Obstet Gynecol Sci.
2019 Nov;62(6):429-437. 10.5468/ogs.2019.62.6.429.
ICSI using fresh and frozen PESA-TESA spermatozoa to examine assisted reproductive outcome retrospectively
- Affiliations
-
- 1Department of Biotechnology, REVA University, Bangalore, India. drkrmanjula@gmail.com
- 2Post Graduate-Department of Biotechnology, Dayananda Sagar Institutions, Bangalore, India.
- KMID: 2462121
- DOI: http://doi.org/10.5468/ogs.2019.62.6.429
Abstract
OBJECTIVE
The male reproductive system generates, accumulates, and transports the sperm. In this study, 2 methods of surgically retrieving sperm, namely, testicular sperm aspiration (TESA) and percutaneous epididymal sperm aspiration (PESA), are discussed and studied in men aged ≤38 years to achieve successful conception using assisted reproductive technology. The purpose was to assess the fertilization rate (FA), clinical pregnancy, and live birth rate (LBR) with sperm.
METHODS
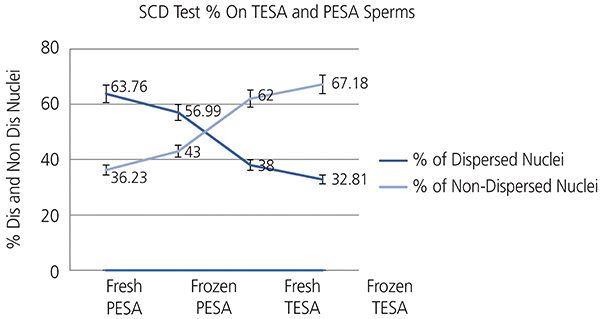
A total of 287 semen samples were divided into 4 groups as follows: fresh PESA (n=73), frozen PESA (n=65), fresh TESA (n=128), and frozen TESA (n=21). The DNA fragmentation test using sperm chromatin dispersion assay was measured and reported.
RESULTS
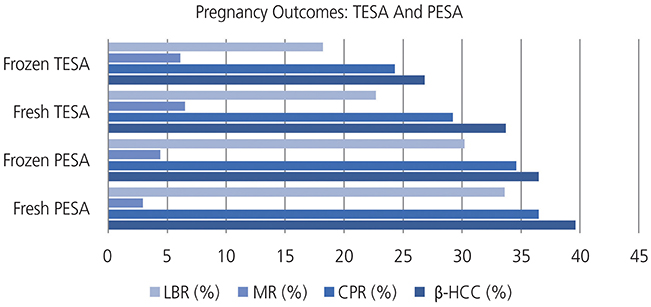
FA was 70.3% and 65.5%, (P<0.022) for fresh and frozen epididymal sperm and 53.8% and 49.5%, (P<0.032) for fresh and frozen testicular sperm. LBR was 33.6% and 30.2% (P<0.075) for fresh and frozen epididymal sperm (PESA) and 22.7% and 18.2% (P<0.063) for fresh and frozen-thawed TESA sperm.
CONCLUSION
Exposure to tissue shearing may adversely affect sperm quality. Increased sperm DNA damage due to long-term exposure while teasing enhances reactive oxygen species production foremost to membrane damage because of the oxidation of polyunsaturated fatty acid in lipids (lipid peroxidation), oxidation of amino acid in proteins, and inactivation of specific enzymes, all leading to enzymatic dipping and possibility of less fertilization and conception as indicated by the increase in LBR with fresh/frozen PESA compared to with fresh/frozen TESA.
Keyword
MeSH Terms
Figure
Reference
-
1. Temple-Smith PD, Southwick GJ, Yates CA, Trounson AO, de Kretser DM. Human pregnancy by in vitro fertilization (IVF) using sperm aspirated from the epididymis. J In Vitro Fert Embryo Transf. 1985; 2:119–122.2. Corea M, Campagnone J, Sigman M. The diagnosis of azoospermia depends on the force of centrifugation. Fertil Steril. 2005; 83:920–922.
Article3. Esteves SC, Lee W, Benjamin DJ, Seol B, Verza S Jr, Agarwal A. Reproductive potential of men with obstructive azoospermia undergoing percutaneous sperm retrieval and intracytoplasmic sperm injection according to the cause of obstruction. J Urol. 2013; 189:232–237.
Article4. Glina S, Fragoso JB, Martins FG, Soares JB, Galuppo AG, Wonchockier R. Percutaneous epididymal sperm aspiration (PESA) in men with obstructive azoospermia. Int Braz J Urol. 2003; 29:141–145.
Article5. Hao L, Li ZG, He HG, Zhang ZG, Zhang JJ, Dong Y, et al. Application of percutaneous epididymal sperm aspiration in azoospermia. Eur Rev Med Pharmacol Sci. 2017; 21:1032–1035.6. Kovac JR, Lehmann KJ, Fischer MA. A single-center study examining the outcomes of percutaneous epididymal sperm aspiration in the treatment of obstructive azoospermia. Urol Ann. 2014; 6:41–45.
Article7. Gardner DK, Lane M, Watson AJ. A laboratory guide to the mammalian embryo. New York (NY): Oxford University Press;2004.8. Gardner DK, Rizk BR, Falcone T. Human assisted reproductive technology: future trends in laboratory and clinical practice. Cambridge: Cambridge University Press;2011.9. Nagy Z, Liu J, Cecile J, Silber S, Devroey P, Van Steirteghem A. Using ejaculated, fresh, and frozen-thawed epididymal and testicular spermatozoa gives rise to comparable results after intracytoplasmic sperm injection. Fertil Steril. 1995; 63:808–815.10. Zhu J, Tsirigotis M, Pelekanos M, Craft I. In-vitro maturation of human testicular spermatozoa. Hum Reprod. 1996; 11:231–232.11. Smith RP, Coward RM, Lipshultz LI. The office visit. Urol Clin North Am. 2014; 41:19–37.
Article12. McBride JA, Coward RM. Recovery of spermatogenesis following testosterone replacement therapy or anabolic-androgenic steroid use. Asian J Androl. 2016; 18:373–380.
Article13. Coward RM, Mata DA, Smith RP, Kovac JR, Lipshultz LI. Vasectomy reversal outcomes in men previously on testosterone supplementation therapy. Urology. 2014; 84:1335–1341.
Article14. Boorjian S, Lipkin M, Goldstein M. The impact of obstructive interval and sperm granuloma on outcome of vasectomy reversal. J Urol. 2004; 171:304–306.
Article15. International Committee of Medical Journal Editors (ICMJE). Recommendations for the conduct, reporting, editing, and publication of scholarly work in medical journals (December 16, 2014). [place unknown]: ICMJE;2014.16. Coward RM, Mills JN. A step-by-step guide to office-based sperm retrieval for obstructive azoospermia. Transl Androl Urol. 2017; 6:730–744.
Article17. Gorgy A, Meniru GI, Naumann N, Beski S, Bates S, Craft IL. The efficacy of local anaesthesia for percutaneous epididymal sperm aspiration and testicular sperm aspiration. Hum Reprod. 1998; 13:646–650.
Article18. Donoso P, Tournaye H, Devroey P. Which is the best sperm retrieval technique for non-obstructive azoospermia? A systematic review. Hum Reprod Update. 2007; 13:539–549.
Article19. Van Peperstraten A, Proctor ML, Johnson NP, Philipson G. Techniques for surgical retrieval of sperm prior to intra-cytoplasmic sperm injection (ICSI) for azoospermia. Cochrane Database Syst Rev. 2008; 2:CD002807.20. Bernie AM, Mata DA, Ramasamy R, Schlegel PN. Comparison of microdissection testicular sperm extraction, conventional testicular sperm extraction, and testicular sperm aspiration for nonobstructive azoospermia: a systematic review and meta-analysis. Fertil Steril. 2015; 104:1099–1103.
Article21. Semião-Francisco L, Braga DP, Figueira Rde C, Madaschi C, Pasqualotto FF, Iaconelli A Jr, et al. Assisted reproductive technology outcomes in azoospermic men: 10 years of experience with surgical sperm retrieval. Aging Male. 2010; 13:44–50.22. Lewin A, Weiss DB, Friedler S, Ben-Shachar I, Porat-Katz A, Meirow D, et al. Delivery following intracytoplasmic injection of mature sperm cells recovered by testicular fine needle aspiration in a case of hypergonadotropic azoospermia due to maturation arrest. Hum Reprod. 1996; 11:769–771.
Article23. Gorgy A, Podsiadly BT, Bates S, Craft IL. Testicular sperm aspiration (TESA): the appropriate technique. Hum Reprod. 1998; 13:1111–1113.
Article24. Jensen CF, Ohl DA, Hiner MR, Fode M, Shah T, Smith GD, et al. Multiple needle-pass percutaneous testicular sperm aspiration as first-line treatment in azoospermic men. Andrology. 2016; 4:257–262.
Article25. Qiu Y, Wang S, Yang D, Fan Y, Su Q, Wang Z, et al. Percutaneous vasal sperm aspiration and intrauterine insemination in the treatment of obstructive azoospermia. Fertil Steril. 1997; 68:1135–1138.
Article26. Qiu Y, Wang SM, Yang DT, Wang LG. Percutaneous vasal sperm aspiration and intrauterine insemination for infertile males with anejaculation. Fertil Steril. 2003; 79:618–620.
Article27. Fernández JL, Muriel L, Goyanes V, Segrelles E, Gosálvez J, Enciso M, et al. Simple determination of human sperm DNA fragmentation with an improved sperm chromatin dispersion test. Fertil Steril. 2005; 84:833–842.28. Lewin A, Reubinoff B, Porat-Katz A, Weiss D, Eisenberg V, Arbel R, et al. Testicular fine needle aspiration: the alternative method for sperm retrieval in non-obstructive azoospermia. Hum Reprod. 1999; 14:1785–1790.
Article29. McLachlan RI, Rajpert-De Meyts E, Hoei-Hansen CE, de Kretser DM, Skakkebaek NE. Histological evaluation of the human testis--approaches to optimizing the clinical value of the assessment: mini review. Hum Reprod. 2007; 22:2–16.
Article30. Esteves SC, Varghese AC. Laboratory handling of epididymal and testicular spermatozoa: what can be done to improve sperm injections outcome. J Hum Reprod Sci. 2012; 5:233–243.
Article31. Schiff JD, Palermo GD, Veeck LL, Goldstein M, Rosenwaks Z, Schlegel PN. Success of testicular sperm extraction [corrected] and intracytoplasmic sperm injection in men with Klinefelter syndrome. J Clin Endocrinol Metab. 2005; 90:6263–6267.32. Sharpe RM, McKinnell C, Kivlin C, Fisher S. Proliferation and functional maturation of Sertoli cells, and their relevance to disorders of testis function in adulthood. Reproduction. 2003; 125:769–784.
Article33. Pasqualotto FF, Rossi-Ferragut LM, Rocha CC, Iaconelli A Jr, Borges E Jr. Outcome of in vitro fertilization and intracytoplasmic injection of epididymal and testicular sperm obtained from patients with obstructive and nonobstructive azoospermia. J Urol. 2002; 167:1753–1756.34. Ou L, Guo YH, Sun YP, Su YC. Outcomes of ICSI with microamount frozen-thawed sperm obtained by PESA or TESA in the treatment of azoospermia. Zhonghua Nan Ke Xue. 2010; 16:328–332.35. Silber SJ, Van Steirteghem AC, Liu J, Nagy Z, Tournaye H, Devroey P. High fertilization and pregnancy rate after intracytoplasmic sperm injection with spermatozoa obtained from testicle biopsy. Hum Reprod. 1995; 10:148–152.
Article36. Aamir J, Ashwini LS, Ganguly D, Murugan S, Muthiah SS, et al. Interpretation: real-time assessment on immotile but viable spermatozoa for intracytoplasmic sperm injection (ICSI): an embryologists outlook. Austin J In Vitro Fertili. 2015; 2:1021.37. Verheyen G, Popovic-Todorovic B, Tournaye H. Processing and selection of surgically-retrieved sperm for ICSI: a review. Basic Clin Androl. 2017; 27:6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracytoplasmic Sperm Injection Using Frozen-Thawed and Fresh Testicular Sperm in Patients with Azoospermia
- Influence on the Pregnancy Rate of Motility of Fresh and Frozen Testicular Spermatozoa in Obstructive Azoospermic Patients
- Decondensation and Pronucleus Formation of Human Spermatozoa Using Different Concentrations of PVP
- Comparison of ICSI Outcomes between Fresh and Cryopreserved-Thawed Testicular Spermatozoa
- Successful pregnancies using frozen thawed testicular sperm in ICSI program