Pediatr Gastroenterol Hepatol Nutr.
2019 Sep;22(5):447-452. 10.5223/pghn.2019.22.5.447.
Is There a Need for Bowel Management after Surgery for Isolated Intestinal Malrotation in Children?
- Affiliations
-
- 1Department of Pediatric Surgery, Skåne University Hospital, Lund, Sweden. martin.salo@med.lu.se
- 2Department of Clinical Sciences, Pediatrics, Lund University, Lund, Sweden.
- KMID: 2457746
- DOI: http://doi.org/10.5223/pghn.2019.22.5.447
Abstract
- PURPOSE
Few studies have reported non-acute long-term morbidity rates in children with intestinal malrotation. The aim of this study was to investigate the rate of constipation in children undergoing Ladd's procedure for isolated intestinal malrotation.
METHODS
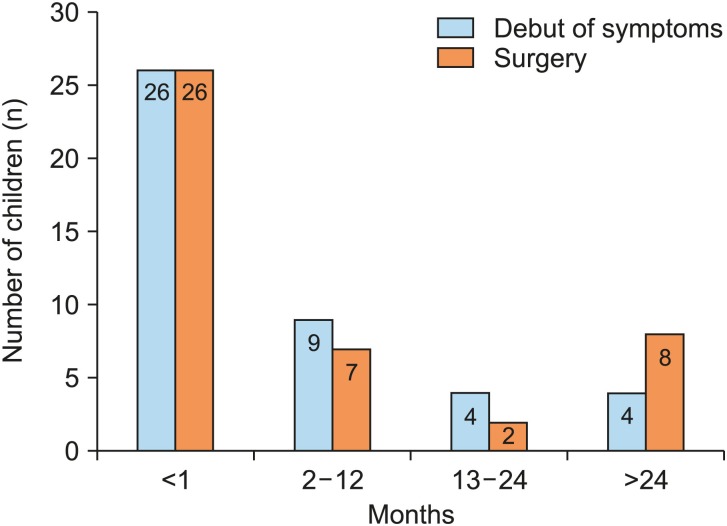
This retrospective study included children aged <15 years who underwent Ladd's procedure for intestinal malrotation between 2001 and 2016. Demographics, presence of volvulus perioperatively, need for bowel resection, short term (<30 days) and long-term complications, including mortality were recorded. Constipation was defined as treatment with laxatives at 1-year follow-up.
RESULTS
Of the 43 children included in the study, 49% were boys. The median age at surgery was 28 days (0-5, 293 days). Volvulus occurred in 26 children (60.5%), and bowel resection was required in 4 children (9.3%). Short-term complications categorized as grades II-V according to the Clavien-Dindo classification occurred in 13 children (30.2%). Of these, 5 children (11.6%) required re-operation. Constipation was observed in 9 children (23.7%) at the 1-year follow-up. No difference was observed in the rate of perioperative volvulus between children with and without constipation (44% vs. 65%, p=0.45). Excluding re-operations performed within 30 days after surgery, 3 children (6%) underwent surgery for intestinal obstruction during the study period.
CONCLUSION
Many children undergoing Ladd's procedure require bowel management even at long-term follow-up, probably secondary to constipation. It is important to thoroughly evaluate bowel function at the time of follow-up to verify or exclude constipation, and if treatment of constipation is unsuccessful, these children require evaluation for dysmotility disorders and/or intestinal neuronal dysplasia.
Keyword
MeSH Terms
Figure
Reference
-
1. Dilley AV, Pereira J, Shi EC, Adams S, Kern IB, Currie B, et al. The radiologist says malrotation: does the surgeon operate? Pediatr Surg Int. 2000; 16:45–49. PMID: 10663834.
Article2. Devane SP, Coombes R, Smith VV, Bisset WM, Booth IW, Lake BD, et al. Persistent gastrointestinal symptoms after correction of malrotation. Arch Dis Child. 1992; 67:218–221. PMID: 1543383.
Article3. Coombs RC, Buick RG, Gornall PG, Corkery JJ, Booth IW. Intestinal malrotation: the role of small intestinal dysmotility in the cause of persistent symptoms. J Pediatr Surg. 1991; 26:553–556. PMID: 2061809.
Article4. Feitz R, Vos A. Malrotation: the postoperative period. J Pediatr Surg. 1997; 32:1322–1324. PMID: 9314253.
Article5. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.6. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.7. Murphy FL, Sparnon AL. Long-term complications following intestinal malrotation and the Ladd's procedure: a 15 year review. Pediatr Surg Int. 2006; 22:326–329. PMID: 16518597.8. Husberg B, Salehi K, Peters T, Gunnarsson U, Michanek M, Nordenskjöld A, et al. Congenital intestinal malrotation in adolescent and adult patients: a 12-year clinical and radiological survey. Springerplus. 2016; 5:245. PMID: 27026938.
Article9. Van Den Berg MM, Benninga MA, Di Lorenzo C. Epidemiology of childhood constipation: a systematic review. Am J Gastroenterol. 2006; 101:2401–2409. PMID: 17032205.
Article10. Saps M, Nichols-Vinueza DX, Rosen JM, Velasco-Benítez CA. Prevalence of functional gastrointestinal disorders in Colombian school children. J Pediatr. 2014; 164:542–545.e1. PMID: 24332822.11. Loening-Baucke V. Prevalence rates for constipation and faecal and urinary incontinence. Arch Dis Child. 2007; 92:486–489. PMID: 16857698.
Article12. Kyrklund K, Koivusalo A, Rintala RJ, Pakarinen MP. Evaluation of bowel function and fecal continence in 594 Finnish individuals aged 4 to 26 years. Dis Colon Rectum. 2012; 55:671–676. PMID: 22595847.
Article13. Lindgren H, Nejstgaard MC, Salö M, Stenström P. Evaluation of bowel function in healthy children: untreated constipation is common. Acta Paediatr. 2018; 107:875–885. PMID: 29344986.
Article14. Mehall JR, Chandler JC, Mehall RL, Jackson RJ, Wagner CW, Smith SD. Management of typical and atypical intestinal malrotation. J Pediatr Surg. 2002; 37:1169–1172. PMID: 12149695.
Article15. Stauffer UG, Herrmann P. Comparison of late results in patients with corrected intestinal malrotation with and without fixation of the mesentery. J Pediatr Surg. 1980; 15:9–12. PMID: 7365665.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Review of Symptomatic Intestinal Malrotation
- Intestinal Malrotation with Concurrent Portal Vein and Superior Mesenteric Vein Thromboses
- Various Imaging Features of Intestinal Malrotation, Associated Anomalies, and Complications
- Intestinal Malrotation With a Fixed Partial Volvulus in an Adult
- A Case of Intestinal Malrotation with Midgut Volvulus Presenting with Intermittent Vomiting and Abdominal Pain