Investig Magn Reson Imaging.
2019 Dec;23(4):367-373. 10.13104/imri.2019.23.4.367.
Primary Pelvic Peritoneal Yolk Sac Tumor in the Post-Pubertal Female: a Case Report with Literature Review
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Seoul Hospital, Seoul, Korea. demian3923@naver.com
- 2Department of Pathology, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 3Department of Obstetrics and Gynecology, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- KMID: 2468054
- DOI: http://doi.org/10.13104/imri.2019.23.4.367
Abstract
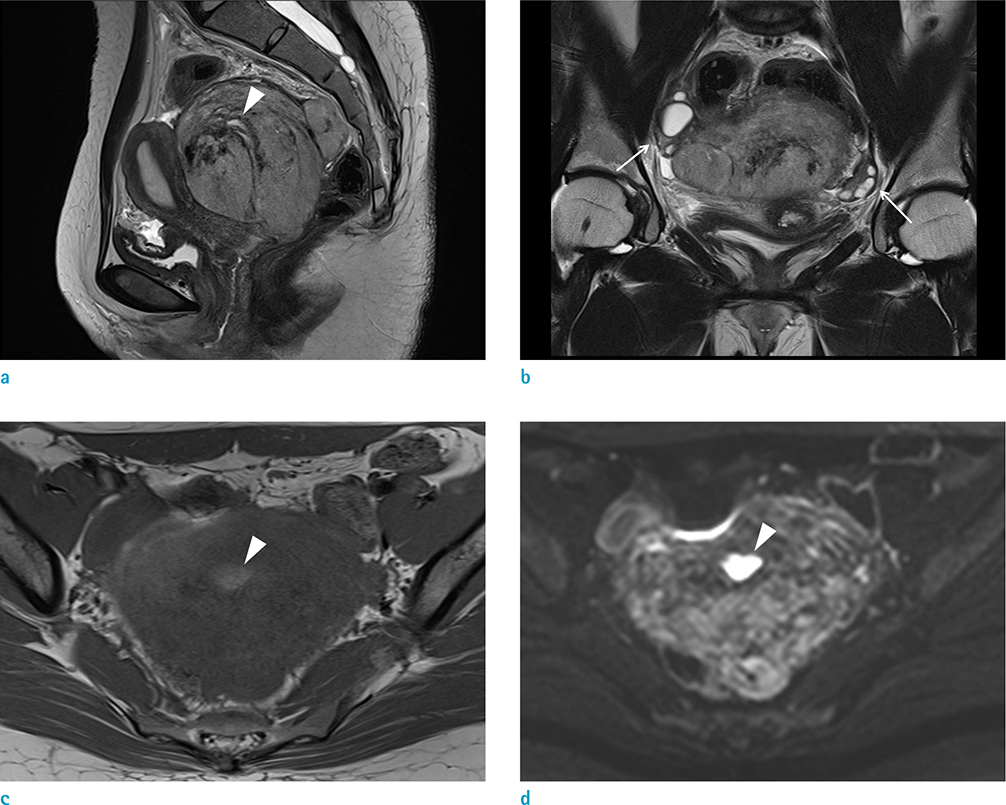
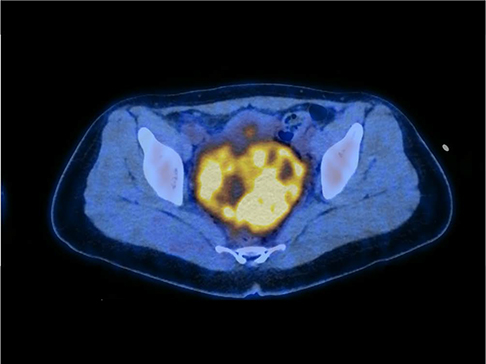
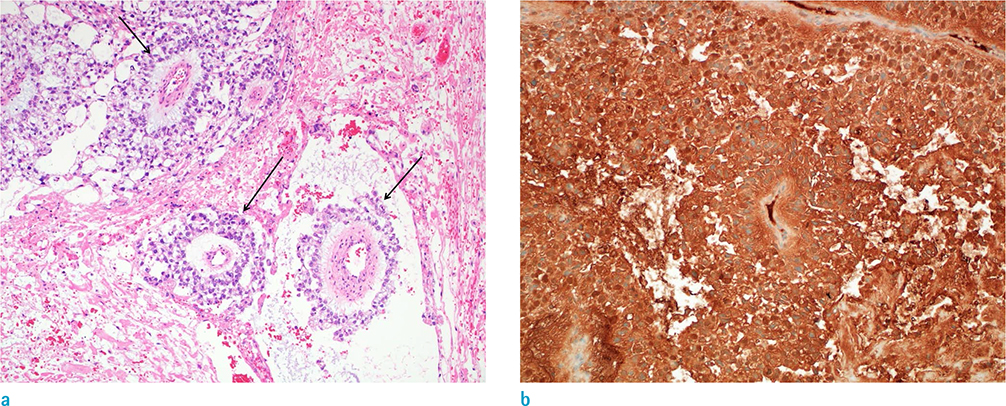
- Yolk sac tumors are rare malignant germ cell neoplasms that usually arise from the gonads. Extragonadal yolk sac tumors (EGYSTs) frequently occur in the mediastinum in post-pubertal females. EGYSTs in the pelvis are extremely rare, and to date, only thirteen cases have been reported in the English literature. Among them, the primary EGYST of the pelvic peritoneum in post-pubertal females has only been reported in ten cases. The present case describes a 26-year-old female diagnosed with primary peritoneal yolk sac tumor located in the rectouterine pouch. We report clinical and tumor imaging features, including ultrasound, computed tomography (CT), magnetic resonance images (MRI), positron emission tomography-computed tomography (PET-CT), and present a review of the literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Gilbert KL, Bergman S, Dodd LG, Volmar KE, Creager AJ. Cytomorphology of yolk sac tumor of the liver in fine-needle aspiration: a pediatric case. Diagn Cytopathol. 2006; 34:421–423.2. Huntington RW Jr, Bullock WK. Yolk sac tumors of extragonadal origin. Cancer. 1970; 25:1368–1376.3. Thiele J, Castro S, Lee KD. Extragonadal endodermal sinus tumor (yolk sac tumor) of the pelvis. Cancer. 1971; 27:391–396.4. Clement PB, Young RH, Scully RE. Extraovarian pelvic yolk sac tumors. Cancer. 1988; 62:620–626.5. Dede M, Pabuccu R, Yagci G, Yenen MC, Goktolga U, Gunhan O. Extragonadal yolk sac tumor in pelvic localization. A case report and literature review. Gynecol Oncol. 2004; 92:989–999.6. Tseng MJ, Jung SM. Primary extra-gonadal yolk-sac tumour of pelvis with unusual presentation. Lancet Oncol. 2007; 8:179–180.7. Pasternack T, Shaco-Levy R, Wiznitzer A, Piura B. Extraovarian pelvic yolk sac tumor: case report and review of published work. J Obstet Gynaecol Res. 2008; 34:739–744.8. Baba T, Su S, Umeoka S, et al. Advanced extragonadal yolk sac tumor serially followed up with (18)F-fluorodexyglucose-positoron emission tomography and computerized tomography and serum alpha-fetoprotein. J Obstet Gynaecol Res. 2012; 38:605–609.9. Rudaitis V, Mickys U, Katinaite J, Dulko J. Successful treatment of advanced stage yolk sac tumour of extragonadal origin: a case report and review of literature. Acta Med Litu. 2016; 23:110–116.10. Garnick MB, Canellos GP, Richie JP. Treatment and surgical staging of testicular and primary extragonadal germ cell cancer. JAMA. 1983; 250:1733–1741.11. McKenney JK, Heerema-McKenney A, Rouse RV. Extragonadal germ cell tumors: a review with emphasis on pathologic features, clinical prognostic variables, and differential diagnostic considerations. Adv Anat Pathol. 2007; 14:69–92.12. Shaaban AM, Rezvani M, Elsayes KM, et al. Ovarian malignant germ cell tumors: cellular classification and clinical and imaging features. Radiographics. 2014; 34:777–801.13. Ravishankar S, Malpica A, Ramalingam P, Euscher ED. Yolk sac tumor in extragonadal pelvic sites: still a diagnostic challenge. Am J Surg Pathol. 2017; 41:1–11.14. Wang M, Jiang S, Zhang Y, et al. The application of 18F-FDG PET/CT in ovarian immature teratomas when pathological examination results contradict clinical observations: a case report. Medicine (Baltimore). 2017; 96:e9171.15. Takehara K, Konishi H, Kojima A, et al. SUV max of FDG-PET/CT as a prognostic factor in ovarian clear cell adenocarcinoma. J Clin Oncol. 2014; 32:e16509.