Cancer Res Treat.
2024 Jan;56(1):92-103. 10.4143/crt.2022.1598.
Strategies to Improve Smoking Cessation for Participants in Lung Cancer Screening Program: Analysis of Factors Associated with Smoking Cessation in Korean Lung Cancer Screening Project (K-LUCAS)
- Affiliations
-
- 1National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 2Department of Cancer Control and Population Health, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- 3Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Pulmonary, Allergy and Critical Care Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
- 5Department of Family Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
- 6Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 7Department of Diagnostic Radiology, National Cancer Center, Goyang, Korea
- 8Department of Radiology, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2550326
- DOI: http://doi.org/10.4143/crt.2022.1598
Abstract
- Purpose
Smoking cessation intervention is one of the key components of successful lung cancer screening program. We investigated the effectiveness and related factors of smoking cessation services provided to the participants in a population-based lung cancer screening trial.
Materials and Methods
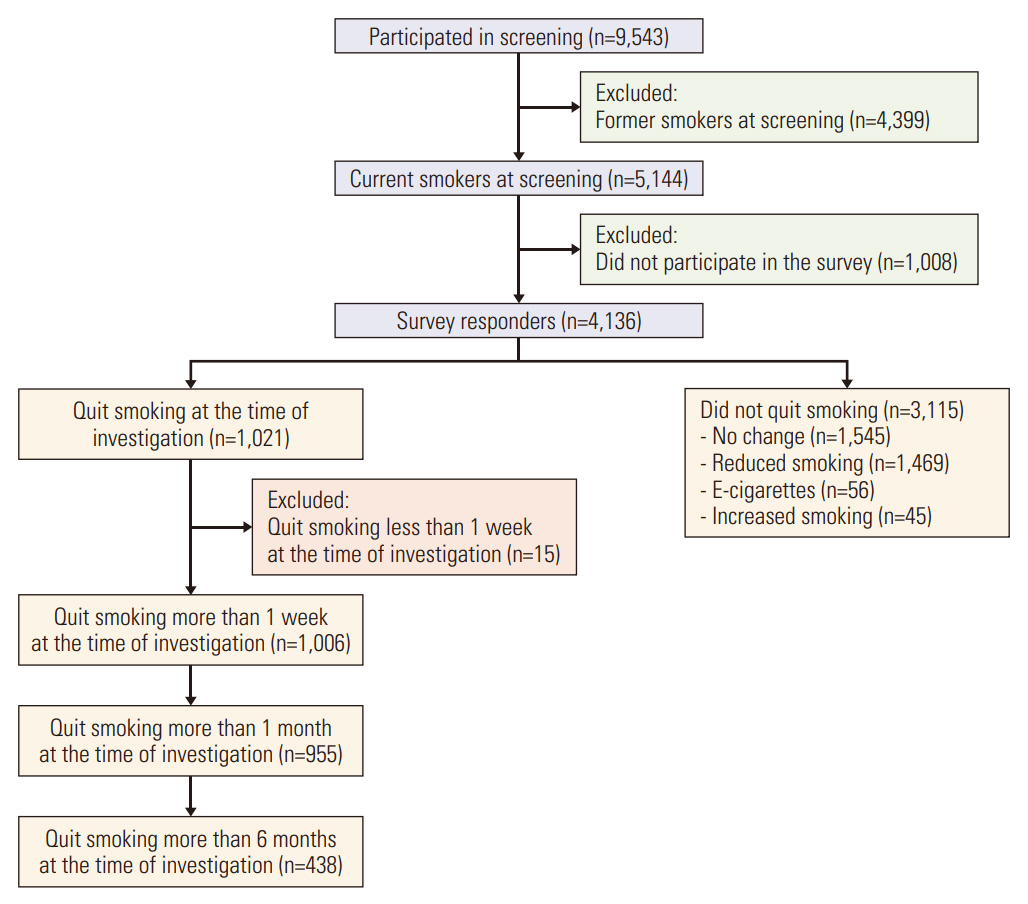
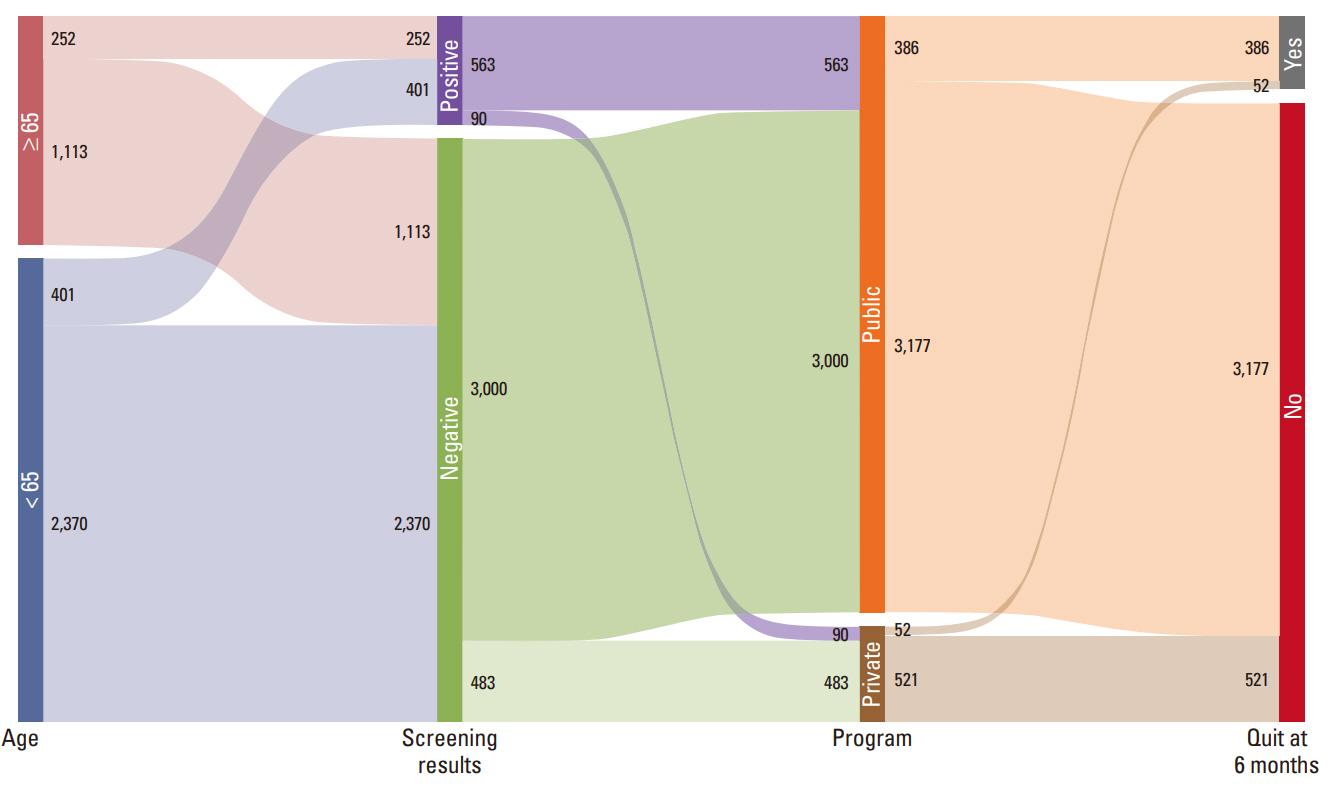
The Korean Lung Cancer Screening Project (K-LUCAS) is a nationwide, multi-center lung cancer screening trial that evaluates the feasibility of implementing population-based lung cancer screening. All 5,144 current smokers who participated in the K-LUCAS received a mandatory smoking cessation counseling. Changes in smoking status were followed up using a telephone survey in 6 months after lung cancer screening participation. The lung cancer screening’s impact on smoking cessation is analyzed by variations in the smoking cessation interventions provided in screening units.
Results
Among 4,136 survey responders, participant’s motivation to quit smoking increased by 9.4% on average after lung cancer screening. After 6 months from the initial screening, 24.3% of participants stopped smoking, and 10.6% of participants had not smoked continuously for at least 6 months after screening. Over 80% of quitters stated that participation in lung cancer screening motivated them to quit smoking. Low-cost public smoking cessation program combined with lung cancer screening increased the abstinence rates. The smokers were three times more likely to quit smoking when the smoking cessation counseling was provided simultaneously with low-dose computed tomography screening results than when provided separately.
Conclusion
A mandatory smoking cessation intervention integrated with screening result counselling by a physician after participation in lung cancer screening could be effective for increasing smoking cessation attempts.
Figure
Reference
-
References
1. Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Niksic M, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018; 391:1023–75.2. National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365:395–409.3. Oudkerk M, Devaraj A, Vliegenthart R, Henzler T, Prosch H, Heussel CP, et al. European position statement on lung cancer screening. Lancet Oncol. 2017; 18:e754–66.4. de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020; 382:503–13.5. Lynge E, Tornberg S, von Karsa L, Segnan N, van Delden JJ. Determinants of successful implementation of population-based cancer screening programmes. Eur J Cancer. 2012; 48:743–8.6. Burns DM. Tobacco-related diseases. Semin Oncol Nurs. 2003; 19:244–9.7. Taylor KL, Cox LS, Zincke N, Mehta L, McGuire C, Gelmann E. Lung cancer screening as a teachable moment for smoking cessation. Lung Cancer. 2007; 56:125–34.8. Lee J, Kim Y, Kim HY, Goo JM, Lim J, Lee CT, et al. Feasibility of implementing a national lung cancer screening program: interim results from the Korean Lung Cancer Screening Project (K-LUCAS). Transl Lung Cancer Res. 2021; 10:723–36.9. Lee J, Lim J, Kim Y, Kim HY, Goo JM, Lee CT, et al. Development of protocol for Korean Lung Cancer Screening Project (K-LUCAS) to evaluate effectiveness and feasibility to implement National Cancer Screening Program. Cancer Res Treat. 2019; 51:1285–94.10. Cho YK, Kang YM, Yoo JH, Lee J, Park JY, Lee WJ, et al. Implications of the dynamic nature of metabolic health status and obesity on risk of incident cardiovascular events and mortality: a nationwide population-based cohort study. Metabolism. 2019; 97:50–6.11. American College of Radiology. Lung Imaging Reporting and Data System (Lung-RAD) [Internet]. Reston, VA: American College of Radiology;c2018. [cited 2018 Jun 18]. Available from: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads.12. McMahon PM, Kong CY, Bouzan C, Weinstein MC, Cipriano LE, Tramontano AC, et al. Cost-effectiveness of computed tomography screening for lung cancer in the United States. J Thorac Oncol. 2011; 6:1841–8.13. Ashraf H, Saghir Z, Dirksen A, Pedersen JH, Thomsen LH, Dossing M, et al. Smoking habits in the randomised Danish Lung Cancer Screening Trial with low-dose CT: final results after a 5-year screening programme. Thorax. 2014; 69:574–9.14. Brain K, Carter B, Lifford KJ, Burke O, Devaraj A, Baldwin DR, et al. Impact of low-dose CT screening on smoking cessation among high-risk participants in the UK Lung Cancer Screening Trial. Thorax. 2017; 72:912–8.15. van der Aalst CM, van den Bergh KA, Willemsen MC, de Koning HJ, van Klaveren RJ. Lung cancer screening and smoking abstinence: 2 year follow-up data from the DutchBelgian randomised controlled lung cancer screening trial. Thorax. 2010; 65:600–5.16. Pistelli F, Aquilini F, Falaschi F, Puliti D, Ocello C, Lopes Pegna A, et al. Smoking cessation in the ITALUNG lung cancer screening: what does “teachable moment” mean? Nicotine Tob Res. 2020; 22:1484–91.17. Bade M, Bahr V, Brandt U, Eigentopf A, Bruchert T, Gross ML, et al. Effect of smoking cessation counseling within a randomised study on early detection of lung cancer in Germany. J Cancer Res Clin Oncol. 2016; 142:959–68.18. Han MA. The price of tobacco and its effects on smoking behaviors in Korea: the 2015 Korea Community Health Survey. Prev Med. 2019; 120:71–7.19. Hughes JR, Carpenter MJ, Naud S. Do point prevalence and prolonged abstinence measures produce similar results in smoking cessation studies? a systematic review. Nicotine Tob Res. 2010; 12:756–62.20. Huang WH, Hsu HY, Chang BC, Chang FC. Factors correlated with success rate of outpatient smoking cessation services in Taiwan. Int J Environ Res Public Health. 2018; 15:1218.21. Eum YH, Kim HJ, Bak S, Lee SH, Kim J, Park SH, et al. Factors related to the success of smoking cessation: a retrospective cohort study in Korea. Tob Induc Dis. 2022; 20:15.22. Regan EA, Lowe KE, Make BJ, Lynch DA, Kinney GL, Budoff MJ, et al. Identifying smoking-related disease on lung cancer screening CT scans: increasing the value. Chronic Obstr Pulm Dis. 2019; 6:233–45.23. Ravenel JG, Nance JW. Coronary artery calcification in lung cancer screening. Transl Lung Cancer Res. 2018; 7:361–7.24. Hall DL, Neil JM, Ostroff JS, Hawari S, O’Cleirigh C, Park ER. Perceived cancer-related benefits of quitting smoking and associations with quit intentions among recently diagnosed cancer patients. J Health Psychol. 2021; 26:831–42.25. Moldovanu D, de Koning HJ, van der Aalst CM. Lung cancer screening and smoking cessation efforts. Transl Lung Cancer Res. 2021; 10:1099–109.26. Tammemagi MC, Berg CD, Riley TL, Cunningham CR, Taylor KL. Impact of lung cancer screening results on smoking cessation. J Natl Cancer Inst. 2014; 106:dju084.27. Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014; 4:e006414.28. Lindson-Hawley N, Thompson TP, Begh R. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2015; (3):CD006936.29. Piper ME, Bullen C, Krishnan-Sarin S, Rigotti NA, Steinberg ML, Streck JM, et al. Defining and measuring abstinence in clinical trials of smoking cessation interventions: an updated review. Nicotine Tob Res. 2020; 22:1098–106.30. Cadham CJ, Jayasekera JC, Advani SM, Fallon SJ, Stephens JL, Braithwaite D, et al. Smoking cessation interventions for potential use in the lung cancer screening setting: a systematic review and meta-analysis. Lung Cancer. 2019; 135:205–16.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evidence of National Lung Cancer Screening Program in Korea
- Smoking Cessation
- National Lung Cancer Screening in Korea: Introduction and Imaging Quality Control
- Development of Protocol for Korean Lung Cancer Screening Project (K-LUCAS) to Evaluate Effectiveness and Feasibility to Implement National Cancer Screening Program
- Lung Cancer: Overview