J Korean Ophthalmol Soc.
2019 Dec;60(12):1363-1368. 10.3341/jkos.2019.60.12.1363.
Optic Neuropathy after Taking Linezolid
- Affiliations
-
- 1Department of Ophthalmology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. coolleo@uuh.ulsan.kr
- KMID: 2466197
- DOI: http://doi.org/10.3341/jkos.2019.60.12.1363
Abstract
- PURPOSE
We report a case of optic neuropathy in a patient who was treated with pre-extensively drug-resistant tuberculosis(pre-XDR TB) treatment with linezolid.
CASE SUMMARY
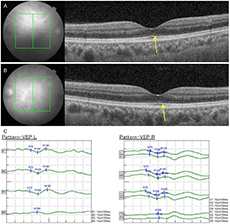
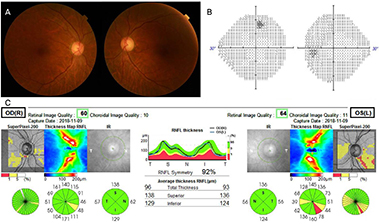
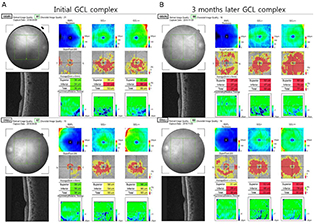
A 61-year-old male patient with no other underlying disease was diagnosed with pre-XDR Tb 6 months before and took the TB drug at another hospital. Ethambolol was not prescribed because it was resistant from the beginning of TB treatment. Threrefore, linezolid was included for treatment of pre-XDR TB. The patient's best corrected visual acuity was 20/400 in both eyes at the time of outpatient visit. In Ishihara color vision test, both eyes showed complete color blindness. There was no detectable relative afferent pupillary defect, and fundus examination showed hyperemic optic discs and visual field examination showed both central visual field defects. Linezolid induced optic neuropathy was suspected, the drug was discontinued. After one month, the patient's best corrected visual acuity recovered to 20/20 in both eyes, and visual field and color vision returned to normal at 3 months.
CONCLUSIONS
Linezolid is a broad spectrum antibiotic and is a useful drug for the treatment of broad-spectrum tuberculosis. However, since long-term use may cause optic neuropathy, the possibility of optic neuropathy should always be considered. If optic neuropathy is suspected, prompt drug withdrawal is required and reversible clinical changes can be expected.
MeSH Terms
Figure
Reference
-
1. Thompson MJ, Albert DM. Ocular tuberculosis. Arch Ophthalmol. 2005; 123:844–849.2. Yoon YS, Lee SH, Min JK, Lee CK. A case of spontaneous recovery of an iris cyst in a patient with peritoneal tuberculosis. J Korean Ophthalmol Soc. 2018; 59:491–495.3. Mok JH. Updates of tuberculosis diagnosis and treatment. J Korean Soc Health Syst Pharm. 2016; 33:101–110.4. Pilania RK, Arora A, Agarwal A, et al. Linezolid-induced mitochondrial toxicity presenting as retinal nerve fiber layer microcysts and optic and peripheral neuropathy in a patient with chronic granulomatous disease. Retin Cases Brief Rep. 2018; 07. DOI: 10.1097/ICB.0000000000000777. PMID30048406.5. Lee M, Lee J, Carroll MW, et al. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N Engl J Med. 2012; 367:1508–1518.6. Yoon SW, Choi JC. Treatment of pulmonary tuberculosis. J Korean Med Assoc. 2019; 62:25–36.7. Kang YA. Diagnosis and treatment of multidrug-resistant tuberculosis. J Korean Med Assoc. 2014; 57:27–33.8. Garrabou G, Soriano À, Pinós T, et al. Influence of mitochondrial genetics on the mitochondrial toxicity of linezolid in blood cells and skin nerve fibers. Antimicrob Agents Chemother. 2017; 61:e00542–e00517.9. De Vriese AS, Coster RV, Smet J, et al. Linezolid-induced inhibition of mitochondrial protein synthesis. Clin Infect Dis. 2006; 42:1111–1117.10. Park SJ, Jung JU, Kang YK, et al. Toxic optic neuropathy caused by chlorfenapyr poisoning. J Korean Ophthalmol Soc. 2018; 59:1097–1102.11. Wang L, Dong J, Cull G, et al. Varicosities of intraretinal ganglion cell axons in human and nonhuman primates. Invest Ophthalmol Vis Sci. 2003; 44:2–9.12. Perry CM, Jarvis B. Linezolid: a review of its use in the management of serious gram-positive infections. Drugs. 2001; 61:525–551.13. Ishii N, Kinouchi R, Inoue M, Yoshida A. Linezolid-induced optic neuropathy with a rare pathological change in the inner retina. Int Ophthalmol. 2016; 36:761–766.14. Rho JP, Sia IG, Crum BA, et al. Linezolid-associated peripheral neuropathy. Mayo Clin Proc. 2004; 79:927–930.15. Park DH, Park TK, Ohn YH, et al. Linezolid induced retinopathy. Doc Ophthalmol. 2015; 131:237–244.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Etiology of Optic Neuropathy
- A Case of Lactic Acidosis Caused by Linezolid Treatment of Persistent Methicillin-Resistant Staphylococcus Aureus Bacteremia
- Correlation between Visual Acuity and Retinal Nerve Fiber Layer Thickness in Optic Neuropathies
- Indirect Traumatic Optic Neuropathy with Gadolinium Enhancement
- Comparison of Optic Disc Appearance in Anterior ischemic optic neuropathy and Optic neuritis