J Korean Neurosurg Soc.
2019 Jul;62(4):414-421. 10.3340/jkns.2018.0091.
Evaluation of Dimensions of Kambin’s Triangle to Calculate Maximum Permissible Cannula Diameter for Percutaneous Endoscopic Lumbar Discectomy: A 3-Dimensional Magnetic Resonance Imaging Based Study
- Affiliations
-
- 1Department of Spine, Deenanath Mangeshkar Hospital, Pune, India. drpai2002@gmail.com
- KMID: 2463672
- DOI: http://doi.org/10.3340/jkns.2018.0091
Abstract
OBJECTIVE
To evaluate 3-dimensional magnetic resonance imaging (MRI) of Kambin's safe zone to calculate maximum cannula diameter permissible for safe percutaneous endoscopic lumbar discectomy.
METHODS
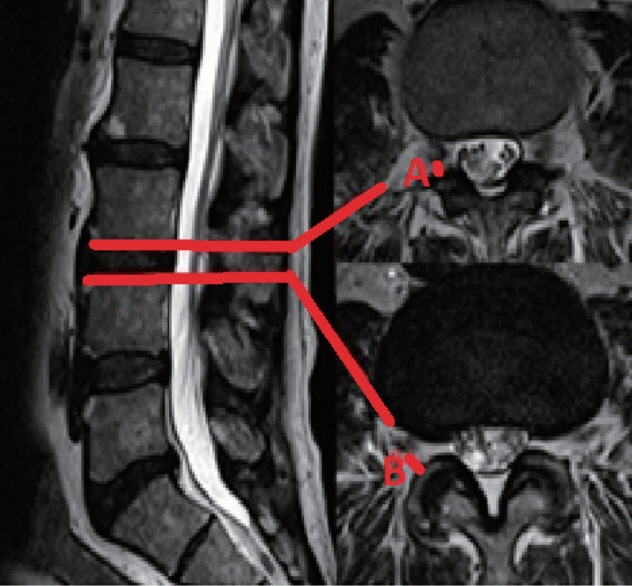
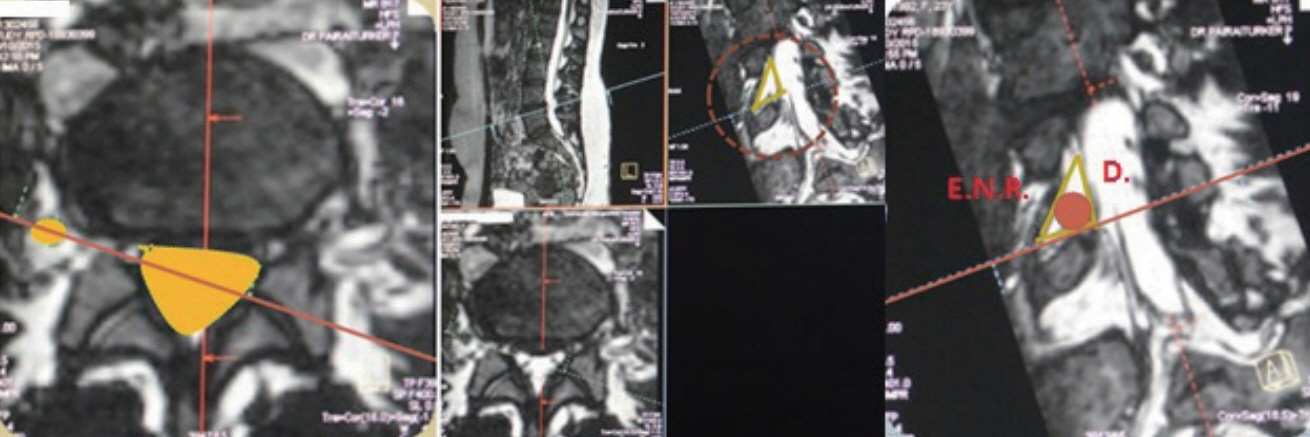
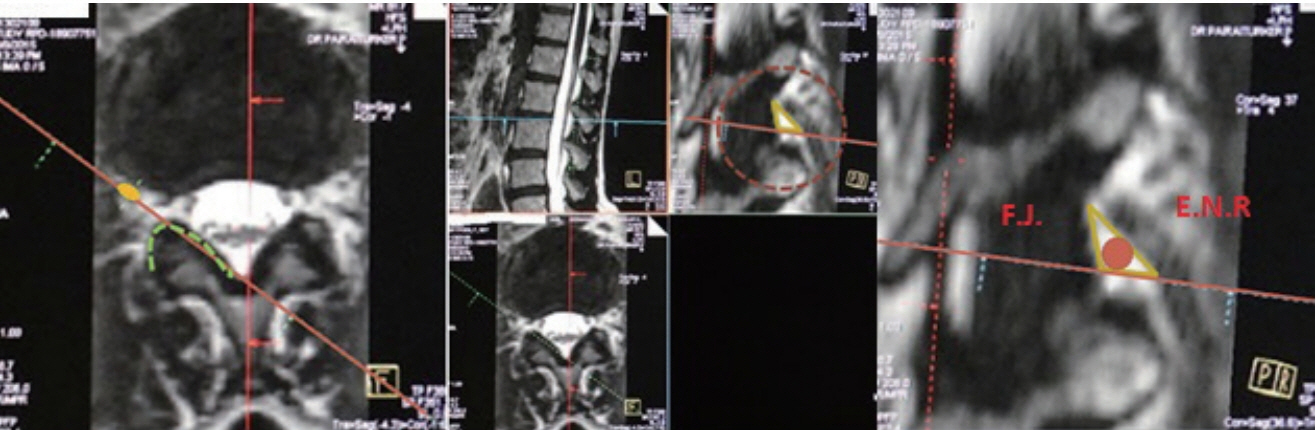
Fifty 3D MRIs of 19 males and 31 females (mean, 47 years) were analysed. Oblique, axial and sagittal views were used for image analysis. Three authors calculated the inscribed circle (cannula diameter) individually, within the neural (original) and bony Kambin's triangle in oblique views, disc heights on sagittal views and root to facet distances at upper and lower end plate levels on axial views and their averages were taken.
RESULTS
The mean root to facet distances at upper end plate level measured on axial sections increased from 3.42±3.01 mm at L12 level to 4.57±2.49 mm at L5S1 level. The mean root to facet distances at lower end plate level measured on axial sections also increased from 6.07±1.13 mm at L12 level to 12.9±2.83 mm at L5S1 level. Mean maximum cannula diameter permissible through the neural Kambin's triangle increased from 5.67±1.38 mm at L12 level to 9.7±3.82 mm at L5S1 level. The mean maximum cannula diameter permissible through the bony Kambin's triangle also increased from 4.03±1.08 mm at L12 level to 6.11±1 mm at L5S1 level. Only 2% of the 427 bony Kambin's triangles could accommodate a cannula diameter of 8mm. The base of the bony Kambin's triangle taken in oblique view (3D MRI) was significantly higher than the root to facet distance at lower end plate level taken in axial view.
CONCLUSION
The largest mean diameter of endoscopic cannula passable through "bony" Kambin's triangle was distinctively smaller than the largest mean diameter of endoscopic cannula passable through "neural" Kambin's triangle at all levels. Although proximity of exiting root to the facet joint is always taken into consideration before PELD procedure, our 3D MRI based anatomical study is the first to provide actual maximum cannula dimensions permissible in this region.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Ahn Y, Lee SH, Lee JH, Kim JU, Liu WC. Transforaminal percutaneous endoscopic lumbar discectomy for upper lumbar disc herniation: clinical outcome, prognostic factors, and technical consideration. Acta Neurochir (Wien). 151:199–206. 2009.
Article2. Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976). 29:E326–E332. 2004.
Article3. Arslan M, Cömert A, Açar HI, Ozdemir M, Elhan A, Tekdemir I, et al. Nerve root to lumbar disc relationships at the intervertebral foramen from a surgical viewpoint: an anatomical study. Clin Anat. 25:218–223. 2012.
Article4. Choi G, Lee SH, Bhanot A, Raiturker PP, Chae YS. Percutaneous endoscopic discectomy for extraforaminal lumbar disc herniations: extraforaminal targeted fragmentectomy technique using working channel endoscope. Spine (Phila Pa 1976). 32:E93–E99. 2007.5. Choi G, Lee SH, Lokhande P, Kong BJ, Shim CS, Jung B, et al. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine (Phila Pa 1976). 33:E508–E515. 2008.
Article6. Choi I, Ahn JO, So WS, Lee SJ, Choi IJ, Kim H. Exiting root injury in transforaminal endoscopic discectomy: preoperative image considerations for safety. Eur Spine J. 22:2481–2487. 2013.
Article7. Civelek E, Solmaz I, Cansever T, Onal B, Kabatas S, Bolukbasi N, et al. Radiological analysis of the triangular working zone during transforaminal endoscopic lumbar discectomy. Asian Spine J. 6:98–104. 2012.
Article8. Güvençer M, Naderi S, Kiray A, Yilmaz HS, Tetik S. The relation between the lumbar vertebrae and the spinal nerves for far lateral lumbar spinal approaches. J Clin Neurosci. 15:192–197. 2008.
Article9. Hoshide R, Feldman E, Taylor W. Cadaveric analysis of the Kambin’s triangle. Cureus. 8:e475. 2016.
Article10. Hurday Y, Xu B, Guo L, Cao Y, Wan Y, Jiang H, et al. Radiographic measurement for transforaminal percutaneous endoscopic approach (PELD). Eur Spine J. 26:635–645. 2017.
Article11. Kambin P, Gellman H. Percutaneous lateral discectomy of the lumbar spine a preliminary report. Clin Orthop Relat Res. 174:127–132. 1983.12. Kendir S, Acar HI, Comert A, Ozdemir M, Kahilogullari G, Elhan A, et al. Window anatomy for neurosurgical approaches. Laboratory investigation. J Neurosurg. 111:365–370. 2009.13. Lee SH, Kang BU, Ahn Y, Choi G, Choi YG, Ahn KU, et al. Operative failure of percutaneous endoscopic lumbar discectomy: a radiologic analysis of 55 cases. Spine (Phila Pa 1976). 31:E285–E290. 2006.14. Lertudomphonwanit T, Keorochana G, Kraiwattanapong C, Chanplakorn P, Leelapattana P, Wajanavisit W. Anatomic considerations of intervertebral disc perspective in lumbar posterolateral approach via Kambin’s triangle: cadaveric study. Asian Spine J. 10:821–827. 2016.
Article15. Loukas M, Louis RG Jr, Childs RS. Anatomical examination of the recurrent artery of Heubner. Clin Anat. 19:25–31. 2006.
Article16. Min JH, Kang SH, Lee JB, Cho TH, Suh JK, Rhyu IJ. Morphometric analysis of the working zone for endoscopic lumbar discectomy. J Spinal Disord Tech. 18:132–135. 2005.
Article17. Mirkovic SR, Schwartz DG, Glazier KD. Anatomic considerations in lumbar posterolateral percutaneous procedures. Spine (Phila Pa 1976). 20:1965–1971. 1995.
Article18. Quester R, Schröder R. The shrinkage of the human brain stem during formalin fixation and embedding in paraffin. J Neurosci Methods. 75:81–89. 1997.
Article19. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976). 33:931–939. 2008.
Article20. Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976). 27:722–731. 2002.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Endoscopic Discectomy Compared to Microsurgical Discectomy: Preliminary Results
- Clinical Outcomes of Percutaneous Endoscopic Laser Lumbar Discectomy
- Cadaveric anatomy of the lumbar triangular safe zone of Kambin’s in North West Indian population
- Evolution of Percutaneous Endoscopic Lumbar Decompression
- Anatomical assessment of the Kambin’s triangle for percutaneous posterolateral transforaminal endoscopic surgery of lumbar intervertebral discs: a magnetic resonance imaging based study