Brain Tumor Res Treat.
2019 Oct;7(2):141-146. 10.14791/btrt.2019.7.e32.
Found at Old Age and Continuously Growing WHO Grade II Fourth Ventricle Ependymoma: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Pathology, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea.
- 3Department of Radiology, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea.
- 4Department of Cancer Control, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea. nsghs@ncc.re.kr
- KMID: 2461188
- DOI: http://doi.org/10.14791/btrt.2019.7.e32
Abstract
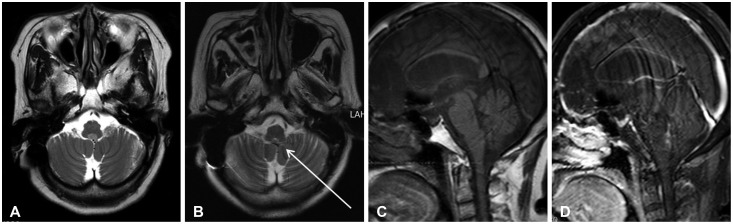
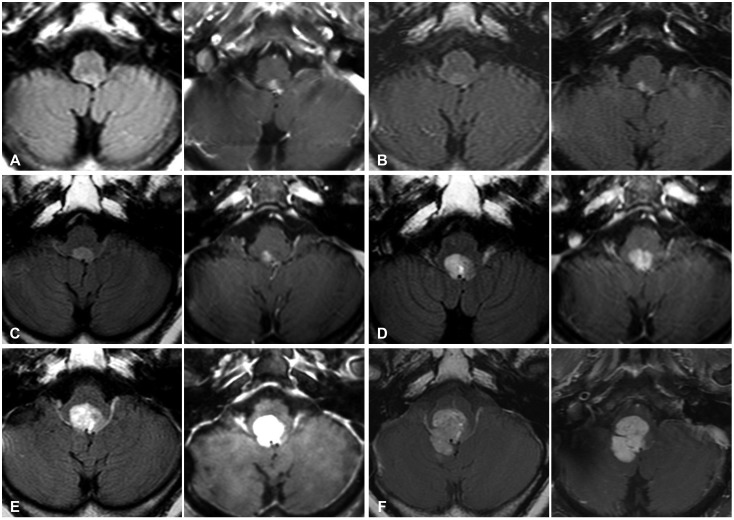
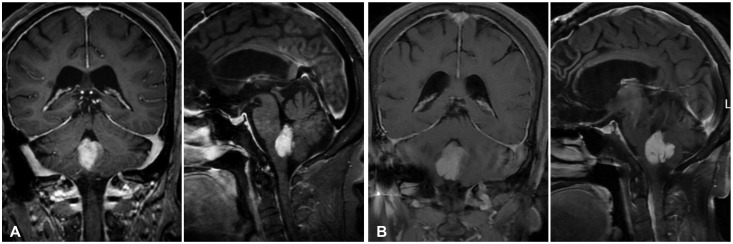
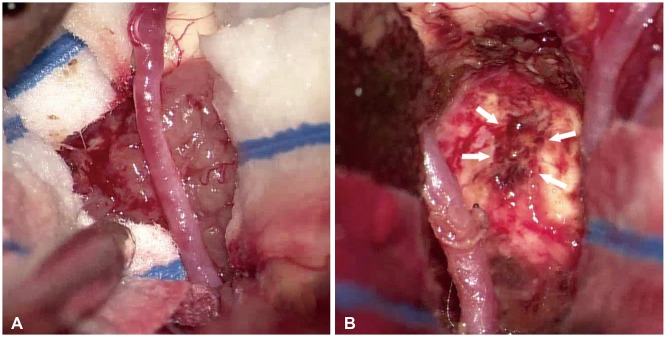
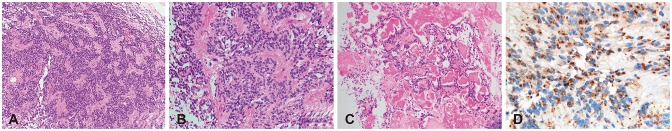
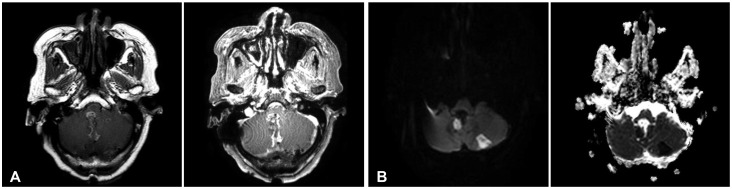
- A 74-year-old woman presented with a month-long nausea and vomiting, then she could not take a meal. She had found an asymptomatic 4th ventricular mass 6 year ago as a preoperative work-up for ovarian cancer. And during the yearly follow-up, the mass had grown continuously over 6 years, and caused symptoms in the seventh year. MRI revealed a large ovoid extra-axial mass in the fourth ventricle compressing adjacent medulla and cerebellum. Surgery achieved near total resection since the tumor tightly adhered to the brain stem of 4th ventricle floor. The histological diagnosis was ependymoma (WHO grade II). She transferred rehabilitation facility for mild gait disturbance, hoarseness and swallowing difficulty. Fourth ventricle ependymoma in the elderly is extremely rare and the growth rate has not been reported. Here, we present a rare care of 4th ventricle ependymoma found asymptomatic at elderly but continuously grow to cause local pressure symptoms.
Keyword
MeSH Terms
Figure
Reference
-
1. Metellus P, Guyotat J, Chinot O, et al. Adult intracranial WHO grade II ependymomas: long-term outcome and prognostic factor analysis in a series of 114 patients. Neuro Oncol. 2010; 12:976–984. PMID: 20484442.
Article2. Mork SJ, Loken AC. Ependymoma: a follow-up study of 101 cases. Cancer. 1977; 40:907–915. PMID: 890671.3. Guyotat J, Metellus P, Giorgi R, et al. Infratentorial ependymomas: prognostic factors and outcome analysis in a multi-center retrospective series of 106 adult patients. Acta Neurochir (Wien). 2009; 151:947–960. PMID: 19499166.
Article4. Jung TY, Jung S, Kook H, Baek HJ. Treatment decisions of World Health Organization grade II and III ependymomas in molecular era. J Korean Neurosurg Soc. 2018; 61:312–318. PMID: 29742878.
Article5. Hayashi T, Inamasu J, Kanai R, Sasaki H, Shinoda J, Hirose Y. Clinical, histological, and genetic features of fourth ventricle ependymoma in the elderly. Neurol Med Chir (Tokyo). 2012; 52:611–616. PMID: 22976148.
Article6. Ferguson SD, Levine NB, Suki D, et al. The surgical treatment of tumors of the fourth ventricle: a single-institution experience. J Neurosurg. 2018; 128:339–351. PMID: 28409732.
Article7. Amirian ES, Armstrong TS, Gilbert MR, Scheurer ME. Predictors of survival among older adults with ependymoma. J Neurooncol. 2012; 107:183–189. PMID: 21952907.
Article8. Jung HW, Yoo H, Paek SH, Choi KS. Long-term outcome and growth rate of subtotally resected petroclival meningiomas: experience with 38 cases. Neurosurgery. 2000; 46:567–574. discussion 574-5. PMID: 10719852.
Article9. Stangerup SE, Caye-Thomasen P, Tos M, Thomsen J. The natural history of vestibular schwannoma. Otol Neurotol. 2006; 27:547–552. PMID: 16791048.
Article10. Saito T, Oki S, Mikami T, et al. [Supratentorial ectopic ependymoma: a case report]. No Shinkei Geka. 1999; 27:1139–1144. PMID: 10629896.11. Ehtesham M, Kabos P, Yong WH, Schievink WI, Black KL, Yu JS. Development of an intracranial ependymoma at the site of a pre-existing cavernous malformation. Surg Neurol. 2003; 60:80–82. discussion 83. PMID: 12865022.
Article12. Sugawara T, Murakami R, Saito R, et al. [Two cases of ependymoma with atypical presentation]. Rinsho Hoshasen. 2003; 48:1218–1221.13. Araki T, Shimono T, Kuwabara M, et al. [Two cases of ependymoma with atypical presentation]. Rinsho Hoshasen. 2008; 53:1141–1145.14. Lord H, Ironside J, Summers D, Gregor A, Erridge S, Myles L. Fourth ventricle ependymoma in father and son. Br J Neurosurg. 2008; 22:423–425. PMID: 17952721.
Article15. Montano N, De Bonis P, Doglietto F, et al. Teaching NeuroImage: hemorrhagic ependymoma in the elderly: a rare cause of headache and gait imbalance. Neurology. 2008; 70:e95. PMID: 18519865.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Disseminated Intravascular Coagulation Developing Following Removal of Ependymoma in the 4th Ventricle: Case Report
- Hemangioblastoma of the Fourth Ventricle: Case Report
- Cerebellar Clear Cell Ependymoma in a 10-Year-Old Girl
- Trapped Fourth Ventricle: Case Report
- Multiple Spinal Cord Recurrences of an Intracranial Ependymoma after 14 Years