Cancer Res Treat.
2019 Oct;51(4):1285-1294. 10.4143/crt.2018.464.
Development of Protocol for Korean Lung Cancer Screening Project (K-LUCAS) to Evaluate Effectiveness and Feasibility to Implement National Cancer Screening Program
- Affiliations
-
- 1National Cancer Control Institute, National Cancer Center, Goyang, Korea. drheat@ncc.re.kr
- 2Department of Cancer Control and Population Health, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea.
- 3Department of Diagnostic Radiology, National Cancer Center, Goyang, Korea.
- 4Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 6Department of Pulmonary, Allergy and Critical Care Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 7Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 8Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea.
- 9Department of Family Medicine, Gachon University Gil Medical Center, Incheon, Korea.
- 10Department of Internal Medicine, Pusan National University, Busan, Korea.
- KMID: 2460578
- DOI: http://doi.org/10.4143/crt.2018.464
Abstract
- PURPOSE
To reduce lung cancer mortality, lung cancer screening was recommended using low-dose computed tomography (LDCT) to high-risk population. A protocol for multicenter lung cancer screening pilot project was developed to evaluate the effectiveness and feasibility of lung cancer screening to implement National Cancer Screening Program in Korea.
MATERIALS AND METHODS
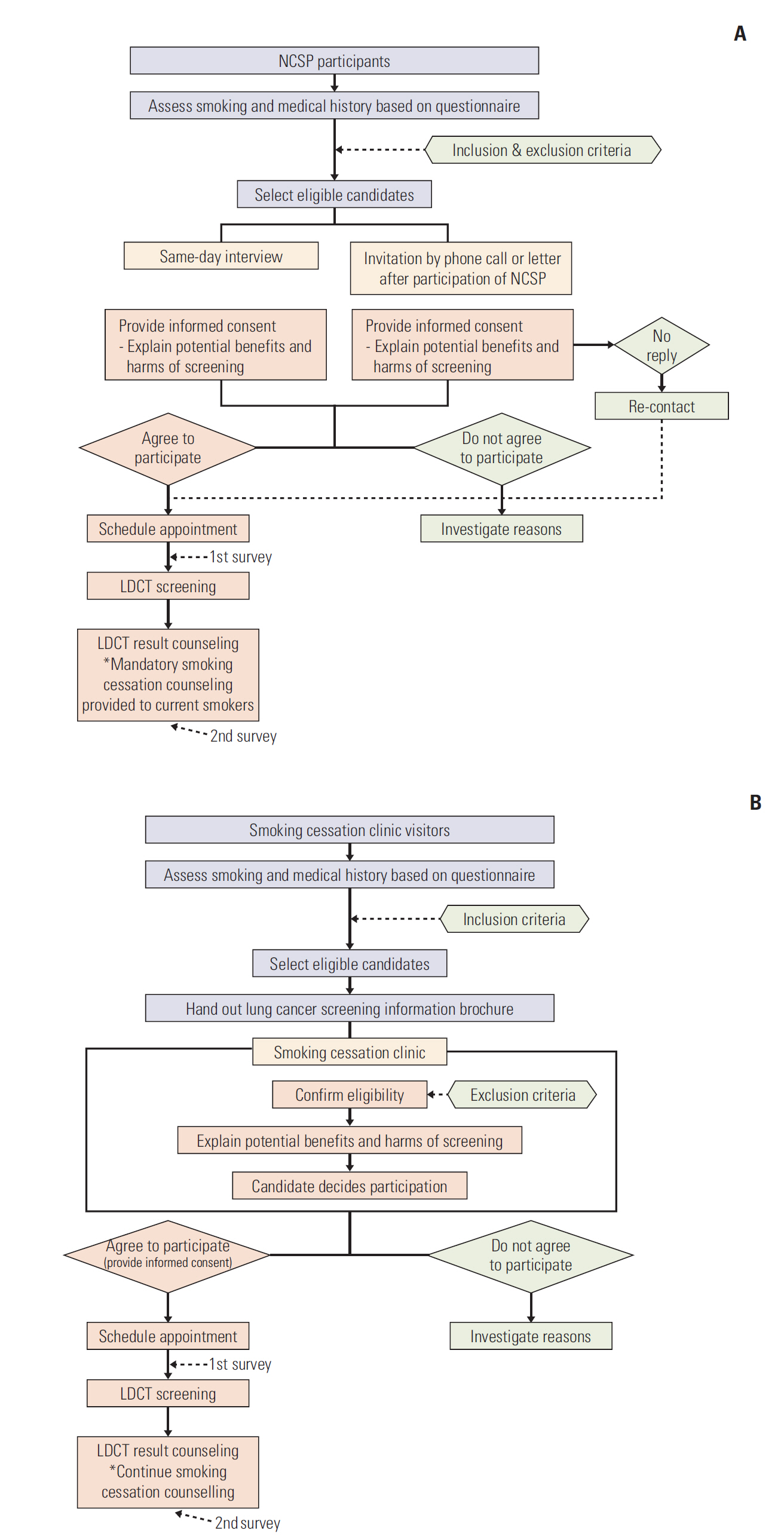
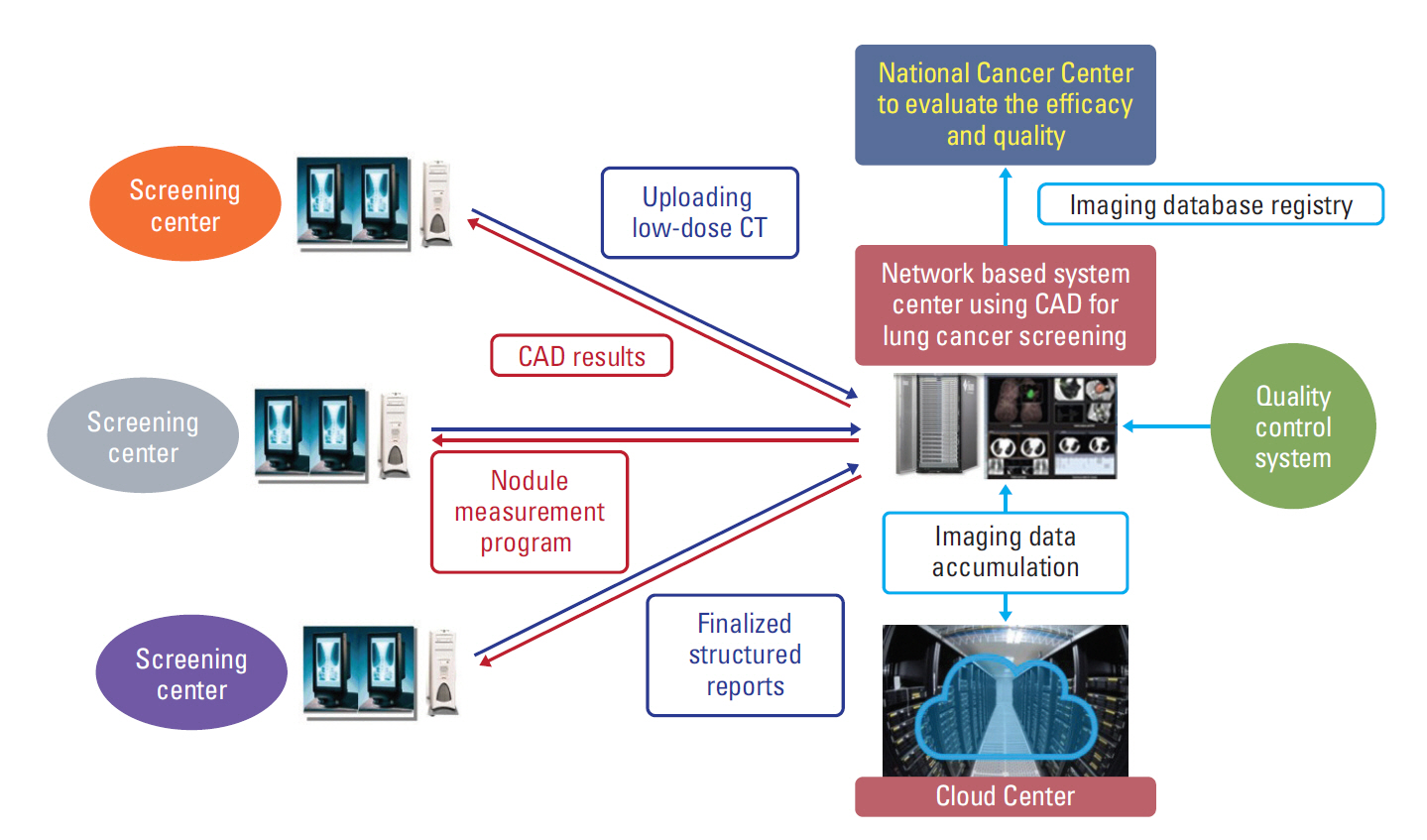
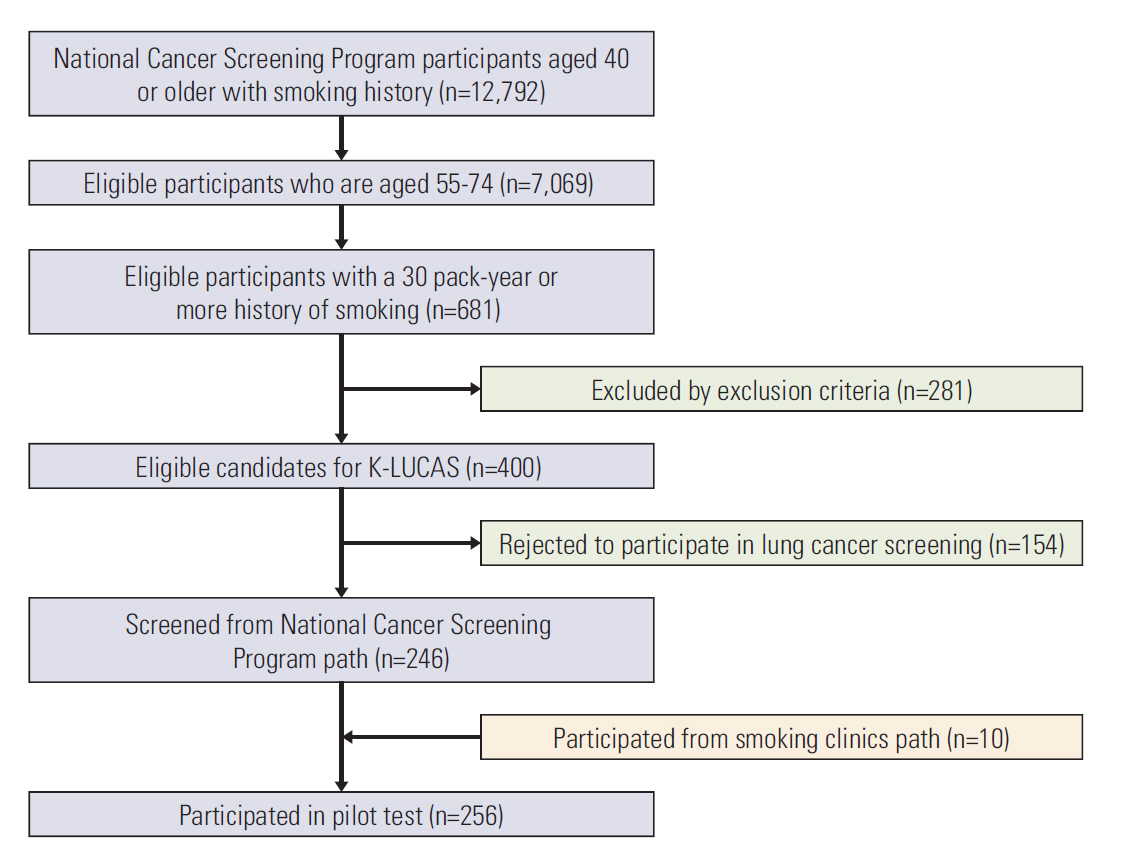
Multidisciplinary expert committee was comprised to develop a standardized protocol for Korean Lung Cancer Screening Project (K-LUCAS). K-LUCAS is a population-based single arm trial that targets high-risk population aged 55-74 years with at least 30 pack-year smoking history. LDCT results are reported by Lung-RADS suggested by American Radiology Society. Network-based system using computer-aided detection program is prepared to assist reducing diagnostic errors. Smoking cessation counselling is provided to all currently smoking participants. A small pilot test was conducted to check the feasibility and compliance of the protocols for K-LUCAS.
RESULTS
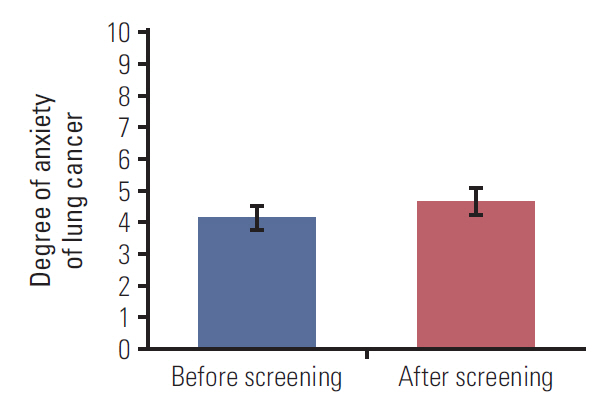
In pilot test, 256 were participated. The average age of participants was 63.2 years and only three participants (1.2%) were female. The participants had a smoking history of 40.5 pack-year on average and 53.9% were current smokers. Among them, 86.3% had willing to participate in lung cancer screening again. The average willingness to quit smoking among current smokers was 12.7% higher than before screening. In Lung-RADS reports, 10 (3.9%) were grade 3 and nine (3.5%) were grade 4. One participant was diagnosed as lung cancer.
CONCLUSION
The protocol developed by this study is assessed to be feasible to perform K-LUCAS in multicenter nationwide scale.
MeSH Terms
Figure
Cited by 2 articles
-
Evidence of National Lung Cancer Screening Program in Korea
Yeol Kim
Korean J Health Promot. 2019;19(4):161-165. doi: 10.15384/kjhp.2019.19.4.161.Cost Utility Analysis of a Pilot Study for the Korean Lung Cancer Screening Project
Juyoung Kim, Bogeum Cho, Seon-Ha Kim, Chang-Min Choi, Yeol Kim, Min-Woo Jo
Cancer Res Treat. 2022;54(3):728-736. doi: 10.4143/crt.2021.480.
Reference
-
References
1. International Agency for Research on Cancer. Fact Sheets by Cancer [Internet]. Lyon: International Agency for Research on Cancer;c2018. [cited 2018 Jun 18]. Available from: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.2. Jung KW, Won YJ, Kong HJ, Lee ES; Community of Population-Based Regional Cancer Registries. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat. 2018; 50:303–16.
Article3. Swensen SJ, Jett JR, Sloan JA, Midthun DE, Hartman TE, Sykes AM, et al. Screening for lung cancer with low-dose spiral computed tomography. Am J Respir Crit Care Med. 2002; 165:508–13.
Article4. Henschke CI, Miettinen OS, Yankelevitz DF, Libby DM, Smith JP. Radiographic screening for cancer. Proposed paradigm for requisite research. Clin Imaging. 1994; 18:16–20.
Article5. Kaneko M, Eguchi K, Ohmatsu H, Kakinuma R, Naruke T, Suemasu K, et al. Peripheral lung cancer: screening and detection with low-dose spiral CT versus radiography. Radiology. 1996; 201:798–802.
Article6. Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, et al. Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet. 1999; 354:99–105.
Article7. Fontana RS, Sanderson DR, Taylor WF, Woolner LB, Miller WE, Muhm JR, et al. Early lung cancer detection: results of the initial (prevalence) radiologic and cytologic screening in the Mayo Clinic study. Am Rev Respir Dis. 1984; 130:561–5.8. National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365:395–409.
Article9. U.S. Preventive Services Task Force. Final recommendation statement: lung cancer: screening [Internet]. Rockville, MD: US Preventive Services Task Force;c2018. [cited 2018 Jun 18]. Available from: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/lung-cancer-screening.10. Centers for Medicare & Medicaid Services. Decision Memo for Screening for Lung Cancer with Low Dose Computed Tomography (LDCT) (CAG-00439N) [Internet]. Baltimore, MD: Centers for Medicare & Medicaid Services;c2018. [cited 2018 Jun 18]. Available from: https://www.cms.gov/medicare-cover-age-database/details/nca-decision memo.aspx?NCAId=274.11. Jang SH, Sheen SS, Kim HY, Yim HW, Park BY, Kim JW, et al. The Korean guideline for lung cancer screening. J Korean Med Assoc. 2015; 58:291–301.
Article12. Eberth JM. Lung cancer screening with low-dose CT in the United States. J Am Coll Radiol. 2015; 12(12 Pt B):1395–402.
Article13. Lee JW, Kim HY, Goo JM, Kim EY, Lee SJ, Kim TJ, et al. Radiological report of pilot study for the Korean Lung Cancer Screening (K-LUCAS) Project: feasibility of implementing lung imaging reporting and data system. Korean J Radiol. 2018; 19:803–8.
Article14. American College of Radiology. Lung Imaging Reporting and Data System (Lung-RAD) [Internet]. Preston, VA: American College of Radiology;c2018. [cited 2018 Jun 18]. Available from: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads.15. McKee BJ, Regis SM, McKee AB, Flacke S, Wald C. Performance of ACR Lung-RADS in a clinical CT lung screening program. J Am Coll Radiol. 2015; 12:273–6.
Article16. Huang P, Park S, Yan R, Lee J, Chu LC, Lin CT, et al. Added value of computer-aided CT image features for early lung cancer diagnosis with small pulmonary nodules: a matched case-control study. Radiology. 2018; 286:286–95.
Article17. World Health Organization. Global tuberculosis report 2017. Geneva: World Health Organization;2017.18. Bach PB, Mirkin JN, Oliver TK, Azzoli CG, Berry DA, Brawley OW, et al. Benefits and harms of CT screening for lung cancer: a systematic review. JAMA. 2012; 307:2418–29.19. Taylor KL, Cox LS, Zincke N, Mehta L, McGuire C, Gelmann E. Lung cancer screening as a teachable moment for smoking cessation. Lung Cancer. 2007; 56:125–34.
Article20. Ostroff JS, Buckshee N, Mancuso CA, Yankelevitz DF, Henschke CI. Smoking cessation following CT screening for early detection of lung cancer. Prev Med. 2001; 33:613–21.
Article21. Byrne MM, Davila EP, Zhao W, Parker D, Hooper MW, CabanMartinez A, et al. Cancer screening behaviors among smokers and non-smokers. Cancer Epidemiol. 2010; 34:611–7.
Article22. Carreras G, Iannucci L, Costa G, Chellini E, Gorini G. Are smokers less likely to seek preventive healthcare measures in Italy? Eur J Cancer Prev. 2018; 27:507–13.
Article23. Quaife SL, McEwen A, Janes SM, Wardle J. Smoking is associated with pessimistic and avoidant beliefs about cancer: results from the International Cancer Benchmarking Partnership. Br J Cancer. 2015; 112:1799–804.
Article24. Wu GX, Raz DJ, Brown L, Sun V. Psychological burden associated with lung cancer screening: a systematic review. Clin Lung Cancer. 2016; 17:315–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evidence of National Lung Cancer Screening Program in Korea
- National Lung Cancer Screening in Korea: Introduction and Imaging Quality Control
- Strategies to Improve Smoking Cessation for Participants in Lung Cancer Screening Program: Analysis of Factors Associated with Smoking Cessation in Korean Lung Cancer Screening Project (K-LUCAS)
- Evidence-based National Cancer Screening program of Korea
- Screening for Lung Cancer