Asian Oncol Nurs.
2019 Dec;19(4):204-213. 10.5388/aon.2019.19.4.204.
Oxaliplatin-induced Peripheral Neuropathy, Symptoms, Distress and Quality of Life among Korean Patients with Gastrointestinal Cancer
- Affiliations
-
- 1Department of Nursing, Graduate School of Yonsei University, Seoul, Korea.
- 2Department of Nursing, Yonsei University College of Nursing, Seoul, Korea. shchu@yuhs.ac
- 3Division of Medical Oncology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Mo-Im Kim Nursing Research Institute, Yonsei University College of Nursing, Seoul, Korea.
- KMID: 2467635
- DOI: http://doi.org/10.5388/aon.2019.19.4.204
Abstract
- PURPOSE
This study was conducted to identify the level of oxaliplatin-induced peripheral neuropathy (OIPN), symptoms, distress, and quality of life (QoL) in gastrointestinal (GI) cancer patients and to identify the factors influencing QoL.
METHODS
A total of 123 patients were recruited for this cross-sectional study. Surveys used were the Therapy-Induced Neuropathy Assessment Scale (TNAS) for OIPN, the MD Anderson Symptom Inventory (MDASI-GI) for general symptoms associated with gastrointestinal cancer and its treatment, a distress thermometer, and the Euro Quality of Life Questionnaire 5-Dimensional Classification (EQ-5D) for QoL.
RESULTS
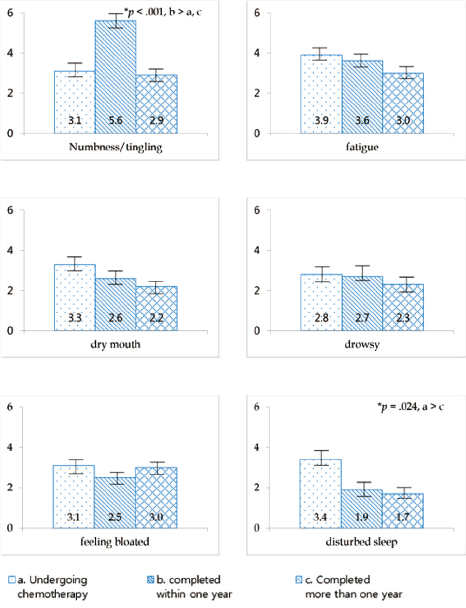
The patients were classified into three groups based on their treatment completion time (current, completed less than one year ago, completed more than one year ago). The scores of MDASI-GI and distress were significantly lower in patients who had completed chemotherapy compared to those who were undergoing treatment (p=.04 and .02 respectively). However, TNAS score was significantly higher in patients who completed chemotherapy less than one year ago than the other two groups (p=.001). In multivariate regression models, the OIPN and distress or general symptoms were identified as factors associated with QoL.
CONCLUSION
In this study, we identified the symptoms that are factors related to the QoL in patients with GI cancer. In particular, the symptoms of OIPN are reported at significantly increased levels for patients who have finished chemotherapy less than one year ago, so efforts to prevent and manage the symptoms of OIPN are needed in this timeframe. To improve QoL of patients with GI cancer, continuous attention and care are required not only during the treatment of cancer but also after the completion of treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. National Cancer Information Center. Cancer facts and figures [Internet]. Accessed June 1, 2019. Available from: https://www.cancer.go.kr.2. Mols F, Beijers T, Vreugdenhil G, van de Poll-Franse L. Chemotherapy-induced peripheral neuropathy and its association with quality of life: a systematic review. Support Care Cancer. 2014; 22:2261–2269.
Article3. Esther Kim JE, Dodd MJ, Aouizerat BE, Jahan T, Miaskowski C. A review of the prevalence and impact of multiple symptoms in oncology patients. J Pain Symptom Manage. 2009; 37:715–736.
Article4. de Gramont A, Figer A, Seymour M, Homerin M, Hmissi A, Cassidy J, et al. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol. 2000; 18:2938–2947.
Article5. Sereno M, Gutiérrez-Gutiérrez G, Gómez-Raposo C, López-Gómez M, Merino-Salvador M, Tébar FZ, et al. Oxaliplatin induced-neuropathy in digestive tumors. Crit Rev Oncol Hematol. 2014; 89:166–178.
Article6. Bennett BK, Park SB, Lin CS, Friedlander ML, Kiernan MC, Goldstein D. Impact of oxaliplatin-induced neuropathy: a patient perspective. Support Care Cancer. 2012; 20:2959–2967.
Article7. André T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol. 2009; 27:3109–3116.
Article8. Kolb NA, Smith AG, Singleton JR, Beck SL, Stoddard GJ, Brown S, et al. The association of chemotherapy-induced peripheral neuropathy symptoms and the risk of falling. JAMA Neurol. 2016; 73:860–866.
Article9. Tofthagen C, Donovan KA, Morgan MA, Shibata D, Yeh Y. Oxaliplatin-induced peripheral neuropathy’s effects on health-related quality of life of colorectal cancer survivors. Support Care Cancer. 2013; 21:3307–3313.
Article10. Oh PJ, Lim SY. Change of cancer symptom, depression and quality of life based on phases of chemotherapy in patients with colorectal or stomach cancer: a prospective study. Korean J Adult Nurs. 2017; 29:313–322.
Article11. National Comprehensive Cancer Network (NCCN). NCCN guidelines for distress management, version 2.2018 [Internet]. June 1, 2019. Available from: https://www.nccn.org/professionals/physician_gls/f_guidelines.asp#supportive.12. Kwon EJ, Yi M. Distress and quality of life in breast cancer survivors in Korea. Asian Oncol Nurs. 2012; 12:289–296.
Article13. Kim KY, Lee SH, Kim JH, Oh PJ. Disturbance in ADL from chemotherapy-induced peripheral neuropathy and quality of life in cancer patients: the mediating effect of psychological distress. J Korean Acad Nurs. 2015; 45:661–670.
Article14. Baek Y, Yi M. Factors influencing quality of life during chemotherapy for colorectal cancer patients in South Korea. J Korean Acad Nurs. 2015; 45:604–612.
Article15. Yang YH. The relationship of symptoms of side effects, fatigue and quality of life in stomach cancer patients receiving chemotherapy. J Korean Acad Adult Nurs. 2002; 14:205–212.16. Padman S, Lee J, Kumar R, Slee M, Hakendorf P, Richards A, et al. Late effects of oxaliplatin-induced peripheral neuropathy (LEON)--cross-sectional cohort study of patients with colorectal cancer surviving at least 2 years. Support Care Cancer. 2015; 23:861–869.
Article17. Lee JY. Assessment and comparison of utility for heart failure using VAS (visual analogue scale), TTO (time trade-off), and EQ-5D (Euro-Qol-5 dimensions) [dissertation]. Seoul: Sungkyunkwan Univ.;2016.18. Kim TH. Validity and reliability evaluation for EQ-5D in the general population of south Korea [dissertation]. Ulsan: Ulsan National University;2012.19. Mendoza TR, Wang XS, Williams LA, Shi Q, Vichaya EG, Dougherty PM, et al. Measuring therapy-induced peripheral neuropathy: preliminary development and validation of the treatment-induced neuropathy assessment scale. J Pain. 2015; 16:1032–1043.
Article20. Wang XS, Williams LA, Eng C, Mendoza TR, Shah NA, Kirkendoll KJ, et al. Validation and application of a module of the M. D. Anderson Symptom Inventory for measuring multiple symptoms in patients with gastrointestinal cancer (the MDASI-GI). Cancer. 2010; 116:2053–2063.
Article21. Donovan KA, Grassi L, McGinty HL, Jacobsen PB. Validation of the distress thermometer worldwide: state of the science. Psychooncology. 2014; 23:241–250.
Article22. Kim SH, Kim W, Kim JH, Woo MK, Baek JY, Kim SY, et al. A prospective study of chronic oxaliplatin-induced neuropathy in patients with colon cancer: long-term outcomes and predictors of severe oxaliplatininduced neuropathy. J Clin Neurol. 2018; 14:81–89.
Article23. Ezendam NP, Pijlman B, Bhugwandass C, Pruijt JF, Mols F, Vos MC, et al. Chemotherapy-induced peripheral neuropathy and its impact on health-related quality of life among ovarian cancer survivors: results from the population-based PROFILES registry. Gynecol Oncol. 2014; 135:510–517.
Article24. Bao T, Basal C, Seluzicki C, Li SQ, Seidman AD, Mao JJ. Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence, risk factors, and fall risk. Breast Cancer Res Treat. 2016; 159:327–333.
Article25. Curt GA, Breitbart W, Cella D, Groopman JE, Horning SJ, Itri LM, et al. Impact of cancer-related fatigue on the lives of patients: new findings from the Fatigue Coalition. Oncologist. 2000; 5:353–360.
Article26. Kroenke K, Johns SA, Theobald D, Wu J, Tu W. Somatic symptoms in cancer patients trajectory over 12 months and impact on functional status and disability. Support Care Cancer. 2013; 21:765–773.
Article27. Kim YS, Tae YS, Nam GH. Distress and quality of life among elderly patients with gastric cancer: the mediating effect of social support. Korean J Adult Nurs. 2017; 29:536–546.
Article28. Kim JG, Kwon LS. Measurement of quality of life related to health by demographic characteristics of adult patients with cancer using EQ-5D Index: focused on the Korea Health & Nutrition Examination Survey. J Digit Policy Manag. 2013; 11:281–291.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Disturbance in ADL from Chemotherapy-induced Peripheral Neuropathy and Quality of Life in Cancer Patients: The Mediating Effect of Psychological Distress
- The Effects of Foot Reflexology on Peripheral Neuropathy, Symptom Distress, Anxiety and Depression in Cancer Patients Treated with Oxaliplatin
- Changes in Chemotherapy-induced Peripheral Neuropathy, Sleep Quality, and Quality of Life following Chemotherapy in Stomach Cancer Patients: a Prospective Study
- Oxaliplatin-Induced Peripheral Neuropathy and Quality of Life in Patients with Digestive System Cancer
- Characteristics and Quality of Life in Gynecologic Cancer Patients with Chemotherapy-induced Peripheral Neuropathy