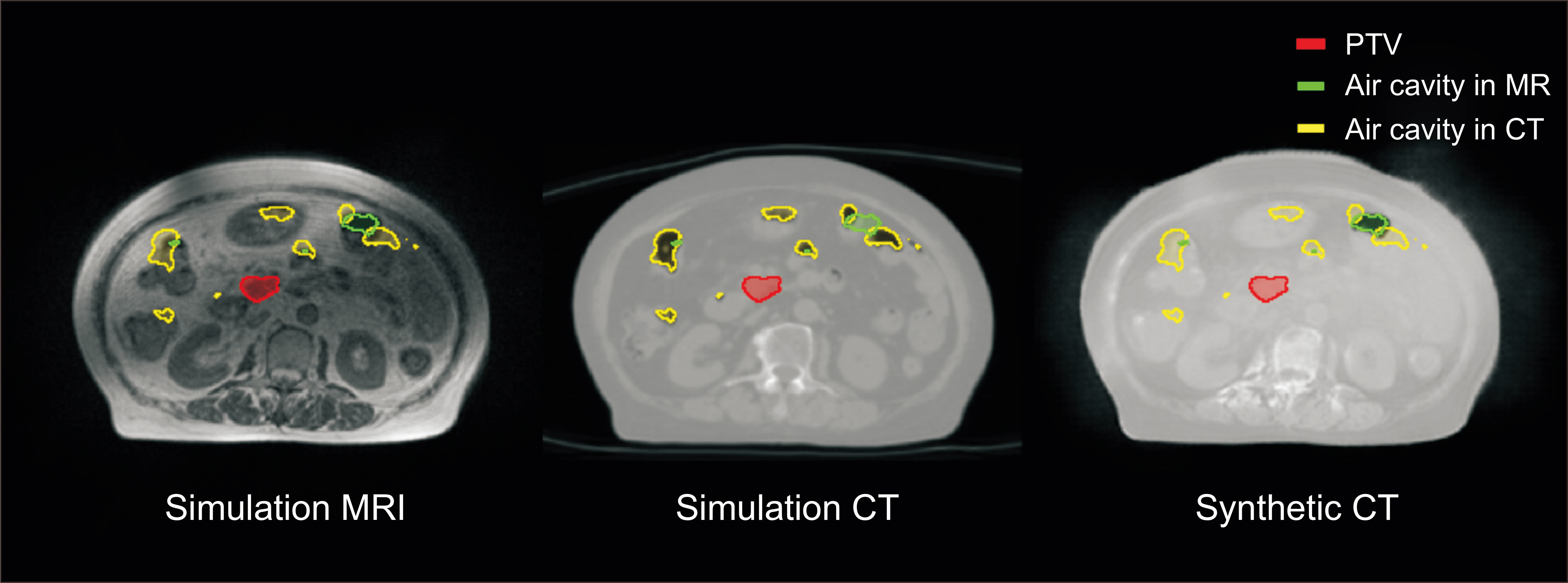
This study included nine patients that previously received MRgRT and their simulation CT and magnetic resonance (MR) images were collected. Air cavities were manually delineated on simulation CT and MR images in the treatment planning system for each patient. The synthetic CT images were generated using the deep learning model trained in a prior study. Two more plans with identical beam parameters were recalculated with ED maps that were either manually overridden by the cavities or derived from the synthetic CT. Dose calculation accuracy was explored in terms of dose-volume histogram parameters and gamma analysis.
Results
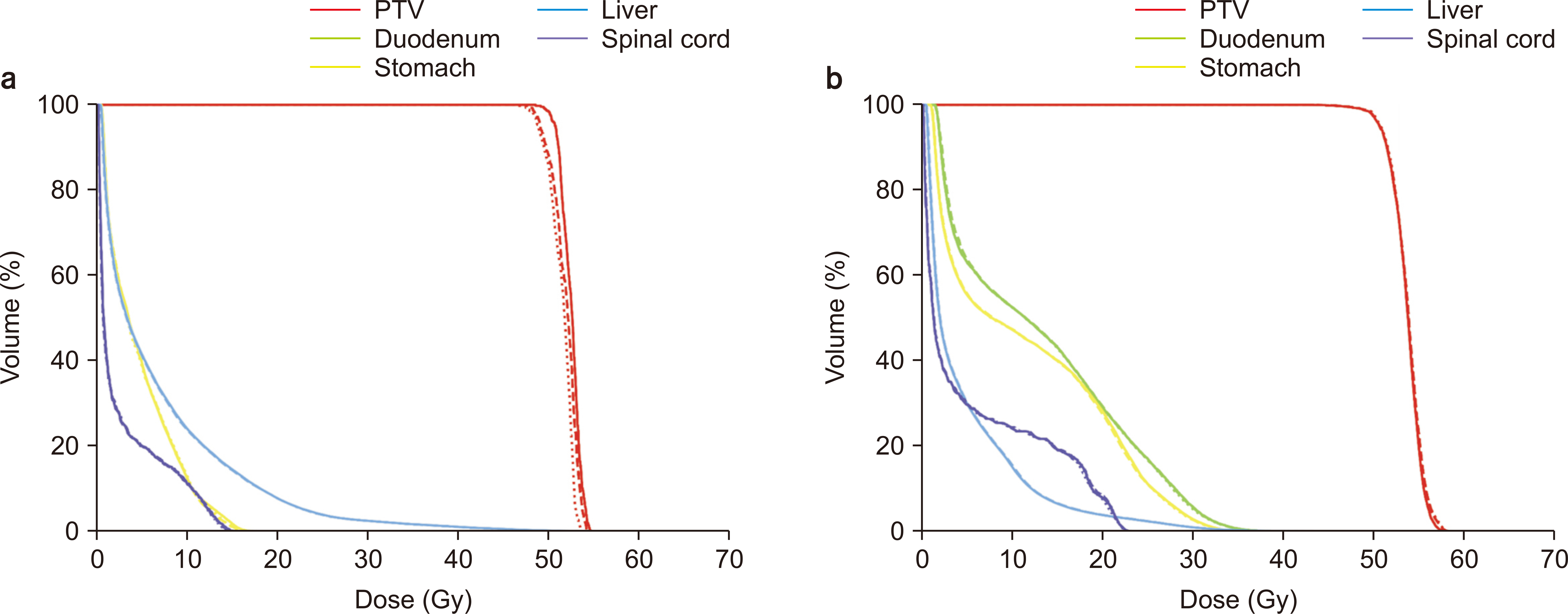
The D 95% averages were 48.80 Gy, 48.50 Gy, and 48.23 Gy for the original, manually assigned, and synthetic CT-based dose distributions, respectively. The greatest deviation was observed for one patient, whose D 95% to synthetic CT was 1.84 Gy higher than the original plan.
Conclusions
The variation of the air cavity position in the gastrointestinal area affects the treatment dose calculation. Synthetic CT-based ED modification would be a significant option for shortening the time-consuming process and improving MRgRT treatment accuracy.
Keyword
Figure
Reference
-
References
1. Lim-Reinders S, Keller BM, Al-Ward S, Sahgal A, Kim A. 2017; Online adaptive radiation therapy. Int J Radiat Oncol Biol Phys. 99:994–1003. DOI: 10.1016/j.ijrobp.2017.04.023. PMID: 28916139.
Article2. Kurz C, Buizza G, Landry G, Kamp F, Rabe M, Paganelli C, et al. 2020; Medical physics challenges in clinical MR-guided radiotherapy. Radiat Oncol. 15:93. DOI: 10.1186/s13014-020-01524-4. PMID: 32370788. PMCID: PMC7201982.
Article3. Hassanzadeh C, Rudra S, Bommireddy A, Hawkins WG, Wang-Gillam A, Fields RC, et al. 2020; Ablative five-fraction stereotactic body radiation therapy for inoperable pancreatic cancer using online MR-guided adaptation. Adv Radiat Oncol. 6:100506. DOI: 10.1016/j.adro.2020.06.010. PMID: 33665480. PMCID: PMC7897757.
Article4. Intven MPW, de Mol van Otterloo SR, Mook S, Doornaert PAH, de Groot-van Breugel EN, Sikkes GG, et al. 2021; Online adaptive MR-guided radiotherapy for rectal cancer; feasibility of the workflow on a 1.5T MR-linac: clinical implementation and initial experience. Radiother Oncol. 154:172–178. DOI: 10.1016/j.radonc.2020.09.024. PMID: 32976875.
Article5. Kupelian P, Sonke JJ. 2014; Magnetic resonance-guided adaptive radiotherapy: a solution to the future. Semin Radiat Oncol. 24:227–232. DOI: 10.1016/j.semradonc.2014.02.013. PMID: 24931098.
Article6. Pollard JM, Wen Z, Sadagopan R, Wang J, Ibbott GS. 2017; The future of image-guided radiotherapy will be MR guided. Br J Radiol. 90:20160667. DOI: 10.1259/bjr.20160667. PMID: 28256898. PMCID: PMC5605101.
Article7. Mutic S, Dempsey JF. 2014; The ViewRay system: magnetic resonance-guided and controlled radiotherapy. Semin Radiat Oncol. 24:196–199. DOI: 10.1016/j.semradonc.2014.02.008. PMID: 24931092.
Article8. Maspero M, Savenije MHF, Dinkla AM, Seevinck PR, Intven MPW, Jurgenliemk-Schulz IM, et al. 2018; Dose evaluation of fast synthetic-CT generation using a generative adversarial network for general pelvis MR-only radiotherapy. Phys Med Biol. 63:185001. DOI: 10.1088/1361-6560/aada6d. PMID: 30109989.
Article9. Spadea MF, Pileggi G, Zaffino P, Salome P, Catana C, Izquierdo-Garcia D, et al. 2019; Deep convolution neural network (DCNN) multiplane approach to synthetic CT generation From MR images-application in brain proton therapy. Int J Radiat Oncol Biol Phys. 105:495–503. DOI: 10.1016/j.ijrobp.2019.06.2535. PMID: 31271823.
Article10. Maspero M, Bentvelzen LG, Savenije MHF, Guerreiro F, Seravalli E, Janssens GO, et al. 2020; Deep learning-based synthetic CT generation for paediatric brain MR-only photon and proton radiotherapy. Radiother Oncol. 153:197–204. DOI: 10.1016/j.radonc.2020.09.029. PMID: 32976877.
Article11. Qi M, Li Y, Wu A, Jia Q, Li B, Sun W, et al. 2020; Multi-sequence MR image-based synthetic CT generation using a generative adversarial network for head and neck MRI-only radiotherapy. Med Phys. 47:1880–1894. DOI: 10.1002/mp.14075. PMID: 32027027.
Article12. Kang SK, An HJ, Jin H, Kim JI, Chie EK, Park JM, et al. 2021; Synthetic CT generation from weakly paired MR images using cycle-consistent GAN for MR-guided radiotherapy. Biomed Eng Lett. 11:263–271. DOI: 10.1007/s13534-021-00195-8. PMID: 34350052. PMCID: PMC8316520.
Article13. Boulanger M, Nunes JC, Chourak H, Largent A, Tahri S, Acosta O, et al. 2021; Deep learning methods to generate synthetic CT from MRI in radiotherapy: a literature review. Phys Med. 89:265–281. DOI: 10.1016/j.ejmp.2021.07.027. PMID: 34474325.
Article14. Kataria T, Sharma K, Subramani V, Karrthick KP, Bisht SS. 2012; Homogeneity Index: an objective tool for assessment of conformal radiation treatments. J Med Phys. 37:207–213. DOI: 10.4103/0971-6203.103606. PMID: 23293452. PMCID: PMC3532749.
Article15. Feuvret L, Noël G, Mazeron JJ, Bey P. 2006; Conformity index: a review. Int J Radiat Oncol Biol Phys. 64:333–342. DOI: 10.1016/j.ijrobp.2005.09.028. PMID: 16414369.
Article16. Iglewicz B, Hoaglin DC. 1993. How to detect and handle outliers. ASQC Quality Press;Milwaukee:17. Boldrini L, Cusumano D, Cellini F, Azario L, Mattiucci GC, Valentini V. 2019; Online adaptive magnetic resonance guided radiotherapy for pancreatic cancer: state of the art, pearls and pitfalls. Radiat Oncol. 14:71. DOI: 10.1186/s13014-019-1275-3. PMID: 31036034. PMCID: PMC6489212.
Article18. Jin H, Kim DY, Park JM, Kang HC, Chie EK, An HJ. 2019; Dosimetric effects of air pocket during magnetic resonance-guided adaptive radiation therapy for pancreatic cancer. Prog Med Phys. 30:104–111. DOI: 10.14316/pmp.2019.30.4.104.
Article19. Michalet M, Bordeau K, Cantaloube M, Valdenaire S, Debuire P, Simeon S, et al. 2022; Stereotactic MR-guided radiotherapy for pancreatic tumors: dosimetric benefit of adaptation and first clinical results in a prospective registry study. Front Oncol. 12:842402. DOI: 10.3389/fonc.2022.842402. PMID: 35356227. PMCID: PMC8959839.
Article20. Werensteijn-Honingh AM, Kroon PS, Winkel D, Aalbers EM, van Asselen B, Bol GH, et al. 2019; Feasibility of stereotactic radiotherapy using a 1.5 T MR-linac: multi-fraction treatment of pelvic lymph node oligometastases. Radiother Oncol. 134:50–54. DOI: 10.1016/j.radonc.2019.01.024. PMID: 31005224.
Article21. Bohoudi O, Bruynzeel AME, Senan S, Cuijpers JP, Slotman BJ, Lagerwaard FJ, et al. 2017; Fast and robust online adaptive planning in stereotactic MR-guided adaptive radiation therapy (SMART) for pancreatic cancer. Radiother Oncol. 125:439–444. DOI: 10.1016/j.radonc.2017.07.028. PMID: 28811038.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dosimetric Effects of Air Pocket during Magnetic Resonance-Guided Adaptive Radiation Therapy for Pancreatic Cancer
- A Study on Rebuildup of 6MV X-ray by the Cavity
- Image-guided radiation therapy in lymphoma management
- Systemic Air Embolism after CT-guided Transthoracic Needle Biopsy
- A study on the comparision of various imaging methods for the staging of renal cell carcinoma