Yonsei Med J.
2016 Jan;57(1):127-131. 10.3349/ymj.2016.57.1.127.
High Remission Rate of Chronic Immune Thrombocytopenia in Children: Result of 20-Year Follow-Up
- Affiliations
-
- 1Department of Pediatrics, Kyung Hee University Medical Center, Seoul, Korea. snoopyi@hanmail.net
- KMID: 2466361
- DOI: http://doi.org/10.3349/ymj.2016.57.1.127
Abstract
- PURPOSE
This study examined the outcomes of children with chronic immune thrombocytopenia (ITP).
MATERIALS AND METHODS
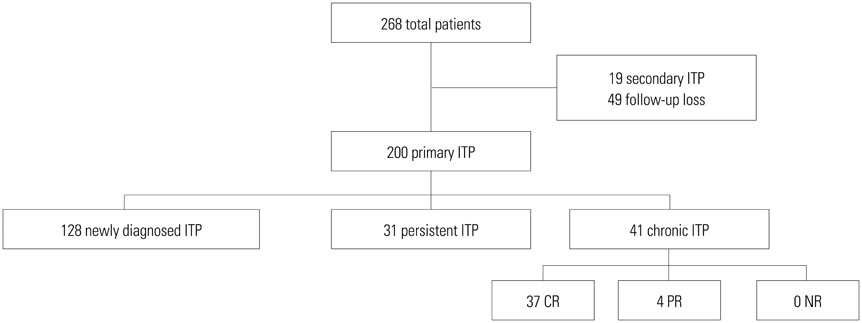
We retrospectively analyzed the medical records of all patients diagnosed with ITP from January 1992 to December 2011 at our institution.
RESULTS
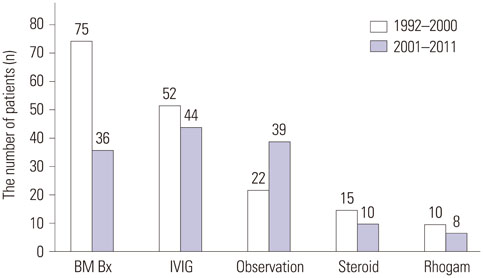
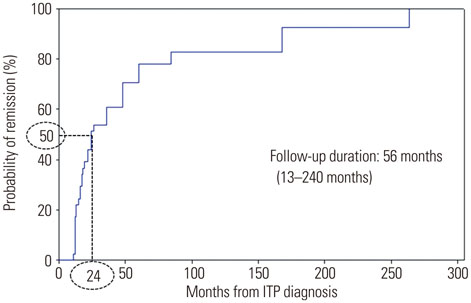
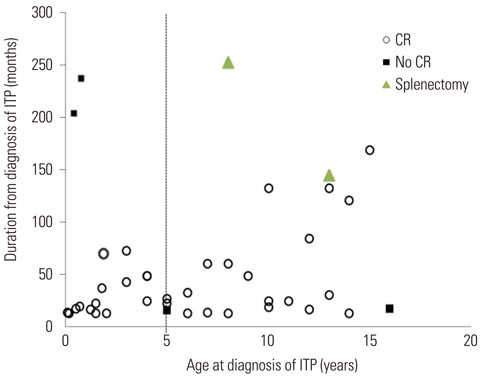
A total of 128 patients (64%) satisfied the criteria for newly diagnosed ITP, 31 (15%) for persistent ITP, and 41 (21%) for chronic ITP. The median age at diagnosis was 4.5 years (range, 1 month to 18 years). The median platelet count at diagnosis was 32x109/L. A comparison of the initial treatment data from 2001 to 2011 with those from 1992 to 2000 showed that the number of bone marrow examinations decreased, whereas observation increased. Chronic ITP presented at an older age than newly diagnosed and persistent ITP (6.6 years vs. 3.8 years vs. 4.1 years, respectively); however, the difference did not reach statistical significance (p=0.17). The probability of complete remission of chronic ITP was 50% and 76% at 2 and 5 years after diagnosis, respectively. Patients aged <1 year at diagnosis had a significantly better prognosis than did older patients (hazard ratio, 3.86; p=0.02).
CONCLUSION
Children with chronic ITP showed a high remission rate after long-term follow-up. This study suggests that invasive treatments such as splenectomy in children with chronic ITP can be delayed for 4 to 5 years if thrombocytopenia and therapeutic medication do not affect the quality of life.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Differential diagnosis of childhood hemorrhagic disorders
Hoi Soo Yoon
J Korean Med Assoc. 2016;59(9):683-689. doi: 10.5124/jkma.2016.59.9.683.
Reference
-
1. Bolton-Maggs PH. Idiopathic thrombocytopenic purpura. Arch Dis Child. 2000; 83:220–222.
Article2. Cuker A, Cines DB. Immune thrombocytopenia. Hematology Am Soc Hematol Educ Program. 2010; 2010:377–384.
Article3. ElAlfy M, Farid S, Abdel Maksoud A. Predictors of chronic idiopathic thrombocytopenic purpura. Pediatr Blood Cancer. 2010; 54:959–962.
Article4. Imbach P, Kühne T, Müller D, Berchtold W, Zimmerman S, Elalfy M, et al. Childhood ITP: 12 months follow-up data from the prospective registry I of the Intercontinental Childhood ITP Study Group (ICIS). Pediatr Blood Cancer. 2006; 46:351–356.
Article5. Kühne T, Buchanan GR, Zimmerman S, Michaels LA, Kohan R, Berchtold W, et al. A prospective comparative study of 2540 infants and children with newly diagnosed idiopathic thrombocytopenic purpura (ITP) from the Intercontinental Childhood ITP Study Group. J Pediatr. 2003; 143:605–608.
Article6. George JN, Kojouri K, Perdue JJ, Vesely SK. Management of patients with chronic, refractory idiopathic thrombocytopenic purpura. Semin Hematol. 2000; 37:290–298.
Article7. Emilia G, Messora C, Longo G, Bertesi M. Long-term salvage treatment by cyclosporin in refractory autoimmune haematological disorders. Br J Haematol. 1996; 93:341–344.
Article8. Kojouri K, Vesely SK, Terrell DR, George JN. Splenectomy for adult patients with idiopathic thrombocytopenic purpura: a systematic review to assess long-term platelet count responses, prediction of response, and surgical complications. Blood. 2004; 104:2623–2634.
Article9. Ahn YS, Harrington WJ, Mylvaganam R, Allen LM, Pall LM. Slow infusion of vinca alkaloids in the treatment of idiopathic thrombocytopenic purpura. Ann Intern Med. 1984; 100:192–196.
Article10. Bansal D, Bhamare TA, Trehan A, Ahluwalia J, Varma N, Marwaha RK. Outcome of chronic idiopathic thrombocytopenic purpura in children. Pediatr Blood Cancer. 2010; 54:403–407.
Article11. Rosthøj S, Rajantie J, Treutiger I, Zeller B, Tedgård U, Henter JI, et al. Duration and morbidity of chronic immune thrombocytopenic purpura in children: five-year follow-up of a Nordic cohort. Acta Paediatr. 2012; 101:761–766.
Article12. Shim YJ, Kim UH, Suh JK, Lee KS. Natural course of childhood chronic immune thrombocytopenia using the revised terminology and definitions of the international working group: a single center experience. Blood Res. 2014; 49:187–191.
Article13. Rodeghiero F. First-line therapies for immune thrombocytopenic purpura: re-evaluating the need to treat. Eur J Haematol Suppl. 2008; 19–26.
Article14. Rodeghiero F, Stasi R, Gernsheimer T, Michel M, Provan D, Arnold DM, et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood. 2009; 113:2386–2393.
Article15. Walker JH, Walker W. Idiopathic thrombocytopenic purpura in childhood. Arch Dis Child. 1961; 36:649–657.
Article16. Reid MM. Chronic idiopathic thrombocytopenic purpura: incidence, treatment, and outcome. Arch Dis Child. 1995; 72:125–128.
Article17. Eden OB, Lilleyman JS. Guidelines for management of idiopathic thrombocytopenic purpura. The British Paediatric Haematology Group. Arch Dis Child. 1992; 67:1056–1058.
Article18. British Committee for Standards in Haematology General Haematology Task Force. Guidelines for the investigation and management of idiopathic thrombocytopenic purpura in adults, children and in pregnancy. Br J Haematol. 2003; 120:574–596.19. Jung TW, Kwon DH, Jeong DC, Koh DG. Analysis for spontaneous remission of chronic immune thrombocytopenic purpura in children. Clin Pediatr Hematol Oncol. 2011; 18:81–85.20. Peterson LC, Rao KV, Crosson JT, White JG. Fechtner syndrome--a variant of Alport's syndrome with leukocyte inclusions and macrothrombocytopenia. Blood. 1985; 65:397–406.
Article21. Robb LG, Tiedeman K. Idiopathic thrombocytopenic purpura: predictors of chronic disease. Arch Dis Child. 1990; 65:502–506.
Article22. Michel M, Khellaf M, Desforges L, Lee K, Schaeffer A, Godeau B, et al. Autoimmune thrombocytopenic Purpura and Helicobacter pylori infection. Arch Intern Med. 2002; 162:1033–1036.
Article23. Hashino S, Mori A, Suzuki S, Izumiyama K, Kahata K, Yonezumi M, et al. Platelet recovery in patients with idiopathic thrombocytopenic purpura after eradication of Helicobacter pylori. Int J Hematol. 2003; 77:188–191.
Article24. Emilia G, Longo G, Luppi M, Gandini G, Morselli M, Ferrara L, et al. Helicobacter pylori eradication can induce platelet recovery in idiopathic thrombocytopenic purpura. Blood. 2001; 97:812–814.
Article25. Jarque I, Andreu R, Llopis I, De la Rubia J, Gomis F, Senent L, et al. Absence of platelet response after eradication of Helicobacter pylori infection in patients with chronic idiopathic thrombocytopenic purpura. Br J Haematol. 2001; 115:1002–1003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Advances in management of pediatric chronic immune thrombocytopenia: a narrative review
- Diagnostic Approach of Childhood Immune Thrombocytopenia
- Natural course of childhood chronic immune thrombocytopenia using the revised terminology and definitions of the international working group: a single center experience
- Association of CD4+CD25+FoxP3+ regulatory T cells with natural course of childhood chronic immune thrombocytopenic purpura
- Clinical Courses and Outcome of Newly Diagnosed Immune Thrombocytopenia in Infants