Acute Crit Care.
2019 Aug;34(3):202-211. 10.4266/acc.2019.00563.
Reduction of PaCOâ‚‚ by high-flow nasal cannula in acute hypercapnic respiratory failure patients receiving conventional oxygen therapy
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. sangmin2@snu.ac.kr
- KMID: 2457678
- DOI: http://doi.org/10.4266/acc.2019.00563
Abstract
- BACKGROUND
It has been suggested that a high-flow nasal cannula (HFNC) could help to remove carbon dioxide (CO2) from anatomical dead spaces, but evidence to support that is lacking. The objective of this study was to elucidate whether use of an HFNC could reduce the arterial partial pressure of CO2 (PaCO2) in patients with acute hypercapnic respiratory failure who are receiving conventional oxygen (O2) therapy.
METHODS
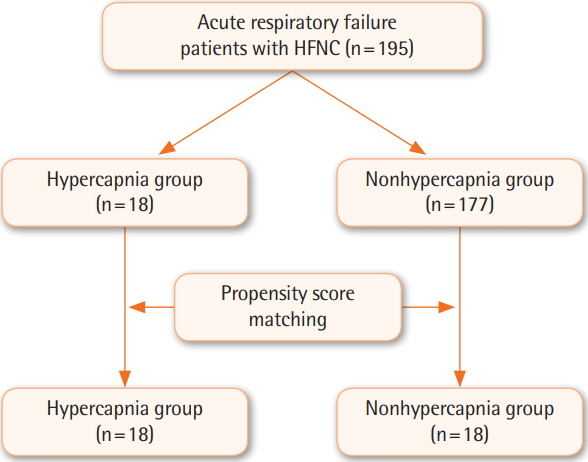
A propensity score-matched observational study was conducted to evaluate patients treated with an HFNC for acute hypercapnic respiratory failure from 2015 to 2016. The hypercapnia group was defined as patients with a PaCO2 >50 mm Hg and arterial pH <7.35.
RESULTS
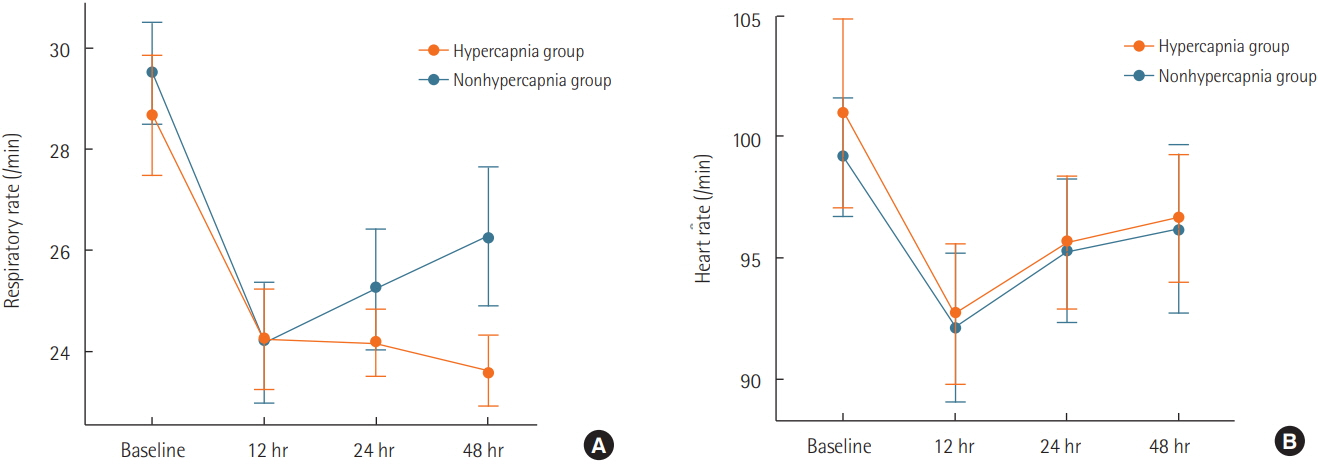
Eighteen patients in the hypercapnia group and 177 patients in the nonhypercapnia group were eligible for the present study. Eighteen patients in each group were matched by propensity score. Decreased PaCO2 and consequent pH normalization over time occurred in the hypercapnia group (P=0.002 and P=0.005, respectively). The initial PaCO2 level correlated linearly with PaCO2 removal after the use of an HFNC (R2=0.378, P=0.010). The fraction of inspired O2 used in the intensive care unit was consistently higher for 48 hours in the nonhypercapnia group. Physiological parameters such as respiratory rate and arterial partial pressure of O2 improved over time in both groups.
CONCLUSIONS
Physiological parameters can improve after the use of an HFNC in patients with acute hypercapnic respiratory failure given low-flow O2 therapy via a facial mask. Further studies are needed to identify which hypercapnic patients might benefit from an HFNC.
MeSH Terms
Figure
Cited by 2 articles
-
Successful noninvasive ventilation in a severely acidotic and hypercapnic comatose COVID-19 patient with multiple comorbidities: a case report
Joseph Abraham Poonuraparampil, Habib Md Reazaul Karim, Manu P Kesavankutty, Porika Prashanth Nayak
Acute Crit Care. 2022;37(1):120-123. doi: 10.4266/acc.2020.00983.Comparison of preoxygenation with a high-flow nasal cannula and a simple face mask before intubation in Korean patients with head and neck cancer
Jun-Young Jo, Jungpil Yoon, Heeyoon Jang, Wook-Jong Kim, Seungwoo Ku, Seong-Soo Choi
Acute Crit Care. 2024;39(1):61-69. doi: 10.4266/acc.2022.01543.
Reference
-
1. Hernández G, Roca O, Colinas L. High-flow nasal cannula support therapy: new insights and improving performance. Crit Care. 2017; 21:62.
Article2. Curley GF, Laffy JG, Zhang H, Slutsky AS. Noninvasive respiratory support for acute respiratory failure-high flow nasal cannula oxygen or non-invasive ventilation? J Thorac Dis. 2015; 7:1092–7.3. Nishimura M. High-flow nasal cannula oxygen therapy in adults. J Intensive Care. 2015; 3:15.
Article4. Dysart K, Miller TL, Wolfson MR, Shaffer TH. Research in high flow therapy: mechanisms of action. Respir Med. 2009; 103:1400–5.
Article5. Sztrymf B, Messika J, Mayot T, Lenglet H, Dreyfuss D, Ricard JD. Impact of high-flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care. 2012; 27:324–e9-13.
Article6. Itagaki T, Okuda N, Tsunano Y, Kohata H, Nakataki E, Onodera M, et al. Effect of high-flow nasal cannula on thoraco-abdominal synchrony in adult critically ill patients. Respir Care. 2014; 59:70–4.
Article7. Möller W, Celik G, Feng S, Bartenstein P, Meyer G, Oliver E, et al. Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol (1985). 2015; 118:1525–32.
Article8. Mündel T, Feng S, Tatkov S, Schneider H. Mechanisms of nasal high flow on ventilation during wakefulness and sleep. J Appl Physiol (1985). 2013; 114:1058–65.
Article9. Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF. Oxygen delivery through high-flow nasal cannulae increase endexpiratory lung volume and reduce respiratory rate in postcardiac surgical patients. Br J Anaesth. 2011; 107:998–1004.
Article10. Riera J, Pérez P, Cortés J, Roca O, Masclans JR, Rello J. Effect of high-flow nasal cannula and body position on end-expiratory lung volume: a cohort study using electrical impedance tomography. Respir Care. 2013; 58:589–96.
Article11. Davidson AC, Banham S, Elliott M, Kennedy D, Gelder C, Glossop A, et al. BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax. 2016; 71 Suppl 2:ii1–35.
Article12. Diaz O, Iglesia R, Ferrer M, Zavala E, Santos C, Wagner PD, et al. Effects of noninvasive ventilation on pulmonary gas exchange and hemodynamics during acute hypercapnic exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997; 156:1840–5.
Article13. Schönhofer B, Sortor-Leger S. Equipment needs for noninvasive mechanical ventilation. Eur Respir J. 2002; 20:1029–36.14. Mehta S, Hill NS. Noninvasive ventilation. Am J Respir Crit Care Med. 2001; 163:540–77.
Article15. Fraser JF, Spooner AJ, Dunster KR, Anstey CM, Corley A. Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomized crossover trial. Thorax. 2016; 71:759–61.16. Bräunlich J, Köhler M, Wirtz H. Nasal highflow improves ventilation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016; 11:1077–85.
Article17. Chatila W, Nugent T, Vance G, Gaughan J, Criner GJ. The effects of high-flow vs low-flow oxygen on exercise in advanced obstructive airways disease. Chest. 2004; 126:1108–15.
Article18. Pilcher J, Eastlake L, Richards M, Power S, Cripps T, Bibby S, et al. Physiological effects of titrated oxygen via nasal highflow cannulae in COPD exacerbations: a randomized controlled cross-over trial. Respirology. 2017; 22:1149–55.
Article19. British Thoracic Society Standards of Care Committee. Noninvasive ventilation in acute respiratory failure. Thorax. 2002; 57:192–211.20. Rawat D, Sharma S. Hypercapnea. Treasure Island: StatPearls Publishing. 2019.21. Jubran A. Rapid shallow breathing: causes and consequences. In : Mancebo J, Net A, Brochard L, editors. Mechanical ventilation and weaning. Berlin, Heidelberg: Springer Berlin-Heidelberg;2002. p. 161–8.22. Miro AM, Shivaram U, Hertig I. Continuous positive airway pressure in COPD patients in acute hypercapnic respiratory failure. Chest. 1993; 103:266–8.
Article23. Jaoude P, Kufel T, El-Solh AA. Survival benefit of CPAP favors hypercapnic patients with the overlap syndrome. Lung. 2014; 192:251–8.
Article24. Mauri T, Eronia N, Turrini C, Grasselli G, Bellani G, Pesenti A. High flow nasal cannula improves lung aeration and enhances CO2 removal in hypoxemic critically ill patients. Intensive Care Med Exp. 2015; 3:A176.
Article25. Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ. 2010; 341:c5462.
Article26. Chang GY, Cox CA, Shaffer TH. Nasal cannula, CPAP, and highflow nasal cannula: effect of flow on temperature, humidity, pressure, and resistance. Biomed Instrum Technol. 2011; 45:69–74.
Article27. Jeffrey AA, Warren PM, Flenley DC. Acute hypercapnic respiratory failure in patients with chronic obstructive lung disease: risk factors and use of guidelines for management. Thorax. 1992; 47:34–40.
Article28. Lee CC, Mankodi D, Shaharyar S, Ravindranathan S, Danckers M, Herscovici P, et al. High flow nasal cannula versus conventional oxygen therapy and non-invasive ventilation in adults with acute hypoxemic respiratory failure: a systematic review. Respir Med. 2016; 121:100–8.
Article29. Coudroy R, Jamet A, Petua P, Robert R, Frat JP, Thille AW. Highflow nasal cannula oxygen therapy versus noninvasive ventilation in immunocompromised patients with acute respiratory failure: an observational cohort study. Ann Intensive Care. 2016; 6:45.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study on the Changes of SaO2, According to the Different Type of Oxygen Suppliers
- Factors about Failure after High Flow Oxygen through Nasal Cannula Therapy in Hypoxic Respiratory Failure Patients at Emergency Department Presentation
- Treatment of acute respiratory failure: high-flow nasal cannula
- High-flow nasal cannula for respiratory failure in adult patients
- High-flow nasal cannula oxygen therapy in children: a clinical review