Acute Crit Care.
2019 Nov;34(4):255-262. 10.4266/acc.2019.00640.
The association between the initial lactate level and need for massive transfusion in severe trauma patients with and without traumatic brain injury
- Affiliations
-
- 1Department of Emergency Medicine, Chonnam National University Hospital, Gwangju, Korea. ggodhkekf@hanmail.net
- KMID: 2467304
- DOI: http://doi.org/10.4266/acc.2019.00640
Abstract
- BACKGROUND
Exsanguination is a major cause of death in severe trauma patients. The purpose of this study was to analyze the prognostic impact of the initial lactate level for massive transfusion (MT) in severe trauma. We divided patients according to subgroups of traumatic brain injury (TBI) and non-TBI.
METHODS
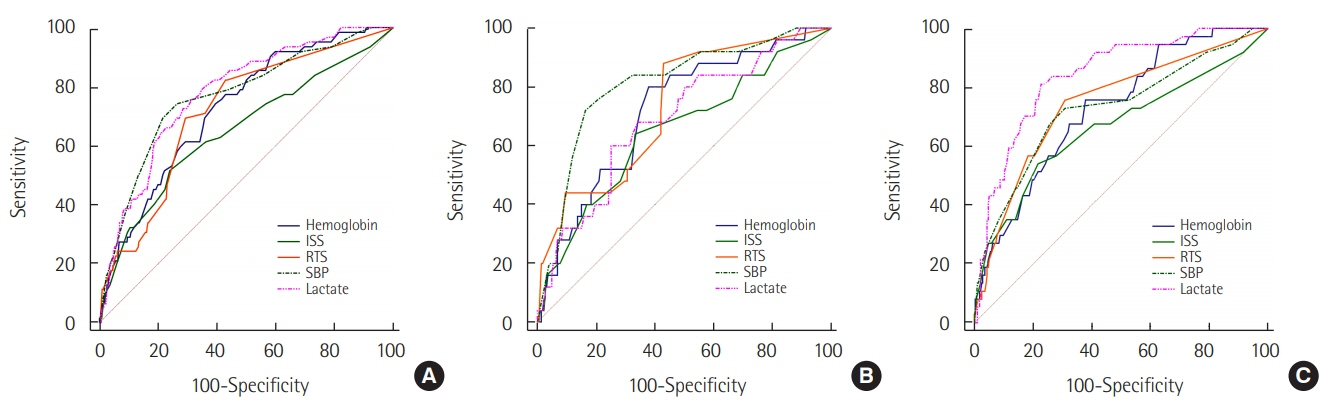
This single-institution retrospective study was conducted on patients who were admitted to hospital for severe trauma between January 2016 and December 2017. TBI was defined by a head Abbreviated Injury Scale ≥3. Receiver operating characteristic analysis was used to analyze the prognostic impact of the lactate level. Multivariate analyses were performed to evaluate the relationship between the MT and lactate level. The primary outcome was MT.
RESULTS
Of the 553 patients, MT was performed in 62 patients (11.2%). The area under the curve (AUC) for the lactate level for predicting MT was 0.779 (95% confidence interval [CI], 0.742 to 0.813). The AUCs for lactate level in the TBI and non-TBI patients were 0.690 (95% CI, 0.627 to 0.747) and 0.842 (95% CI, 0.796 to 0.881), respectively. In multivariate analyses, the lactate level was independently associated with the MT (odds ratio [OR], 1.179; 95% CI, 1.070 to 1.299). The lactate level was independently associated with MT in non-TBI patients (OR, 1.469; 95% CI, 1.262 to 1.710), but not in TBI patients.
CONCLUSIONS
The initial lactate level may be a possible prognostic factor for MT in severe trauma. In TBI patients, however, the initial lactate level was not suitable for predicting MT.
Keyword
MeSH Terms
Figure
Reference
-
1. Lefering R, Paffrath T, Bouamra O, Coats TJ, Woodford M, Jenks T, et al. Epidemiology of in-hospital trauma deaths. Eur J Trauma Emerg Surg. 2012; 38:3–9.
Article2. Brown JB, Gestring ML, Forsythe RM, Stassen NA, Billiar TR, Peitzman AB, et al. Systolic blood pressure criteria in the National Trauma Triage Protocol for geriatric trauma: 110 is the new 90. J Trauma Acute Care Surg. 2015; 78:352–9.3. Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma. 2006; 60(6 Suppl):S3–11.
Article4. Johnson JJ, Garwe T, Albrecht RM, Adeseye A, Bishop D, Fails RB, et al. Initial inferior vena cava diameter on computed tomographic scan independently predicts mortality in severely injured trauma patients. J Trauma Acute Care Surg. 2013; 74:741–6.
Article5. Hagiwara A, Kushimoto S, Kato H, Sasaki J, Ogura H, Matsuoka T, et al. Can early aggressive administration of fresh frozen plasma improve outcomes in patients with severe blunt trauma?: a report by the Japanese Association for the Surgery of Trauma. Shock. 2016; 45:495–501.6. Odell DD, Liao K. Superior vena cava and innominate vein reconstruction in thoracic malignancies: double-vein reconstruction. Semin Thorac Cardiovasc Surg. 2011; 23:326–9.
Article7. Jansen TC, van Bommel J, Schoonderbeek FJ, Sleeswijk Visser SJ, van der Klooster JM, Lima AP, et al. Early lactate-guided therapy in intensive care unit patients: a multicenter, openlabel, randomized controlled trial. Am J Respir Crit Care Med. 2010; 182:752–61.8. Lyu X, Xu Q, Cai G, Yan J, Yan M. Efficacies of fluid resuscitation as guided by lactate clearance rate and central venous oxygen saturation in patients with septic shock. Zhonghua Yi Xue Za Zhi. 2015; 95:496–500.9. Liang D, Zhou X, Hong X, Feng X, Shan P, Xie Q, et al. Association between admission lactate levels and mortality in patients with acute coronary syndrome: a retrospective cohort study. Coron Artery Dis. 2019; 30:26–32.10. Dekker SE, de Vries HM, Lubbers WD, van de Ven PM, Toor EJ, Bloemers FW, et al. Lactate clearance metrics are not superior to initial lactate in predicting mortality in trauma. Eur J Trauma Emerg Surg. 2017; 43:841–51.
Article11. Johnson MC, Alarhayem A, Convertino V, Carter R 3rd, Chung K, Stewart R, et al. Comparison of compensatory reserve and arterial lactate as markers of shock and resuscitation. J Trauma Acute Care Surg. 2017; 83:603–8.
Article12. Namas R, Ghuma A, Hermus L, Zamora R, Okonkwo DO, Billiar TR, et al. The acute inflammatory response in trauma/hemorrhage and traumatic brain injury: current state and emerging prospects. Libyan J Med. 2009; 4:97–103.13. Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974; 14:187–96.14. Mellick D, Gerhart KA, Whiteneck GG. Understanding outcomes based on the post-acute hospitalization pathways followed by persons with traumatic brain injury. Brain Inj. 2003; 17:55–71.
Article15. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–45.
Article16. Vandromme MJ, Griffin RL, Weinberg JA, Rue LW 3rd, Kerby JD. Lactate is a better predictor than systolic blood pressure for determining blood requirement and mortality: could prehospital measures improve trauma triage? J Am Coll Surg. 2010; 210:861–9.
Article17. Brooke M, Yeung L, Miraflor E, Garcia A, Victorino GP. Lactate predicts massive transfusion in hemodynamically normal patients. J Surg Res. 2016; 204:139–44.
Article18. Dekker SE, Duvekot A, de Vries HM, Geeraedts LM Jr, Peerdeman SM, de Waard MC, et al. Relationship between tissue perfusion and coagulopathy in traumatic brain injury. J Surg Res. 2016; 205:147–54.
Article19. Tian HL, Chen H, Wu BS, Cao HL, Xu T, Hu J, et al. D-dimer as a predictor of progressive hemorrhagic injury in patients with traumatic brain injury: analysis of 194 cases. Neurosurg Rev. 2010; 33:359–66.
Article20. Spinella PC, Holcomb JB. Resuscitation and transfusion principles for traumatic hemorrhagic shock. Blood Rev. 2009; 23:231–40.
Article21. Patet C, Suys T, Carteron L, Oddo M. Cerebral lactate metabolism after traumatic brain injury. Curr Neurol Neurosci Rep. 2016; 16:31.
Article22. Sala N, Suys T, Zerlauth JB, Bouzat P, Messerer M, Bloch J, et al. Cerebral extracellular lactate increase is predominantly nonischemic in patients with severe traumatic brain injury. J Cereb Blood Flow Metab. 2013; 33:1815–22.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Trauma Patients with Massive Transfusion in the Emergency Department
- The relationship between the serum lactate level and in-hospital mortality after decompressive craniectomy in traumatic brain Injury
- A Simple Comment of Trauma-Induced Coagulopathy and Massive Transfusion
- Surgical Outcomes in Patients with Simultaneous Traumatic Brain and Torso Injuries in a Single Regional Trauma Center over a 5-Year Period
- Animal Models of Traumatic Brain Injury