Carbapenem-resistant Enterobacteriaceae: Prevalence and Risk Factors in a Single Community-Based Hospital in Korea
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. jhyoo@catholic.ac.kr
- 2Vaccine Bio Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2466428
- DOI: http://doi.org/10.3947/ic.2016.48.3.166
Abstract
- BACKGROUND
Carbapenemase-producing Enterobacteriaceae (CPE) are Gram-negative bacteria with increasing prevalence of infection worldwide. In Korea, 25 cases of CPE isolates were reported by the Korea Centers for Disease Control and Prevention in 2011. Most CPE cases were detected mainly at tertiary referral hospitals. We analyzed the prevalence and risk factors for carbapenem-resistant Enterobacteriaceae (CRE) in a mid-sized community-based hospital in Korea.
MATERIALS AND METHODS
We retrospectively analyzed all consecutive episodes of Enterobacteriaceae in a mid-sized community-based hospital from January 2013 to February 2014. CRE was defined as organisms of Enterobacteriaceae showing decreased susceptibility to carbapenems. Risk factors for CRE were evaluated by a case-double control design. Carbapenemase was confirmed for CRE using a combined disc test.
RESULTS
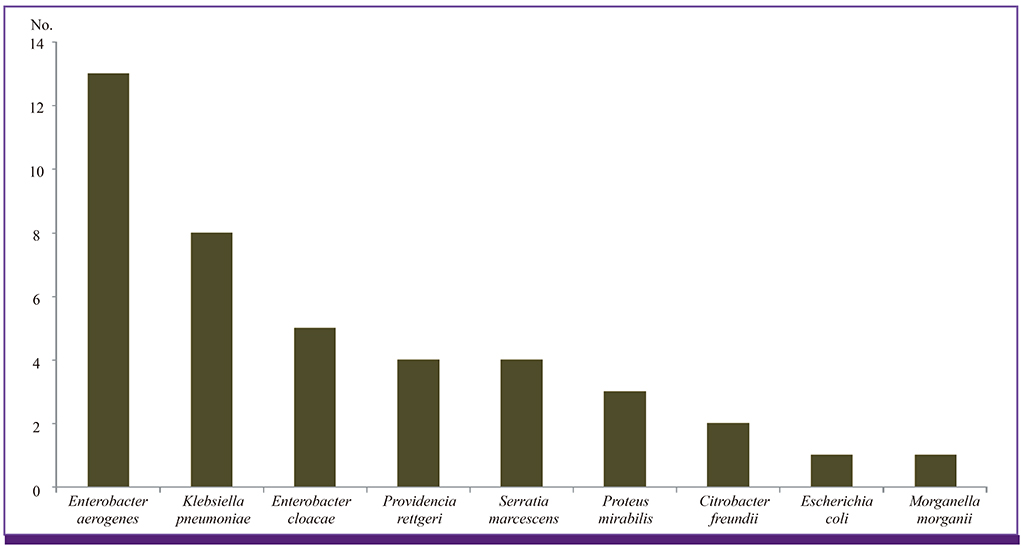
During 229,710 patient-days, 2,510 Enterobacteriaceae isolates were obtained. A total of 41 (1.6%) CRE isolates were enrolled in the study period. Thirteen species (31.7%) were Enterobacter aerogenes, 8 (19.5%) Klebsiella pneumoniae, 5 (12.2%) Enterobacter cloacae, and 15 other species of Enterobacteriaceae, respectively. Among the 41 isolates, only one (2.4%) E. aerogenes isolate belonged to CPE. For evaluation of risk factors, a total of 111 patients were enrolled and this included 37 patients in the CRE group, 37 in control group I (identical species), and 37 in control group II (different species). Based on multivariate analysis, regularly visiting the outpatient clinic was a risk factor for CRE acquisition in the control group I (P = 0.003), while vascular catheter and Charlson comorbidity index score ≥ 3 were risk factors in control group II (P = 0.010 and 0.011, each). Patients with CRE were more likely to experience a reduced level of consciousness, use a vasopressor, be under intensive care, and suffer from acute kidney injury. However, CRE was not an independent predictor of mortality compared with both control groups.
CONCLUSION
In conclusion, the prevalence of CRE was higher than expected in a mid-sized community-based hospital in Korea. CRE should be considered when patients have a vascular catheter, high comorbidity score, and regular visits to the outpatient clinic. This study suggests the need for appropriate prevention efforts and constant attention to CRE infection control in a mid-sized community-based hospital.
MeSH Terms
-
Acute Kidney Injury
Ambulatory Care Facilities
Carbapenems
Centers for Disease Control and Prevention (U.S.)
Comorbidity
Consciousness
Critical Care
Drug Resistance
Enterobacter aerogenes
Enterobacter cloacae
Enterobacteriaceae*
Gram-Negative Bacteria
Humans
Infection Control
Klebsiella pneumoniae
Korea*
Mortality
Multivariate Analysis
Prevalence*
Retrospective Studies
Risk Factors*
Tertiary Care Centers
Vascular Access Devices
Carbapenems
Figure
Cited by 5 articles
-
Are Community-Based Hospitals Safe from Carbapenem-Resistant Enterobacteriaceae in Korea?
Chang-Seop Lee
Infect Chemother. 2016;48(3):246-248. doi: 10.3947/ic.2016.48.3.246.Establishment of Experimental Murine Peritonitis Model with Hog Gastric Mucin for Carbapenem-Resistant Gram-Negative Bacteria
Jung Yeon Park, Chulmin Park, Hye-Sun Chun, Ji-Hyun Byun, Sung-Yeon Cho, Dong-Gun Lee
Infect Chemother. 2017;49(1):57-61. doi: 10.3947/ic.2017.49.1.57.MCR1 and KPC2 Co-producing Klebsiella pneumoniae Bacteremia: First Case in Korea
Ji Young Park, Sang Taek Heo, Ki Tae Kwon, Do Young Song, Kwang Jun Lee, Ji Ae Choi
Infect Chemother. 2019;51(4):399-404. doi: 10.3947/ic.2019.51.4.399.Carbapenem-resistant
Enterobacteriaceae : recent updates and treatment strategies
Hyo-Jin Lee, Dong-Gun Lee
J Korean Med Assoc. 2018;61(4):281-289. doi: 10.5124/jkma.2018.61.4.281.Outbreak of Carbapenem-resistant
Enterobacteriaceae (CRE) in a Long-term Acute Care Facility in the Republic of Korea
Sunwha Jung, Sangshin Park
Korean J Healthc Assoc Infect Control Prev. 2022;27(1):43-50. doi: 10.14192/kjicp.2022.27.1.43.
Reference
-
1. Wang JT, Wu UI, Lauderdale TL, Chen MC, Li SY, Hsu LY, Chang SC. Carbapenem-nonsusceptible Enterobacteriaceae in Taiwan. PLoS One. 2015; 10:e0121668.
Article2. Kaniga K, Flamm R, Tong SY, Lee M, Friedland I, Redman R. Worldwide experience with the use of doripenem against extended-spectrum-β-lactamase-producing and ciprofloxacin-resistant Enterobacteriaceae: analysis of six phase 3 clinical studies. Antimicrob Agents Chemother. 2010; 54:2119–2124.
Article3. Ling ML, Tee YM, Tan SG, Amin IM, How KB, Tan KY, Lee LC. Risk factors for acquisition of carbapenem resistant Enterobacteriaceae in an acute tertiary care hospital in Singapore. Antimicrob Resist Infect Control. 2015; 4:26.
Article4. Xu Y, Gu B, Huang M, Liu H, Xu T, Xia W, Wang T. Epidemiology of carbapenem resistant Enterobacteriaceae (CRE) during 2000-2012 in Asia. J Thorac Dis. 2015; 7:376–385.5. Schwaber MJ, Klarfeld-Lidji S, Navon-Venezia S, Schwartz D, Leavitt A, Carmeli Y. Predictors of carbapenem-resistant Klebsiella pneumoniae acquisition among hospitalized adults and effect of acquisition on mortality. Antimicrob Agents Chemother. 2008; 52:1028–1033.
Article6. Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008; 29:1099–1106.
Article7. Patel N, Harrington S, Dihmess A, Woo B, Masoud R, Martis P, Fiorenza M, Graffunder E, Evans A, McNutt LA, Lodise TP. Clinical epidemiology of carbapenem-intermediate or -resistant Enterobacteriaceae. J Antimicrob Chemother. 2011; 66:1600–1608.
Article8. Lee K, Lee HS, Jang SJ, Park AJ, Lee MH, Song WK, Chong Y. Members of Korean Nationwide Surveillance ofAntimicrobial Resistance Group. Antimicrobial resistance surveillance of bacteria in 1999 in Korea with a special reference to resistance of enterococci to vancomycin and gram-negative bacilli to third generation cephalosporin, imipenem, and fluoroquinolone. J Korean Med Sci. 2001; 16:262–270.
Article9. Kwak YG, Choi SH, Choo EJ, Chung JW, Jeong JY, Kim NJ, Woo JH, Ryu J, Kim YS. Risk factors for the acquisition of carbapenem-resistant Klebsiella pneumoniae among hospitalized patients. Microb Drug Resist. 2005; 11:165–169.
Article10. Lee H, Ko KS, Song JH, Peck KR. Antimicrobial activity of doripenem and other carbapenems against gram-negative pathogens from Korea. Microb Drug Resist. 2011; 17:37–45.
Article11. Gómez Rueda V, Zuleta Tobón JJ. Risk factors for infection with carbapenem-resistant Klebsiella pneumoniae: a case-case-control study. Colomb Med (Cali). 2014; 45:54–60.12. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.
Article13. Kim J, Lee JY, Kim SI, Song W, Kim JS, Jung S, Yu JK, Park KG, Park YJ. Rates of fecal transmission of extended-spectrum β-lactamase-producing and carbapenem-resistant Enterobacteriaceae among patients in intensive care units in Korea. Ann Lab Med. 2014; 34:20–25.
Article14. Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing: Twenty-second informational supplement M100-S22. CLSI: Wayne, PA;2012.15. Chang YY, Chuang YC, Siu LK, Wu TL, Lin JC, Lu PL, Wang JT, Wang LS, Lin YT, Huang LJ, Fung CP. Clinical features of patients with carbapenem nonsusceptible Klebsiella pneumoniae and Escherichia coli in intensive care units: a nationwide multicenter study in Taiwan. J Microbiol Immunol Infect. 2015; 48:219–225.
Article16. Logan LK, Renschler JP, Gandra S, Weinstein RA, Laxminarayan R; Centers for Disease Control. Prevention Epicenters Program. Carbapenem-resistant Enterobacteriaceae in children, United States, 1999-2012. Emerg Infect Dis. 2015; 21:2014–2021.
Article17. Anderson KF, Lonsway DR, Rasheed JK, Biddle J, Jensen B, McDougal LK, Carey RB, Thompson A, Stocker S, Limbago B, Patel JB. Evaluation of methods to identify the Klebsiella pneumoniae carbapenemase in Enterobacteriaceae . J Clin Microbiol. 2007; 45:2723–2725.
Article18. Ampaire LM, Katawera V, Nyehangane D, Boum Y, Bazira J. Epidemiology of carbapenem resistance among multi-drug resistant enterobacteriaceae in Uganda. Br Microbiol Res J. 2015; 8:418–423.
Article19. Torres-Gonzalez P, Cervera-Hernandez ME, Niembro-Ortega MD, Leal-Vega F, Cruz-Hervert LP, García-García L, Galindo-Fraga A, Martinez-Gamboa A, Bobadilla-Del Valle M, Sifuentes-Osornio J, Ponce-de-Leon A. Factors associated to prevalence and incidence of carbapenem-resistant Enterobacteriaceae fecal carriage: a cohort study in a Mexican Tertiary Care Hospital. PLoS One. 2015; 10:e0139883.20. Guh AY, Bulens SN, Mu Y, Jacob JT, Reno J, Scott J, Wilson LE, Vaeth E, Lynfield R, Shaw KM, Vagnone PM, Bamberg WM, Janelle SJ, Dumyati G, Concannon C, Beldavs Z, Cunningham M, Cassidy PM, Phipps EC, Kenslow N, Travis T, Lonsway D, Rasheed JK, Limbago BM, Kallen AJ. Epidemiology of carbapenem-resistant enterobacteriaceae in 7 US communities, 2012-2013. JAMA. 2015; 314:1479–1487.
Article21. Huh K, Kim J, Cho SY, Ha YE, Joo EJ, Kang CI, Chung DR, Lee NY, Song JH, Peck KR; Korean Network for Study on Infectious Diseases (KONSID). Continuous increase of the antimicrobial resistance among gram-negative pathogens causing bacteremia: a nationwide surveillance study by the Korean Network for Study on Infectious Diseases (KONSID). Diagn Microbiol Infect Dis. 2013; 76:477–482.
Article22. Kim BM, Jeon EJ, Jang JY, Chung JW, Park J, Choi JC, Shin JW, Park IW, Choi BW, Kim JY. Four year trend of carbapenem-resistance in newly opened ICUs of a university-affiliated hospital of South Korea. Tuberc Respir Dis (Seoul). 2012; 72:360–366.
Article23. Kim DK, Kim HS, Pinto N, Jeon J, D’Souza R, Kim MS, Choi JY, Yong D, Jeong SH, Lee K. Xpert CARBA-R assay for the detection of carbapenemase-producing organisms in intensive care unit patients of a Korean Tertiary Care Hospital. Ann Lab Med. 2016; 36:162–165.
Article24. Thaden JT, Pogue JM, Kaye KS. Role of newer and re-emerging older agents in the treatment of infections caused by carbapenem-resistant Enterobacteriaceae. Virulence. 2016; 6:1–14.
Article25. Sader HS, Castanheira M, Flamm RK, Mendes RE, Farrell DJ, Jones RN. Tigecycline activity tested against carbapenem-resistant Enterobacteriaceae from 18 European nations: results from the SENTRY surveillance program (2010-2013). Diagn Microbiol Infect Dis. 2015; 83:183–186.
Article26. Livermore DM, Warner M, Mushtaq S, Doumith M, Zhang J, Woodford N. What remains against carbapenem-resistant Enterobacteriaceae? Evaluation of chloramphenicol, ciprofloxacin, colistin, fosfomycin, minocycline, nitrofurantoin, temocillin and tigecycline. Int J Antimicrob Agents. 2011; 37:415–419.
Article27. Kim SY, Shin J, Shin SY, Ko KS. Characteristics of carbapenem-resistant Enterobacteriaceae isolates from Korea. Diagn Microbiol Infect Dis. 2013; 76:486–490.
Article28. Jiao Y, Qin Y, Liu J, Li Q, Dong Y, Shang Y, Huang Y, Liu R. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection/colonization and predictors of mortality: a retrospective study. Pathog Glob Health. 2015; 109:68–74.
Article29. Giannella M, Trecarichi EM, De Rosa FG, Del Bono V, Bassetti M, Lewis RE, Losito AR, Corcione S, Saffioti C, Bartoletti M, Maiuro G, Cardellino CS, Tedeschi S, Cauda R, Viscoli C, Viale P, Tumbarello M. Risk factors for carbapenem-resistant Klebsiella pneumoniae bloodstream infection among rectal carriers: a prospective observational multicentre study. Clin Microbiol Infect. 2014; 20:1357–1362.
Article30. Correa L, Martino MD, Siqueira I, Pasternak J, Gales AC, Silva CV, Camargo TZ, Scherer PF, Marra AR. A hospital-based matched case-control study to identify clinical outcome and risk factors associated with carbapenem-resistant Klebsiella pneumoniae infection. BMC Infect Dis. 2013; 13:80.31. Ahn JY, Song JE, Kim MH, Choi H, Kim JK, Ann HW, Kim JH, Jeon Y, Jeong SJ, Kim SB, Ku NS, Han SH, Song YG, Yong D, Lee K, Kim JM, Choi JY. Risk factors for the acquisition of carbapenem-resistant Escherichia coli at a tertiary care center in South Korea: a matched case-control study. Am J Infect Control. 2014; 42:621–625.
Article32. Jeon MH, Choi SH, Kwak YG, Chung JW, Lee SO, Jeong JY, Woo JH, Kim YS. Risk factors for the acquisition of carbapenem-resistant Escherichia coli among hospitalized patients. Diagn Microbiol Infect Dis. 2008; 62:402–406.
Article33. Gupta N, Limbago BM, Patel JB, Kallen AJ. Carbapenem-resistant Enterobacteriaceae: epidemiology and prevention. Clin Infect Dis. 2011; 53:60–67.34. Martirosov DM, Lodise TP. Emerging trends in epidemiology and management of infections caused by carbapenem-resistant Enterobacteriaceae. Diagn Microbiol Infect Dis. 2016; 85:266–275.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and Risk Factors for Carbapenem-Resistant Enterobacteriaceae Colonization in Patients with Stroke
- Are Community-Based Hospitals Safe from Carbapenem-Resistant Enterobacteriaceae in Korea?
- The Infinity War: How to Cope with Carbapenem-resistant Enterobacteriaceae
- Epidemiological Characteristics of Carbapenemase Producing Carbapenem-Resistant Enterobacteriaceae Colonization
- Carbapenem-Resistant Enterobacteriaceae: Rapid Laboratory Diagnosis and Surveillance Culture for Infection Control