J Korean Soc Radiol.
2010 Jun;62(6):597-605.
Various Imaging Features of Intestinal Malrotation, Associated Anomalies, and Complications
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Cheonan Hospital, Korea. ytokim@schca.ac.kr
Abstract
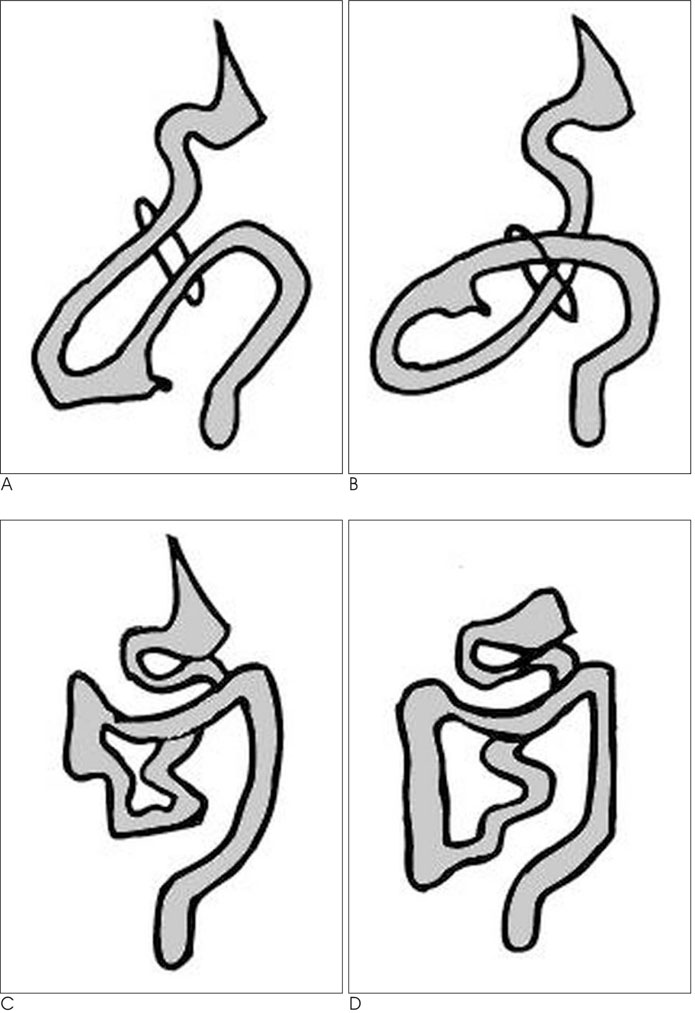
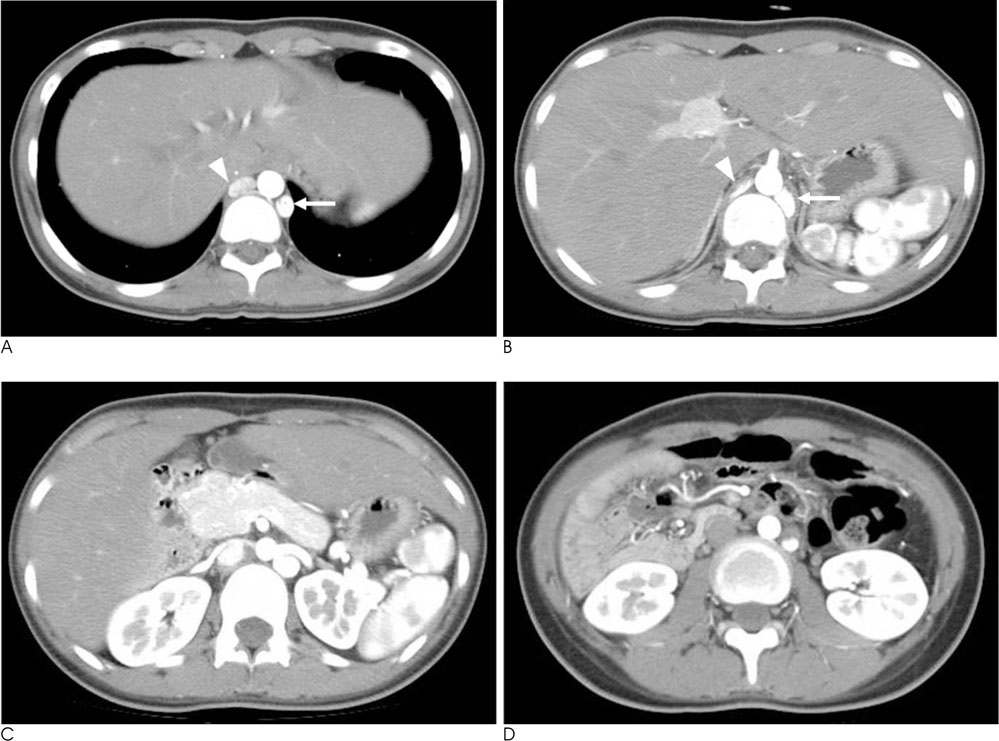
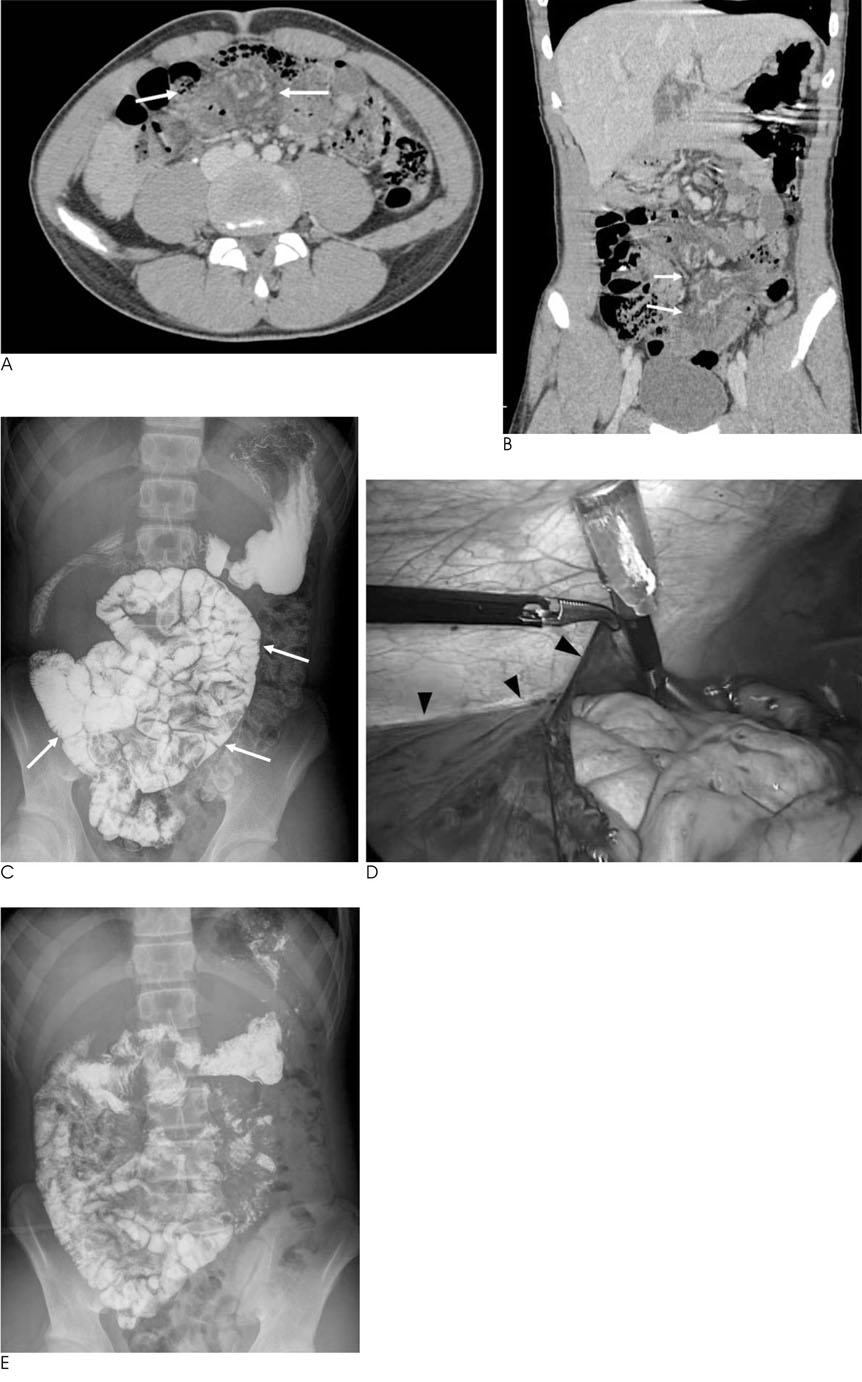
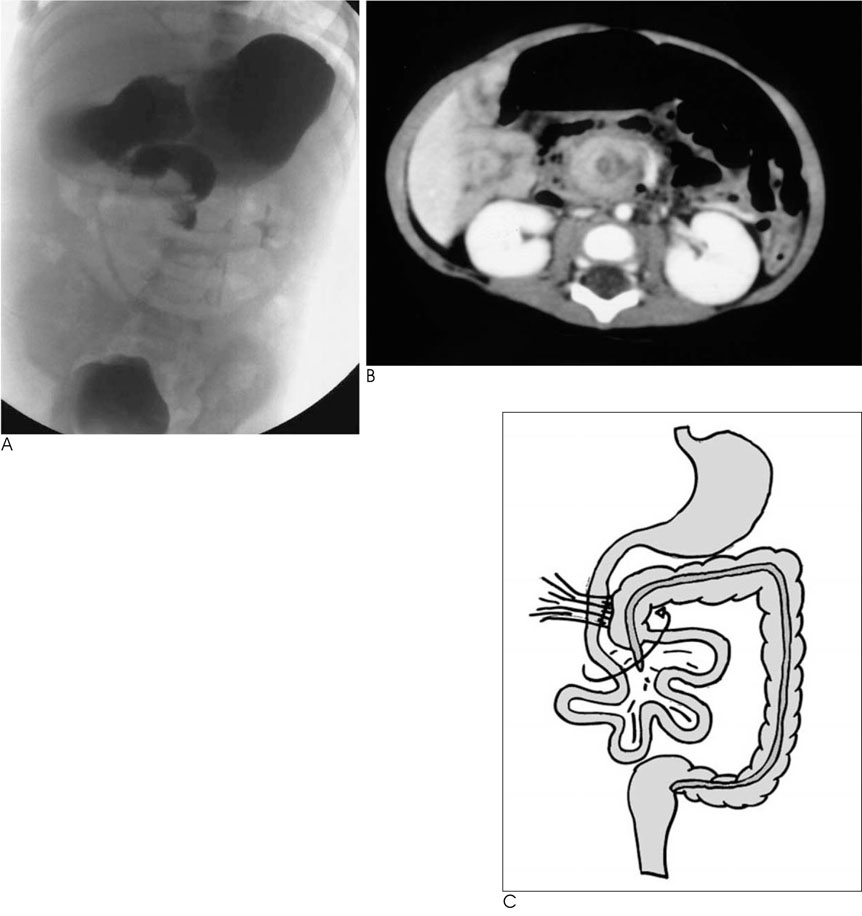
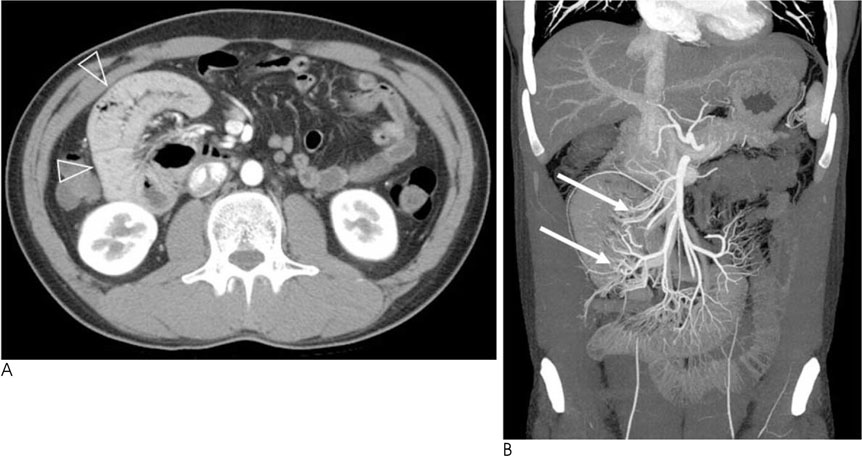
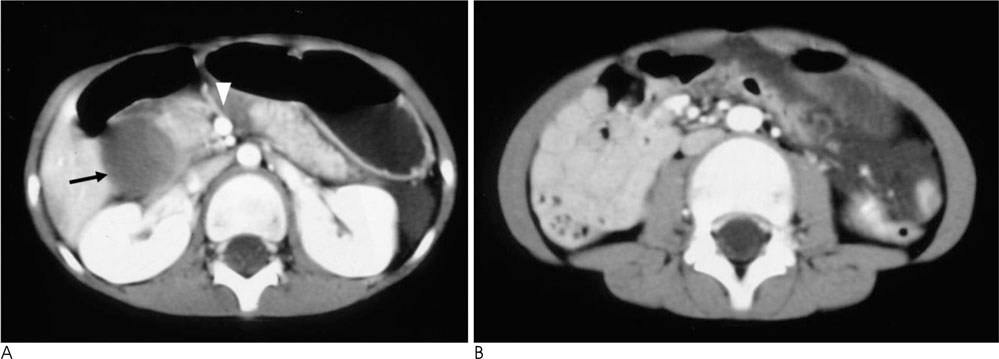
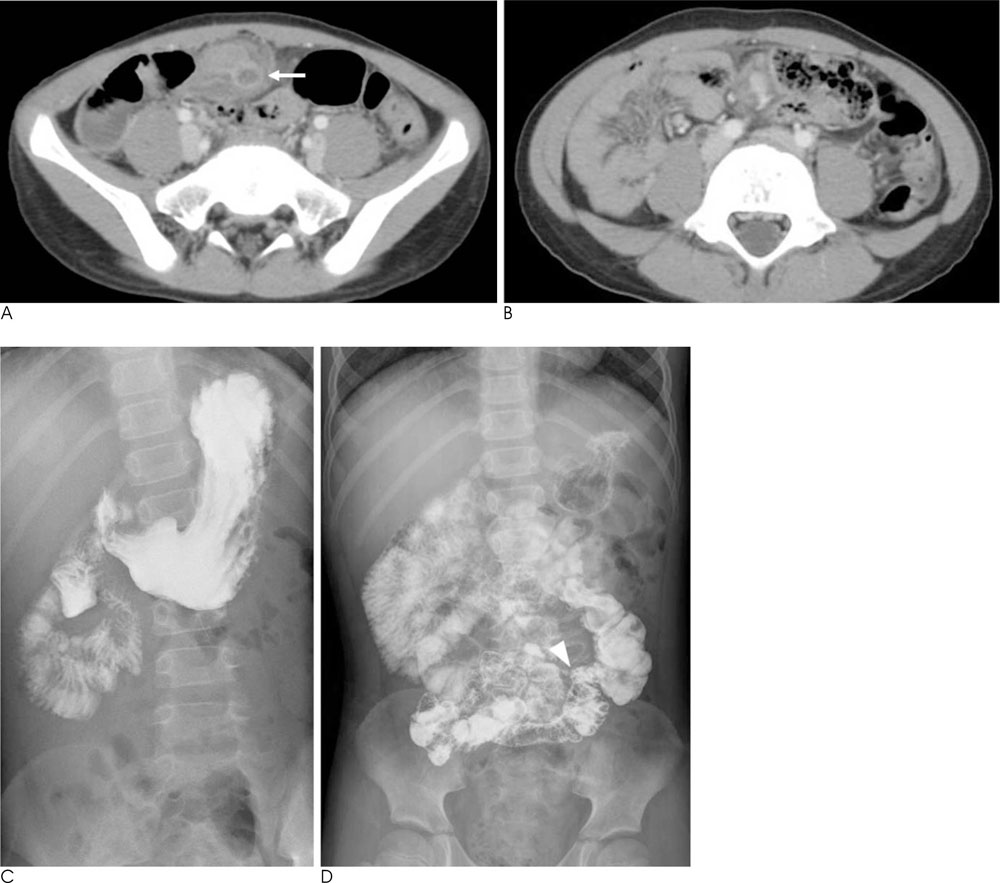
- An abnormal rotation or fixation of the small and large bowel may occur during development, and can result in various forms of intestinal malrotation. Intestinal malrotations are associated with anomalies such as heterotaxy and peritoneal encapsulation, as well as various other complications including midgut volvulus and an internal hernia. Gastrointestinal disorders occurring in patients with intestinal malrotation are difficult to diagnose because of the atypical symptoms and imaging features. We illustrate the various imaging features of intestinal malrotation, associated anomalies, and complications.
MeSH Terms
Figure
Reference
-
1. Applegate KE, Anderson JM, Klatte EC. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006; 26:1485–1500.2. Gore RM, Levine MS. Textbook of gastrointestinal radiology. 3rd ed. Philadelphia: Saunders;2008. p. 2188–2192.3. Pickhardt PJ, Bhalla S. Intestinal malrotation in adolescents and adults: spectrum of clinical and imaging features. AJR Am J Roentgenol. 2002; 179:1429–1435.4. Slovis TL. Caffey's pediatric diagnostic imaging. 11th ed. Philadelphia: Mosby/Elsevier;2008. p. 2106–2116.5. Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2002; 22:1439–1456.6. Chew MH, Sophian Hadi I, Chan G, Ong HS, Wong WK. A problem encapsulated: the rare peritoneal encapsulation syndrome. Singapore Med J. 2006; 47:808–810.7. Wig JD, Gupta SK. Computed tomography in abdominal cocoon. J Clin Gastroenterol. 1998; 26:156–157.8. Tombak MC, Apaydin FD, Colak T, Duce MN, Balci Y, Yazici M, et al. An unusual cause of intestinal obstruction: abdominal cocoon. AJR Am J Roentgenol. 2010; 194:W176–W178.9. Lin JN, Lou CC, Wang KL. Intestinal malrotation and midgut volvulus: a 15-year review. J Formos Med Assoc. 1995; 94:178–181.10. Welte FJ, Grosso M. Left-sided appendicitis in a patient with congenital gastrointestinal malrotation: a case report. J Med Case Rep. 2007; 1:92.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Sided Appendicitis in Patient with Intestinal Malrotation
- A Case of Duodenal Web Associated with Intestinal Malrotation
- Malrotation and Midgut Volvulus in Children: Diagnostic Approach, Imaging Findings, and Pitfalls
- Midgut Volvulus in a 70-year-old Man Due to Intestinal Nonrotation
- Malrotation complicating Midgut Volvulus: Ultrasonographic Finding