J Korean Assoc Oral Maxillofac Surg.
2019 Oct;45(5):233-240. 10.5125/jkaoms.2019.45.5.233.
Management and prevention of third molar surgery-related trigeminal nerve injury: time for a rethink
- Affiliations
-
- 1Oral and Maxillofacial Surgery, Faculty of Dentistry, University of Hong Kong, Hong Kong. mikeyyleung@hku.hk
- KMID: 2461475
- DOI: http://doi.org/10.5125/jkaoms.2019.45.5.233
Abstract
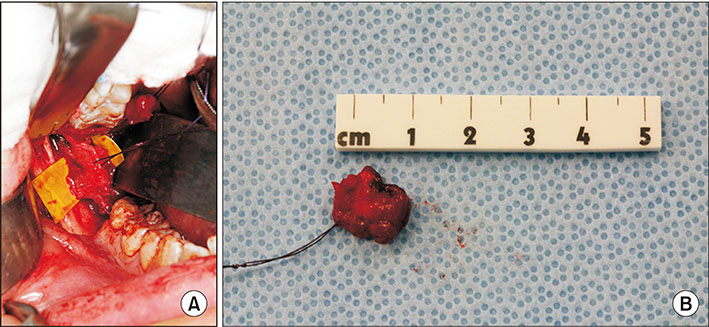
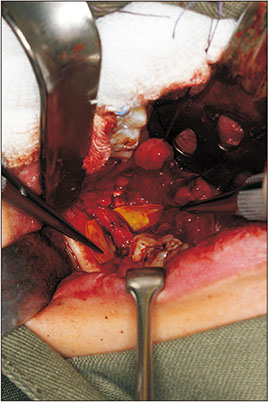
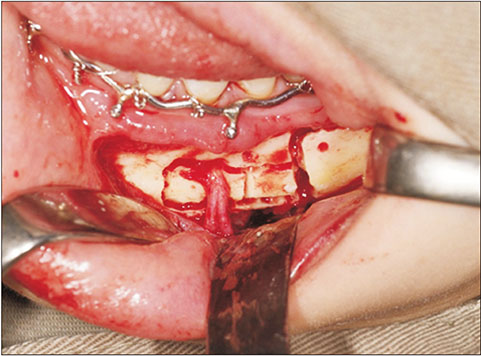
- Trigeminal nerve injury as a consequence of lower third molar surgery is a notorious complication and may affect the patient in long term. Inferior alveolar nerve (IAN) and lingual nerve (LN) injury result in different degree of neurosensory deficit and also other neurological symptoms. The long term effects may include persistent sensory loss, chronic pain and depression. It is crucial to understand the pathophysiology of the nerve injury from lower third molar surgery. Surgery remains the most promising treatment in moderate-to-severe nerve injuries. There are limitations in the current treatment methods and full recovery is not commonly achievable. It is better to prevent nerve injury than to treat with unpredictable results. Coronectomy has been proved to be effective in reducing IAN injury and carries minimal long-term morbidity. New technologies, like the roles of erythropoietin and stem cell therapy, are being investigated for neuroprotection and neural regeneration. Breakthroughs in basic and translational research are required to improve the clinical outcomes of the current treatment modalities of third molar surgery-related nerve injury.
Keyword
MeSH Terms
Figure
Reference
-
1. Haug RH, Abdul-Majid J, Blakey GH, White RP. Evidenced-based decision making: the third molar. Dent Clin North Am. 2009; 53:77–96. ix
Article2. Suter VGA, Rivola M, Schriber M, Leung YY, Bornstein MM. Risk factors for root resorption of second molars associated with impacted mandibular third molars. Int J Oral Maxillofac Surg. 2019; 48:801–809.
Article3. Bataineh AB. Sensory nerve impairment following mandibular third molar surgery. J Oral Maxillofac Surg. 2001; 59:1012–1017. discussion 1017.
Article4. Cheung LK, Leung YY, Chow LK, Wong MC, Chan EK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg. 2010; 39:320–326.
Article5. Lee CT, Zhang S, Leung YY, Li SK, Tsang CC, Chu CH. Patients' satisfaction and prevalence of complications on surgical extraction of third molar. Patient Prefer Adherence. 2015; 9:257–263.6. Leung YY, Cheung LK. Risk factors of neurosensory deficits in lower third molar surgery: a literature review of prospective studies. Int J Oral Maxillofac Surg. 2011; 40:1–10.
Article7. Kim JW, Cha IH, Kim SJ, Kim MR. Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral Maxillofac Surg. 2012; 70:2508–2514.
Article8. Leung YY, Cheung LK. Correlation of radiographic signs, inferior dental nerve exposure, and deficit in third molar surgery. J Oral Maxillofac Surg. 2011; 69:1873–1879.
Article9. Ghai S, Choudhury S. Role of panoramic imaging and cone beam CT for assessment of inferior alveolar nerve exposure and subsequent paresthesia following removal of impacted mandibular third molar. J Maxillofac Oral Surg. 2018; 17:242–247.
Article10. Pichler JW, Beirne OR. Lingual flap retraction and prevention of lingual nerve damage associated with third molar surgery: a systematic review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91:395–401.
Article11. Pogrel MA, Goldman KE. Lingual flap retraction for third molar removal. J Oral Maxillofac Surg. 2004; 62:1125–1130.
Article12. Leung YY, Fung PP, Cheung LK. Treatment modalities of neurosensory deficit after lower third molar surgery: a systematic review. J Oral Maxillofac Surg. 2012; 70:768–778.
Article13. Burchiel KJ. Abnormal impulse generation in focally demyelinated trigeminal roots. J Neurosurg. 1980; 53:674–683.
Article14. Meyer RA, Raja SN, Campbell JN, Mackinnon SE, Dellon AL. Neural activity originating from a neuroma in the baboon. Brain Res. 1985; 325:255–260.
Article15. Leung YY, McGrath C, Cheung LK. Trigeminal neurosensory deficit and patient reported outcome measures: the effect on quality of life. PLoS One. 2013; 8:e77391.
Article16. Leung YY, Lee TC, Ho SM, Cheung LK. Trigeminal neurosensory deficit and patient reported outcome measures: the effect on life satisfaction and depression symptoms. PLoS One. 2013; 8:e72891.
Article17. Leung YY, Cheung LK. Longitudinal treatment outcomes of microsurgical treatment of neurosensory deficit after lower third molar surgery: a prospective case series. PLoS One. 2016; 11:e0150149.
Article18. Devine M, Hirani M, Durham J, Nixdorf DR, Renton T. Identifying criteria for diagnosis of post-traumatic pain and altered sensation of the maxillary and mandibular branches of the trigeminal nerve: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018; 125:526–540.
Article19. Hillerup S, Stoltze K. Lingual nerve injury II. Observations on sensory recovery after micro-neurosurgical reconstruction. Int J Oral Maxillofac Surg. 2007; 36:1139–1145.20. Sandstedt P, Sörensen S. Neurosensory disturbances of the trigeminal nerve: a long-term follow-up of traumatic injuries. J Oral Maxillofac Surg. 1995; 53:498–505.21. Smith JG, Elias LA, Yilmaz Z, Barker S, Shah K, Shah S, et al. The psychosocial and affective burden of posttraumatic neuropathy following injuries to the trigeminal nerve. J Orofac Pain. 2013; 27:293–303.
Article22. Mackinnon SE. Surgical management of the peripheral nerve gap. Clin Plast Surg. 1989; 16:587–603.
Article23. Ziccardi VB, Zuniga JR. Nerve injuries after third molar removal. Oral Maxillofac Surg Clin North Am. 2007; 19:105–115. vii
Article24. Kiesselbach JE, Chamberlain JG. Clinical and anatomic observations on the relationship of the lingual nerve to the mandibular third molar region. J Oral Maxillofac Surg. 1984; 42:565–567.
Article25. Joshi A, Rood JP. External neurolysis of the lingual nerve. Int J Oral Maxillofac Surg. 2002; 31:40–43.
Article26. Robinson PP, Loescher AR, Smith KG. A prospective, quantitative study on the clinical outcome of lingual nerve repair. Br J Oral Maxillofac Surg. 2000; 38:255–263.
Article27. Millesi H. The current state of peripheral nerve surgery in the upper limb. Ann Chir Main. 1984; 3:18–34.
Article28. Pogrel MA, Maghen A. The use of autogenous vein grafts for inferior alveolar and lingual nerve reconstruction. J Oral Maxillofac Surg. 2001; 59:985–988. discussion 988–93.
Article29. Pogrel MA, McDonald AR, Kaban LB. Gore-Tex tubing as a conduit for repair of lingual and inferior alveolar nerve continuity defects: a preliminary report. J Oral Maxillofac Surg. 1998; 56:319–321. discussion 321–2.
Article30. Miloro M, Ruckman P 3rd, Kolokythas A. Lingual nerve repair: to graft or not to graft? J Oral Maxillofac Surg. 2015; 73:1844–1850.
Article31. Zuniga JR. Sensory outcomes after reconstruction of lingual and inferior alveolar nerve discontinuities using processed nerve allograft--a case series. J Oral Maxillofac Surg. 2015; 73:734–744.
Article32. LaBanc JP, Van Boven RW. Surgical management of inferior alveolar nerve injuries. Oral Maxillofac Surg Clin North Am. 1992; 4:425–437.
Article33. Pippi R, Spota A, Santoro M. Prevention of lingual nerve injury in third molar surgery: literature review. J Oral Maxillofac Surg. 2017; 75:890–900.
Article34. National Institute for Health and Care Excellence (NICE). Guidance on the extraction of wisdom teeth. London: NICE;2000.35. Mansoor J, Jowett A, Coulthard P. NICE or not so NICE? Br Dent J. 2013; 215:209–212.
Article36. Leung YY, Cheung LK. Can coronectomy of wisdom teeth reduce the incidence of inferior dental nerve injury? Ann R Australas Coll Dent Surg. 2008; 19:50–51.37. Leung YY, Cheung LK. Safety of coronectomy versus excision of wisdom teeth: a randomized controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:821–827.
Article38. Leung YY, Cheung LK. Coronectomy of the lower third molar is safe within the first 3 years. J Oral Maxillofac Surg. 2012; 70:1515–1522.
Article39. Leung YY, Cheung LK. Long-term morbidities of coronectomy on lower third molar. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016; 121:5–11.
Article40. Leung YY, Cheung KY. Root migration pattern after third molar coronectomy: a long-term analysis. Int J Oral Maxillofac Surg. 2018; 47:802–808.
Article41. Yeung AWK, Wong NSM, Bornstein MM, Leung YY. Three-dimensional radiographic evaluation of root migration patterns 4-8.5 years after lower third molar coronectomy: a cone beam computed tomography study. Int J Oral Maxillofac Surg. 2018; 47:1145–1152.
Article42. Yeung AWK, Wong NSM, Leung YY. Are coronectomy studies being cited? A bibliometric study. J Investig Clin Dent. 2019; 10:e12366.
Article43. Leung YY. Coronectomy of lower third molars with and without guided bony regeneration: a pilot study. Br J Oral Maxillofac Surg. 2016; 54:155–159.
Article44. Leung YY. Guided bone regeneration to reduce root migration after coronectomy of lower third molar: a randomized clinical trial. Clin Oral Investig. 2019; 23:1595–1604.
Article45. Brines ML, Ghezzi P, Keenan S, Agnello D, de Lanerolle NC, Cerami C, et al. Erythropoietin crosses the blood-brain barrier to protect against experimental brain injury. Proc Natl Acad Sci U S A. 2000; 97:10526–10531.
Article46. Ehrenreich H, Hasselblatt M, Dembowski C, Cepek L, Lewczuk P, Stiefel M, et al. Erythropoietin therapy for acute stroke is both safe and beneficial. Mol Med. 2002; 8:495–505.
Article47. Kaptanoglu E, Solaroglu I, Okutan O, Surucu HS, Akbiyik F, Beskonakli E. Erythropoietin exerts neuroprotection after acute spinal cord injury in rats: effect on lipid peroxidation and early ultrastructural findings. Neurosurg Rev. 2004; 27:113–120.
Article48. Shingo T, Sorokan ST, Shimazaki T, Weiss S. Erythropoietin regulates the in vitro and in vivo production of neuronal progenitors by mammalian forebrain neural stem cells. J Neurosci. 2001; 21:9733–9743.
Article49. Hall S. Nerve repair: a neurobiologist's view. J Hand Surg Br. 2001; 26:129–136.
Article50. Walsh S, Midha R. Practical considerations concerning the use of stem cells for peripheral nerve repair. Neurosurg Focus. 2009; 26:E2.
Article51. Techawattanawisal W, Nakahama K, Komaki M, Abe M, Takagi Y, Morita I. Isolation of multipotent stem cells from adult rat periodontal ligament by neurosphere-forming culture system. Biochem Biophys Res Commun. 2007; 357:917–923.
Article52. Pereira LV, Bento RF, Cruz DB, Marchi C, Salomone R, Oiticicca J, et al. Stem cells from human exfoliated deciduous teeth (SHED) differentiate in vivo and promote facial nerve regeneration. Cell Transplant. 2019; 28:55–64.
Article53. Harvey AR, Plant GW, Tan MM. Schwann cells and the regrowth of axons in the mammalian CNS: a review of transplantation studies in the rat visual system. Clin Exp Pharmacol Physiol. 1995; 22:569–579.
Article54. Shimizu S, Kitada M, Ishikawa H, Itokazu Y, Wakao S, Dezawa M. Peripheral nerve regeneration by the in vitro differentiated-human bone marrow stromal cells with Schwann cell property. Biochem Biophys Res Commun. 2007; 359:915–920.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- THE DIAGNOSIS OF TRIGEMINAL NERVE INJURY IN FACIAL TRAUMA BY TRIGEMINAL SOMATOSENSORY EVOKED POTENTIAL
- Meningioma related trigeminal neuralgia presenting as odontalgia: A case report
- Role of neuron and non-neuronal cell communication in persistent orofacial pain
- Maxillary Nerve Block for Patient with Trigeminal Neuralgia
- Sensory recovery after infraorbital nerve avulsion injury