J Korean Neuropsychiatr Assoc.
2019 Aug;58(3):252-258. 10.4306/jknpa.2019.58.3.252.
A Patient with the Disrupted Sleep-Wake Rhythm after Traumatic Brain Injury
- Affiliations
-
- 1Department of Psychiatry, Kangwon National University Hospital, Chuncheon, Korea. jhielee@kangwon.ac.kr
- 2Department of Neurology, Kangwon National University Hospital, Chuncheon, Korea.
- 3Department of Psychiatry, Kangwon National University School of Medicine, Chuncheon, Korea.
- KMID: 2456606
- DOI: http://doi.org/10.4306/jknpa.2019.58.3.252
Abstract
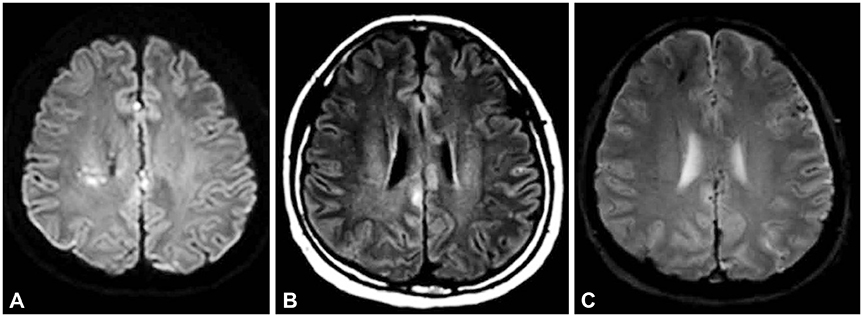
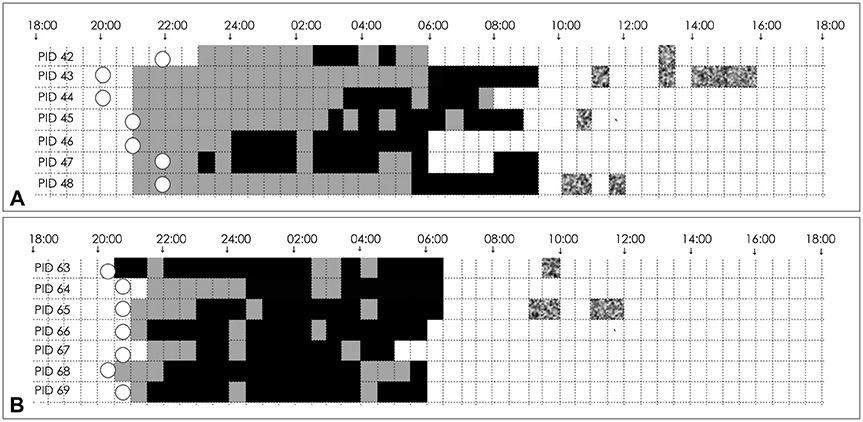
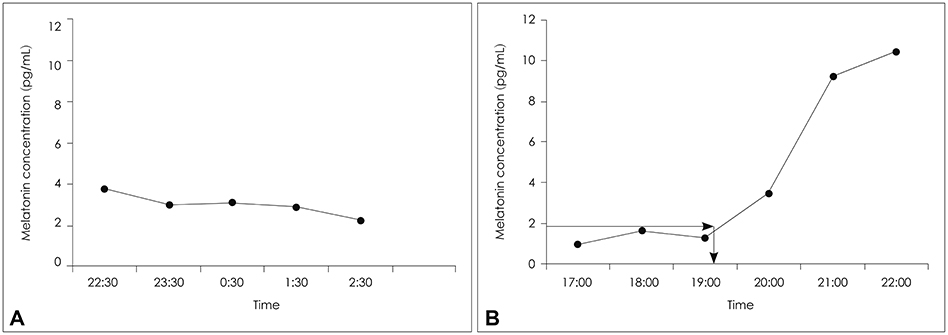
- Many patients with a traumatic brain injury (TBI) experience a range of sleep problems. Although some studies investigated the pathophysiology of sleep-wake cycle disturbances in TBI patients, it has not been clarified. This paper presents a middle aged female patient who showed sleep deprivation and sleep-wake cycle disturbances for approximately three months after TBI. The improvement in the subjective and objective sleep quality was shown by the sleep diary and actigraphy during this period. Moreover, the dim light melatonin onset (DLMO) had been delayed before returning to the normal range in 3 months. In addition, the patient showed an improvement in the neurocognitive function, including attention, memory and language function, along with a consolidation of the sleep-wake cycle. This case showed that the sleep disturbance following a TBI was probably caused by the disrupted melatonin rhythm based on the abnormality of the DLMO. In addition, the cognitive dysfunction after TBI could be associated with sleep-wake cycle disturbances because its gradual improvement occurred as the sleep disturbance diminished. Further studies on the change in circadian rhythm after a brain injury related to neurocognitive impairment are required.
MeSH Terms
Figure
Reference
-
1. Ouellet MC, Beaulieu-Bonneau S, Morin CM. Sleep-wake disturbances after traumatic brain injury. Lancet Neurol. 2015; 14:746–757.
Article2. Duclos C, Dumont M, Wiseman-Hakes C, Arbour C, Mongrain V, Gaudreault PO, et al. Sleep and wake disturbances following traumatic brain injury. Pathol Biol (Paris). 2014; 62:252–261.
Article3. Werner JK Jr, Baumann CR. TBI and sleep-wake disorders: pathophysiology, clinical management, and moving towards the future. Semin Neurol. 2017; 37:419–432.
Article4. Moore RY, Speh JC, Leak RK. Suprachiasmatic nucleus organization. Cell Tissue Res. 2002; 309:89–98.
Article5. Lewy AJ, Emens J, Songer J, Rough J. The neurohormone melatonin as a marker, medicament, and mediator. In : Pfaff DW, Arnold AP, Etgen AM, Fahrbach SE, Rubin RT, editors. Hormones, Brain and Behavior. 2nd ed. New York, NY: Elsevier;2010. p. 2505–2528.6. Shekleton JA, Parcell DL, Redman JR, Phipps-Nelson J, Ponsford JL, Rajaratnam SM. Sleep disturbance and melatonin levels following traumatic brain injury. Neurology. 2010; 74:1732–1738.
Article7. Duclos C, Dumont M, Blais H, Paquet J, Laflamme E, de Beaumont L, et al. Rest-activity cycle disturbances in the acute phase of moderate to severe traumatic brain injury. Neurorehabil Neural Repair. 2014; 28:472–482.
Article8. Malec JF, Brown AW, Leibson CL, Flaada JT, Mandrekar JN, Diehl NN, et al. The mayo classification system for traumatic brain injury severity. J Neurotrauma. 2007; 24:1417–1424.
Article9. Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998; 21:871–881.
Article10. Quinto C, Gellido C, Chokroverty S, Masdeu J. Posttraumatic delayed sleep phase syndrome. Neurology. 2000; 54:250–252.
Article11. Duclos C, Dumont M, Blais H, Paquet J, Quinn MJ, Menon DK, et al. Melatonin secretion and the rest-activity cycle in the acute phase of moderate-severe traumatic brain injury. Brain Inj. 2014; 28:657–658.12. Steele DL, Rajaratnam SM, Redman JR, Ponsford JL. The effect of traumatic brain injury on the timing of sleep. Chronobiol Int. 2005; 22:89–105.
Article13. Ayalon L, Borodkin K, Dishon L, Kanety H, Dagan Y. Circadian rhythm sleep disorders following mild traumatic brain injury. Neurology. 2007; 68:1136–1140.
Article14. Grima NA, Ponsford JL, St Hilaire MA, Mansfield D, Rajaratnam SM. Circadian melatonin rhythm following traumatic brain injury. Neurorehabil Neural Repair. 2016; 30:972–977.
Article15. Piotrowicz K, Klich-Rączka A, Pac A, Zdzienicka A, Grodzicki T. The diurnal profile of melatonin during delirium in elderly patients--preliminary results. Exp Gerontol. 2015; 72:45–49.
Article16. Ángeles-Castellanos M, Ramírez-Gonzalez F, Ubaldo-Reyes L, Rodriguez-Mayoral O, Escobar C. Loss of melatonin daily rhythmicity is associated with delirium development in hospitalized older adults. Sleep Sci. 2016; 9:285–288.
Article17. Chen S, Shi L, Liang F, Xu L, Desislava D, Wu Q, et al. Exogenous melatonin for delirium prevention: a meta-analysis of randomized controlled trials. Mol Neurobiol. 2016; 53:4046–4053.
Article18. Holcomb EM, Towns S, Kamper JE, Barnett SD, Sherer M, Evans C, et al. The relationship between sleep-wake cycle disturbance and trajectory of cognitive recovery during acute traumatic brain injury. J Head Trauma Rehabil. 2016; 31:108–116.
Article19. Duclos C, Dumont M, Arbour C, Paquet J, Blais H, Menon DK, et al. Parallel recovery of consciousness and sleep in acute traumatic brain injury. Neurology. 2017; 88:268–275.
Article