Yonsei Med J.
2016 Jan;57(1):97-102. 10.3349/ymj.2016.57.1.97.
Burkholderia Sepsis in Children as a Hospital-Acquired Infection
- Affiliations
-
- 1Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. dskim6634@yuhs.ac
- 2Department of Laboratory Medicine and Research Institute of Bacterial Resistance, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2466357
- DOI: http://doi.org/10.3349/ymj.2016.57.1.97
Abstract
- PURPOSE
Hospital-acquired Burkholderia cepacia (B. cepacia) infection are not commonly recorded in patients without underlying lung disease, such as cystic fibrosis and chronic granulomatous disease. However, in 2014, B. cepacia appeared more frequently in pediatric blood samples than in any other year. In order to access this situation, we analyzed the clinical characteristics of B. cepacia infections in pediatric patients at our hospital.
MATERIALS AND METHODS
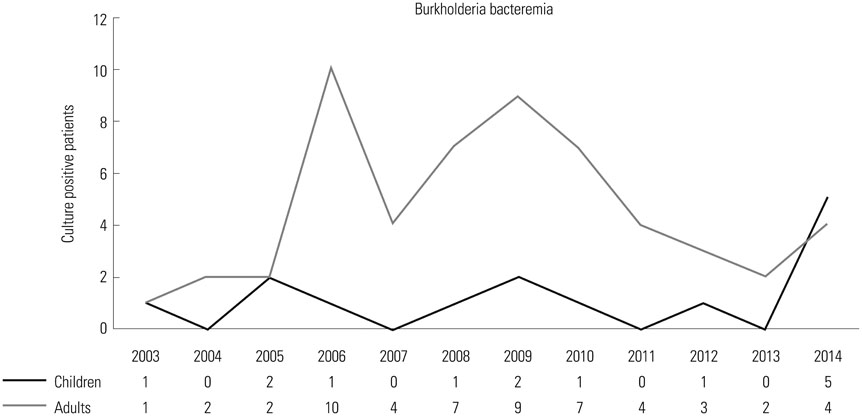
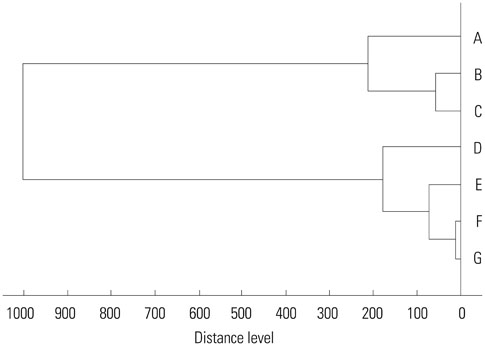
We conducted a retrospective study of blood isolates of B. cepacia taken at our hospital between January 2004 and December 2014. Patient clinical data were obtained by retrospective review of electronic medical records. We constructed a dendrogram for B. cepacia isolates from two children and five adult patients.
RESULTS
A total of 14 pediatric patients and 69 adult patients were identified as having B. cepacia bacteremia. In 2014, higher rates of B. cepacia bacteremia were observed in children. Most of them required Intensive Care Unit (ICU) care (12/14). In eleven children, sputum cultures were examined, and five of these children had the same strain of B. cepacia that grew out from their blood samples. Antibiotics were administered based on antibiotic sensitivity results. Four children expired despite treatment. Compared to children, there were no demonstrative differences in adults, except for history of ICU care.
CONCLUSION
Although there were not many pediatric cases at our hospital, awareness of colonization through hospital-acquired infection and effective therapy for infection of B. cepacia is needed, as it can cause mortality and morbidity.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Aged, 80 and over
Anti-Bacterial Agents/therapeutic use
Bacteremia/drug therapy/*epidemiology
Burkholderia Infections/blood/drug therapy/*epidemiology
Burkholderia cepacia/drug effects/*isolation & purification
Child
Child, Preschool
Cross Infection/blood/*diagnosis/drug therapy/mortality
Disease Outbreaks
Female
Humans
Incidence
Infant
*Intensive Care Units
Male
Microbial Sensitivity Tests
Middle Aged
Republic of Korea/epidemiology
Retrospective Studies
Treatment Outcome
Young Adult
Anti-Bacterial Agents
Figure
Reference
-
1. Mehrad B, Clark NM, Zhanel GG, Lynch JP 3rd. Antimicrobial resistance in hospital-acquired gram-negative bacterial infections. Chest. 2015; 147:1413–1421.
Article2. Kunz AN, Brook I. Emerging resistant Gram-negative aerobic bacilli in hospital-acquired infections. Chemotherapy. 2010; 56:492–500.
Article3. Solomon SL, Oliver KB. Antibiotic resistance threats in the United States: stepping back from the brink. Am Fam Physician. 2014; 89:938–941.4. Segonds C, Chabanon G. [Burkholderia cepacia: dangers of a phytopathogen organism for patients with cystic fibrosis]. Ann Biol Clin (Paris). 2001; 59:259–269.5. Brady MT, Marcon MJ. Pseudomonas and realated genera. In : Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, editors. Textbook of Pediatric Infectious Disease. 7th ed. Philadelphia: Sunders Elsevier;2014. p. 1582–1609.6. Govan JR, Hughes JE, Vandamme P. Burkholderia cepacia: medical, taxonomic and ecological issues. J Med Microbiol. 1996; 45:395–407.
Article7. Gautam V, Singhal L, Ray P. Burkholderia cepacia complex: beyond pseudomonas and acinetobacter. Indian J Med Microbiol. 2011; 29:4–12.
Article8. Griffin PM, Price GR, Schooneveldt JM, Schlebusch S, Tilse MH, Urbanski T, et al. Use of matrix-assisted laser desorption ionization-time of flight mass spectrometry to identify vancomycin-resistant enterococci and investigate the epidemiology of an outbreak. J Clin Microbiol. 2012; 50:2918–2931.
Article9. Spinali S, van Belkum A, Goering RV, Girard V, Welker M, Van Nuenen M, et al. Microbial typing by matrix-assisted laser desorption ionization-time of flight mass spectrometry: do we need guidance for data interpretation? J Clin Microbiol. 2015; 53:760–765.
Article10. Graindorge A, Menard A, Neto M, Bouvet C, Miollan R, Gaillard S, et al. Epidemiology and molecular characterization of a clone of Burkholderia cenocepacia responsible for nosocomial pulmonary tract infections in a French intensive care unit. Diagn Microbiol Infect Dis. 2010; 66:29–40.
Article11. Hua CN, Tokeshi J. Emergence of Burkholderia cepacia in Honolulu: a case of nursing home-acquired B. cepacia sepsis. Hawaii J Med Public Health. 2013; 72:308–309.12. Kaitwatcharachai C, Silpapojakul K, Jitsurong S, Kalnauwakul S. An outbreak of Burkholderia cepacia bacteremia in hemodialysis patients: an epidemiologic and molecular study. Am J Kidney Dis. 2000; 36:199–204.
Article13. Liao CH, Chang HT, Lai CC, Huang YT, Hsu MS, Liu CY, et al. Clinical characteristics and outcomes of patients with Burkholderia cepacia bacteremia in an intensive care unit. Diagn Microbiol Infect Dis. 2011; 70:260–266.
Article14. Lo Cascio G, Bonora MG, Zorzi A, Mortani E, Tessitore N, Loschiavo C, et al. A napkin-associated outbreak of Burkholderia cenocepacia bacteraemia in haemodialysis patients. J Hosp Infect. 2006; 64:56–62.
Article15. Avgeri SG, Matthaiou DK, Dimopoulos G, Grammatikos AP, Falagas ME. Therapeutic options for Burkholderia cepacia infections beyond co-trimoxazole: a systematic review of the clinical evidence. Int J Antimicrob Agents. 2009; 33:394–404.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Skin Infection with Burkholderia cepacia
- Two Case of Burkholderia cepacia Sepsis
- A Case of Ceftazidime-Nonsusceptible Burkholderia pseudomallei Infection
- A Case of Burkholderia cepacia Pneumonia after Lung Transplantation in a Recipient without Cystic Fibrosis
- Pseudoinfections Due to Benzalconium-chloride Solution Contaminated with Burkholderia cepacia