Korean J Leg Med.
2019 Nov;43(4):153-158. 10.7580/kjlm.2019.43.4.153.
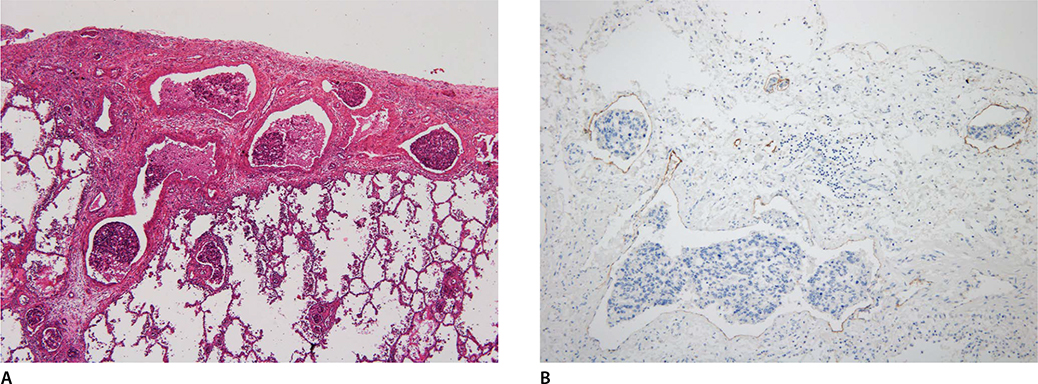
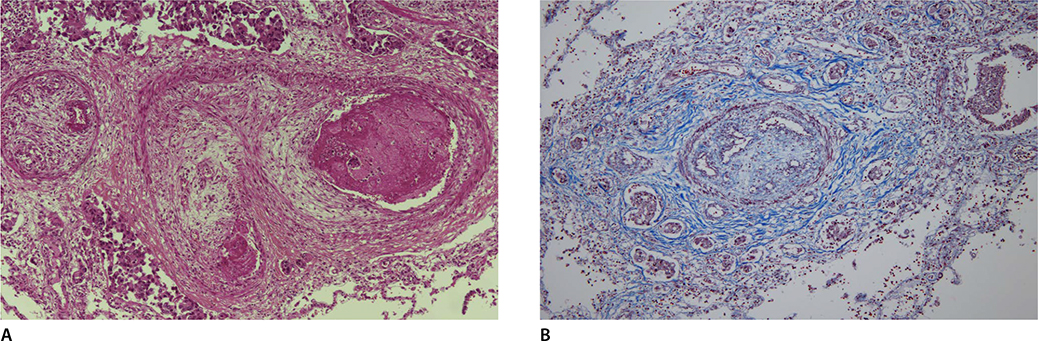
Sudden Unexpected Death During Bronchoscopy of a Patient with Pulmonary Lymphangitic Carcinomatosis and Pulmonary Tumor Thrombotic Microangiopathy due to Gastric Cancer
- Affiliations
-
- 1Medical Examiner's Office, National Forensic Service, Wonju, Korea. zzeva@korea.kr
- 2Department of Pathology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 3Division of Forensic Investigation, National Forensic Service Seoul Institute, Seoul, Korea.
- KMID: 2464493
- DOI: http://doi.org/10.7580/kjlm.2019.43.4.153
Abstract
- We present the case of a 48-year-old woman who complained of sustained dyspnea and newly developed dyspnea, who then suddenly and unexpectedly expired during bronchoscopy. On postmortem examination, the deceased had advanced gastric cancer as a primary tumor. Frequent lymphatic tumor emboli were observed with some pulmonary lymphangitic carcinomatosis (PLC), and pulmonary tumor thrombotic microangiopathy (PTMA). PLC and PTMA are lethal forms of pulmonary metastasis, and PTMA can lead to sudden death. The characteristic findings of PLC and PTMA in the deceased were not predominant, however, and the clinical manifestation was not acutely deteriorating. These findings are, therefore, insufficient to explain the deceased's sudden death. Clinically, the deceased manifested hypoxemia, bradycardia and cardiac arrest during bronchoscopy and then soon expired, suggesting the possibility of cardiovascular complication related to bronchoscopy. Despite several limitations, we assumed that the sudden unexpected death might have been induced by cardiovascular complications related to bronchoscopy and due to the underlying pathologic condition by PLC and PTMA.
Keyword
MeSH Terms
Figure
Reference
-
1. Dennstedt FE, Greenberg SD, Kim HS, et al. Pulmonary lymphangitic carcinomatosis from occult stomach carcinoma in young adults: an unusual cause of dyspnea. Chest. 1983; 84:787–788.2. Uruga H, Fujii T, Kurosaki A, et al. Pulmonary tumor thrombotic microangiopathy: a clinical analysis of 30 autopsy cases. Intern Med. 2013; 52:1317–1323.3. Stahl DL, Richard KM, Papadimos TJ. Complications of bronchoscopy: a concise synopsis. Int J Crit Illn Inj Sci. 2015; 5:189–195.4. Kruckel A, Moreira A, Frohlich W, et al. Eosinophil-cationic protein: a novel liquid prognostic biomarker in melanoma. BMC Cancer. 2019; 19:207.5. Chinen K, Kurosumi M, Ohkura Y, et al. Sudden unexpected death in patients with malignancy: a clinicopathologic study of 28 autopsy cases. Pathol Res Pract. 2006; 202:869–875.6. Bruce DM, Heys SD, Eremin O. Lymphangitis carcinomatosa: a literature review. J R Coll Surg Edinb. 1996; 41:7–13.7. Moubax K, Wuyts W, Vandecaveye V, et al. Pulmonary lymphangitic carcinomatosis as a primary manifestation of gastric carcinoma in a young adult: a case report and review of the literature. BMC Res Notes. 2012; 5:638.8. Bhattacharya PK, Jamil M, Khonglah Y, et al. A rare case of pulmonary lymphangitic carcinomatosis in a young adult with carcinoma stomach. J Clin Diagn Res. 2017; 11:OD07–OD09.9. Belhassine M, Papakrivopoulou E, Venet C, et al. Gastric adenocarcinoma revealed by atypical pulmonary lymphangitic carcinomatosis. J Gastrointest Oncol. 2018; 9:1207–1212.10. Okubo Y, Wakayama M, Kitahara K, et al. Pulmonary tumor thrombotic microangiopathy induced by gastric carcinoma: morphometric and immunohistochemical analysis of six autopsy cases. Diagn Pathol. 2011; 6:27.11. Chinen K, Tokuda Y, Fujiwara M, et al. Pulmonary tumor thrombotic microangiopathy in patients with gastric carcinoma: an analysis of 6 autopsy cases and review of the literature. Pathol Res Pract. 2010; 206:682–689.12. Khan MA, Whitcomb ME. Editorial: Deaths associated with flexible bronchoscopy. Chest. 1976; 70:200–201.13. Hassan G, Qureshi W, Khan GQ, et al. Cardiovascular consequences of fiberoptic bronchoscopy. JK Sci. 2005; 7:1–2.14. Gilchrist FJ, Alton H, Brundler MA, et al. Pulmonary lymphangitic carcinomatosis presenting as severe interstitial lung disease in a 15-year-old female. Eur Respir Rev. 2011; 20:208–210.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Tumor Thrombotic Microangiopathy Associated with Advanced Gastric Cancer Successfully Treated with Chemotherapy
- A Case of Locally Advanced Breast Cancer Complicated by Pulmonary Tumor Thrombotic Microangiopathy
- Fatal progressive right heart failure in a pancreatic cancer patient
- Occult Gastric Cancer Presenting as Hypoxia from Pulmonary Tumor Thrombotic Microangiopathy
- A Case of Pulmonary Tumor Thrombotic Microangiopathy in a Patient with Advanced Gastric Cancer