Korean J Orthod.
2019 Nov;49(6):372-380. 10.4041/kjod.2019.49.6.372.
The influence of leukocyte-platelet-rich plasma on accelerated orthodontic tooth movement in rabbits
- Affiliations
-
- 1Private practice, Nakhon Ratchasima, Thailand.
- 2Orthodontic Section, Department of Preventive Dentistry, Faculty of Dentistry, Prince of Songkla University, Hat Yai, Songkhla, Thailand. samruaj@hotmail.com
- KMID: 2464200
- DOI: http://doi.org/10.4041/kjod.2019.49.6.372
Abstract
OBJECTIVE
To determine the effects of a local injection of leukocyte-platelet-rich plasma (L-PRP) on orthodontic tooth movement in rabbits.
METHODS
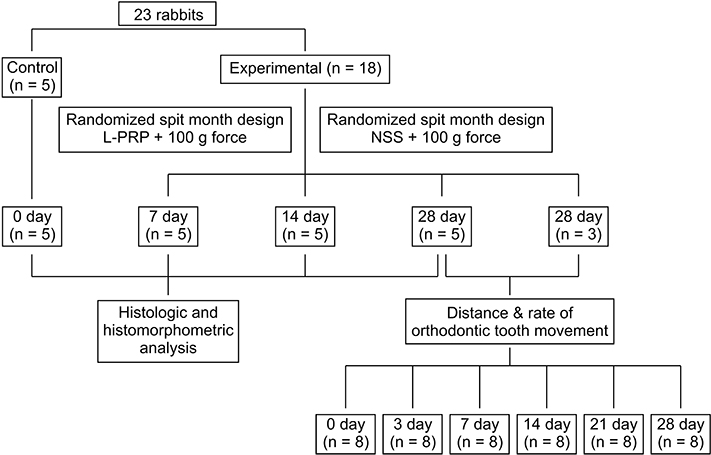
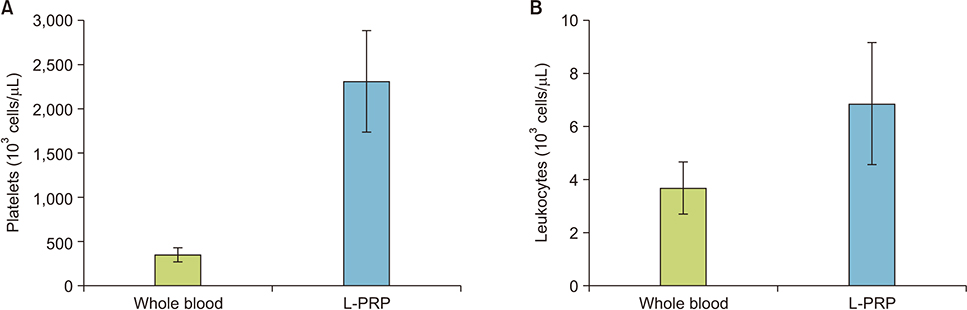
Twenty-three male New Zealand white rabbits were included in a split-mouth design. Tooth movement with a 100-g nickel-titanium closed-coil spring was performed on the maxillary first premolars. L-PRP was injected submucosally at the buccal and lingual areas of the first premolar in one random side of the maxilla and the other side served as the control and received normal saline. The amount of tooth movement was assessed on three-dimensional digital models on days 0, 3, 7, 14, 21, and 28. Histological findings and osteoclast numbers were examined on day 0 as the baseline and on days 7, 14, and 28.
RESULTS
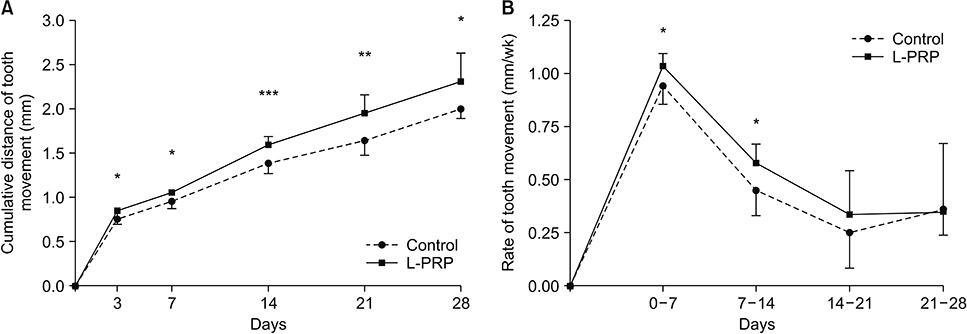
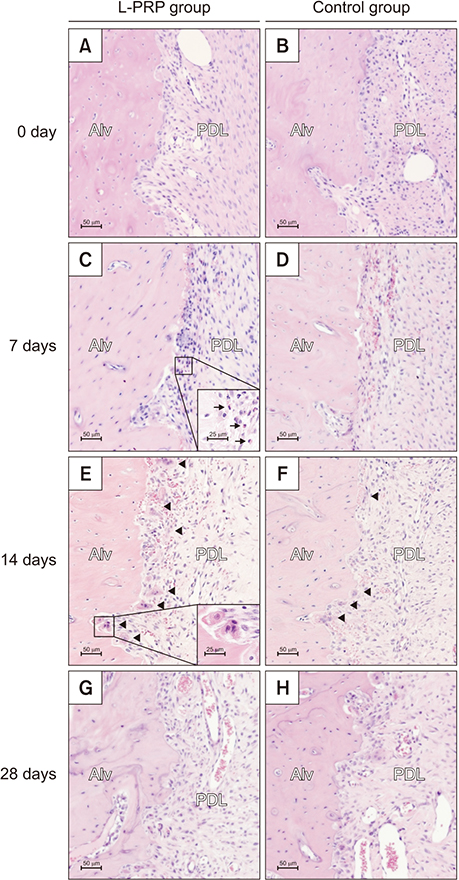
The L-PRP group showed significantly greater cumulative tooth movement at all observed periods. However, a significantly higher rate of tooth movement was observed only on days 0-7 and 7-14. The osteoclast numbers were significantly increased in the L-PRP group on days 7 and 14.
CONCLUSIONS
Local injection of L-PRP resulted in a transient increase in the rate of tooth movement and higher osteoclast numbers.
Figure
Reference
-
1. Teixeira CC, Khoo E, Tran J, Chartres I, Liu Y, Thant LM, et al. Cytokine expression and accelerated tooth movement. J Dent Res. 2010; 89:1135–1141.
Article2. Andrade I Jr, Taddei SRA, Souza PEA. Inflammation and tooth movement: the role of cytokines, chemokines, and growth factors. Semin Orthod. 2012; 18:257–269.
Article3. Sánchez AR, Sheridan PJ, Kupp LI. Is platelet-rich plasma the perfect enhancement factor? A current review. Int J Oral Maxillofac Implants. 2003; 18:93–103.4. Fernandez-Moure JS, Van Eps JL, Cabrera FJ, Barbosa Z, Medrano Del Rosal G, Weiner BK, et al. Platelet-rich plasma: a biomimetic approach to enhancement of surgical wound healing. J Surg Res. 2017; 207:33–44.
Article5. Oryan A, Alidadi S, Moshiri A. Platelet-rich plasma for bone healing and regeneration. Expert Opin Biol Ther. 2016; 16:213–232.
Article6. Rodriguez IA, Growney Kalaf EA, Bowlin GL, Sell SA. Platelet-rich plasma in bone regeneration: engineering the delivery for improved clinical efficacy. Biomed Res Int. 2014; 2014:392398.
Article7. Sundman EA, Cole BJ, Fortier LA. Growth factor and catabolic cytokine concentrations are influenced by the cellular composition of platelet-rich plasma. Am J Sports Med. 2011; 39:2135–2140.
Article8. Yuan T, Guo SC, Han P, Zhang CQ, Zeng BF. Applications of leukocyte- and platelet-rich plasma (L-PRP) in trauma surgery. Curr Pharm Biotechnol. 2012; 13:1173–1184.
Article9. Schär MO, Diaz-Romero J, Kohl S, Zumstein MA, Nesic D. Platelet-rich concentrates differentially release growth factors and induce cell migration in vitro. Clin Orthop Relat Res. 2015; 473:1635–1643.
Article10. Anitua E, Zalduendo M, Troya M, Padilla S, Orive G. Leukocyte inclusion within a platelet rich plasmaderived fibrin scaffold stimulates a more pro-inflammatory environment and alters fibrin properties. PLoS One. 2015; 10:e0121713.
Article11. Pifer MA, Maerz T, Baker KC, Anderson K. Matrix metalloproteinase content and activity in low-platelet, low-leukocyte and high-platelet, high-leukocyte platelet rich plasma (PRP) and the biologic response to PRP by human ligament fibroblasts. Am J Sports Med. 2014; 42:1211–1218.
Article12. Yin W, Qi X, Zhang Y, Sheng J, Xu Z, Tao S, et al. Advantages of pure platelet-rich plasma compared with leukocyte- and platelet-rich plasma in promoting repair of bone defects. J Transl Med. 2016; 14:73.
Article13. Liou EJW. The development of submucosal injection of platelet rich plasma for accelerating orthodontic tooth movement and preserving pressure side alveolar bone. APOS Trends Orthod. 2016; 6:5–11.
Article14. Güleç A, Bakkalbaşı BÇ, Cumbul A, Uslu Ü, Alev B, Yarat A. Effects of local platelet-rich plasma injection on the rate of orthodontic tooth movement in a rat model: a histomorphometric study. Am J Orthod Dentofacial Orthop. 2017; 151:92–104.
Article15. Chen YW, Wang HC, Gao LH, Liu C, Jiang YX, Qu H, et al. Osteoclastogenesis in local alveolar bone in early decortication-facilitated orthodontic tooth movement. PLoS One. 2016; 11:e0153937.
Article16. Jia WT, Zhang CQ, Wang JQ, Feng Y, Ai ZS. The prophylactic effects of platelet-leucocyte gel in osteomyelitis: an experimental study in a rabbit model. J Bone Joint Surg Br. 2010; 92:304–310.17. Rashid A, ElSharaby FA, Nassef EM, Mehanni S, Mostafa YA. Effect of platelet-rich plasma on orthodontic tooth movement in dogs. Orthod Craniofac Res. 2017; 20:102–110.
Article18. Alhashimi N, Frithiof L, Brudvik P, Bakhiet M. Orthodontic tooth movement and de novo synthesis of proinflammatory cytokines. Am J Orthod Dentofacial Orthop. 2001; 119:307–312.
Article19. Ibrahim AY, Gudhimella S, Pandruvada SN, Huja SS. Resolving differences between animal models for expedited orthodontic tooth movement. Orthod Craniofac Res. 2017; 20 Suppl 1:72–76.
Article20. Kaplanski G, Marin V, Montero-Julian F, Mantovani A, Farnarier C. IL-6: a regulator of the transition from neutrophil to monocyte recruitment during inflammation. Trends Immunol. 2003; 24:25–29.
Article21. Dai J, Rabie AB. VEGF: an essential mediator of both angiogenesis and endochondral ossification. J Dent Res. 2007; 86:937–950.
Article22. Mammoto T, Jiang A, Jiang E, Mammoto A. Platelet rich plasma extract promotes angiogenesis through the angiopoietin1-Tie2 pathway. Microvasc Res. 2013; 89:15–24.
Article23. Lyras DN, Kazakos K, Verettas D, Polychronidis A, Tryfonidis M, Botaitis S, et al. The influence of platelet-rich plasma on angiogenesis during the early phase of tendon healing. Foot Ankle Int. 2009; 30:1101–1106.
Article24. Cheung WY, Liu C, Tonelli-Zasarsky RM, Simmons CA, You L. Osteocyte apoptosis is mechanically regulated and induces angiogenesis in vitro. J Orthop Res. 2011; 29:523–530.
Article25. Nakagawa M, Kaneda T, Arakawa T, Morita S, Sato T, Yomada T, et al. Vascular endothelial growth factor (VEGF) directly enhances osteoclastic bone resorption and survival of mature osteoclasts. FEBS Lett. 2000; 473:161–164.
Article26. Kohno S, Kaku M, Tsutsui K, Motokawa M, Ohtani J, Tenjo K, et al. Expression of vascular endothelial growth factor and the effects on bone remodeling during experimental tooth movement. J Dent Res. 2003; 82:177–182.
Article27. Rody WJ Jr, King GJ, Gu G. Osteoclast recruitment to sites of compression in orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2001; 120:477–489.
Article28. Akbulut S, Yagci A, Yay AH, Yalcin B. Experimental investigation of effects of platelet-rich plasma on early phases of orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2019; 155:71–79.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Do platelet concentrates accelerate orthodontic tooth movement?: a systematic review
- Accelerated orthodontic tooth movement: surgical techniques and the regional acceleratory phenomenon
- Effect of Platelet-rich Plasma on Burn Wounds according to Time of Application: An Experimental Study on Rats
- Leukocyte platelet-rich fibrin in endodontic microsurgery: a report of 2 cases
- The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report