Pediatr Gastroenterol Hepatol Nutr.
2019 Nov;22(6):594-600. 10.5223/pghn.2019.22.6.594.
Resolution of Protein-Losing Enteropathy after Congenital Heart Disease Repair by Selective Lymphatic Embolization
- Affiliations
-
- 1Department of Pediatrics, The University of Arizona College of Medicine, Tucson, AZ, USA. rkylat@gmail.com
- 2Department of Surgery, The University of Arizona College of Medicine, Tucson, AZ, USA.
- 3Center for Lymphatic Imaging and Interventions, Children's Hospital of Philadelphia, Philadelphia, PA, USA.
- KMID: 2462101
- DOI: http://doi.org/10.5223/pghn.2019.22.6.594
Abstract
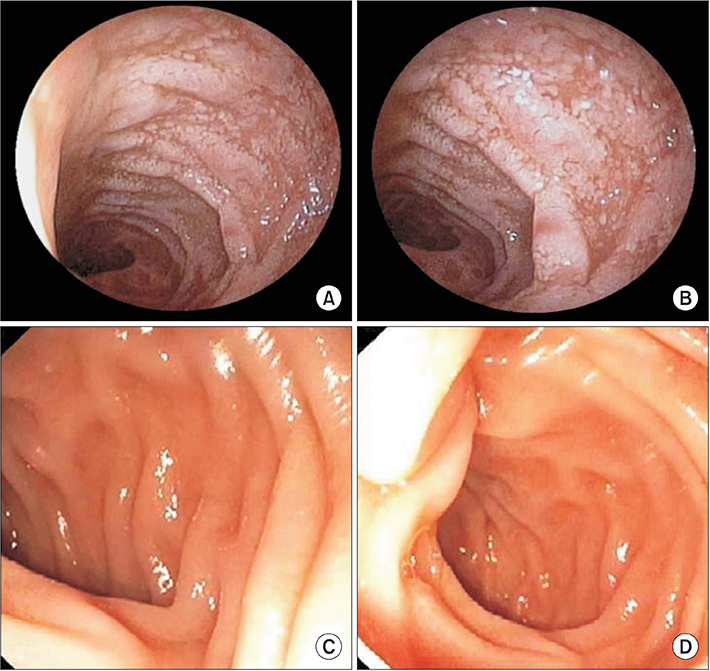
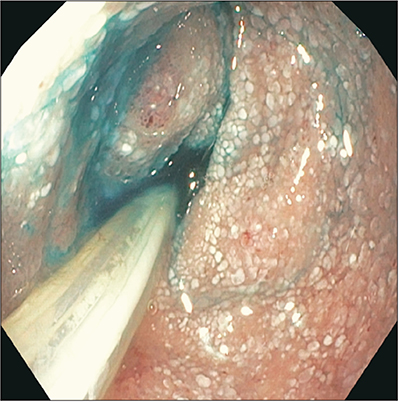
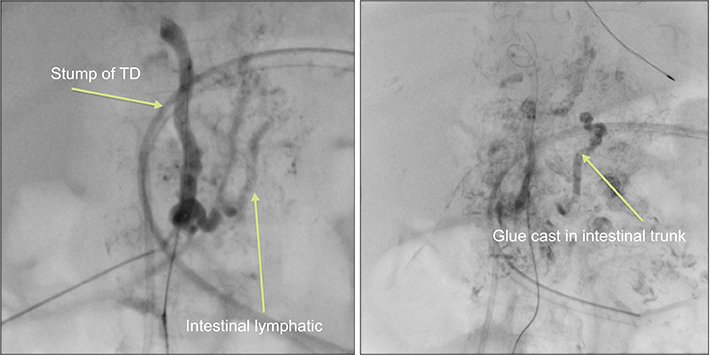
- With improving survival of children with complex congenital heart disease (CCHD), postoperative complications, like protein-losing enteropathy (PLE) are increasingly encountered. A 3-year-old girl with surgically corrected CCHD (ventricular inversion/L-transposition of the great arteries, ventricular septal defect, pulmonary atresia, post-double switch procedure [Rastelli and Glenn]) developed chylothoraces. She was treated with pleurodesis, thoracic duct ligation and subsequently developed chylous ascites and PLE (serum albumin ≤0.9 g/dL) and was malnourished, despite nutritional rehabilitation. Lymphangioscintigraphy/single-photon emission computed tomography showed lymphatic obstruction at the cisterna chyli level. A segmental chyle leak and chylous lymphangiectasia were confirmed by gastrointestinal endoscopy, magnetic resonance (MR) enterography, and MR lymphangiography. Selective glue embolization of leaking intestinal lymphatic trunks led to prompt reversal of PLE. Serum albumin level and weight gain markedly improved and have been maintained for over 3 years. Selective interventional embolization reversed this devastating lymphatic complication of surgically corrected CCHD.
Keyword
MeSH Terms
-
Adhesives
Arteries
Cardiac Surgical Procedures
Child
Child, Preschool
Chyle
Chylous Ascites
Embolization, Therapeutic
Endoscopy, Gastrointestinal
Female
Heart Defects, Congenital*
Heart Septal Defects, Ventricular
Humans
Ligation
Lymphatic Abnormalities
Lymphography
Pleurodesis
Postoperative Complications
Protein-Losing Enteropathies*
Pulmonary Atresia
Rehabilitation
Serum Albumin
Thoracic Duct
Tomography, Emission-Computed
Weight Gain
Adhesives
Serum Albumin
Figure
Reference
-
1. Greenwald DA. Protein-losing gastroenteropathy. In : Feldman M, Friedman L, Brandt L, editors. Sleisenger and Fordtran's gastrointestinal and liver disease. 10th ed. Philadelphia: Saunders;2016. p. 464–470.2. Levitt DG, Levitt MD. Protein losing enteropathy: comprehensive review of the mechanistic association with clinical and subclinical disease states. Clin Exp Gastroenterol. 2017; 10:147–168.
Article3. Johnson JN, Driscoll DJ, O'Leary PW. Protein-losing enteropathy and the Fontan operation. Nutr Clin Pract. 2012; 27:375–384.
Article4. Mertens L, Hagler DJ, Sauer U, Somerville J, Gewillig M. Protein-losing enteropathy after the Fontan operation: an international multicenter study. PLE study group. J Thorac Cardiovasc Surg. 1998; 115:1063–1073.
Article5. Malcic I, Sauer U, Stern H, Kellerer M, Kühlein B, Locher D, et al. The influence of pulmonary artery banding on outcome after the Fontan operation. J Thorac Cardiovasc Surg. 1992; 104:743–747.
Article6. John AS, Johnson JA, Khan M, Driscoll DJ, Warnes CA, Cetta F. Clinical outcomes and improved survival in patients with protein-losing enteropathy after the Fontan operation. J Am Coll Cardiol. 2014; 64:54–62.
Article7. Gleason WA Jr, Roodman ST, Laks H. Protein-losing enteropathy and intestinal lymphangiectasia after superior vena cava--right pulmonary artery (Glenn) shunt. J Thorac Cardiovasc Surg. 1979; 77:843–846.
Article8. Meadows J, Jenkins K. Protein-losing enteropathy: integrating a new disease paradigm into recommendations for prevention and treatment. Cardiol Young. 2011; 21:363–377.
Article9. Meadows J, Gauvreau K, Jenkins K. Lymphatic obstruction and protein-losing enteropathy in patients with congenital heart disease. Congenit Heart Dis. 2008; 3:269–276.
Article10. Rychik J, Spray TL. Strategies to treat protein-losing enteropathy. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2002; 5:3–11.
Article11. James H, Witte MH, Bernas M, Barber B. Proposal for prevention or alleviation of protein/lymph-losing enteropathy (PLE/LLE) after Fontan circulation treatment of univentricular hearts: restoration of lymph balance with a “lymphatic right-to-left shunt.”. Lymphology. 2016; 49:114–127.12. Petersen VP, Hastrup J. Protein-losing enteropathy in constrictive pericarditis. Acta Med Scand. 1963; 173:401–410.
Article13. António M, Gordo A, Pereira C, Pinto F, Fragata I, Fragata J. Thoracic duct decompression for protein-losing enteropathy in failing fontan circulation. Ann Thorac Surg. 2016; 101:2370–2373.
Article14. Connor FL, Angelides S, Gibson M, Larden DW, Roman MR, Jones O, et al. Successful resection of localized intestinal lymphangiectasia post-Fontan: role of (99m)technetium-dextran scintigraphy. Pediatrics. 2003; 112(3 Pt 1):e242–7.
Article15. Magdo HS, Stillwell TL, Greenhawt MJ, Stringer KA, Yu S, Fifer CG, et al. Immune abnormalities in Fontan protein-losing enteropathy: a case-control study. J Pediatr. 2015; 167:331–337.
Article16. Müller C, Wolf H, Göttlicher J, Zielinski CC, Eibl MM. Cellular immunodeficiency in protein-losing enteropathy. Predominant reduction of CD3+ and CD4+ lymphocytes. Dig Dis Sci. 1991; 36:116–122.17. Goldberg DJ, Dodds K, Avitabile CM, Glatz AC, Brodsky JL, Semeao EJ, et al. Children with protein-losing enteropathy after the Fontan operation are at risk for abnormal bone mineral density. Pediatr Cardiol. 2012; 33:1264–1268.
Article18. Guez D, Nadolski GJ, Pukenas BA, Itkin M. Transhepatic lymphatic embolization of intractable hepatic lymphorrhea. J Vasc Interv Radiol. 2014; 25:149–150.
Article19. Itkin M, Piccoli DA, Nadolski G, Rychik J, DeWitt A, Pinto E, et al. Protein-losing enteropathy in patients with congenital heart disease. J Am Coll Cardiol. 2017; 69:2929–2937.
Article20. Latson L. Once more unto the breach: a new treatment paradigm for protein-losing enteropathy. J Am Coll Cardiol. 2017; 69:2938–2940.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Protein-losing Enteropathy in Congestive Heart Failure : Resolution with Prednisolone
- Therapeutic Lymphatic Embolization in Pediatric Primary Intestinal Lymphangiectasia
- Primary protein-losing enteropathy : report of a case (idiopathic intestinal lymphangiectasia)
- A case of constrictive pericarditis presenting with protein-losing enteropathy
- A case of systemic lupus erythematosus with chylothorax, chronic interstitial cystitis and protein-losing enteropathy