Ann Dermatol.
2019 Oct;31(5):571-575. 10.5021/ad.2019.31.5.571.
A Case of Subcutaneous and Intranasal Phaeohyphomycosis Caused by Microsphaeropsis arundinis in an Immunocompromised Patient Misdiagnosed with Mucormycosis
- Affiliations
-
- 1Department of Dermatology, School of Medicine, Chosun University, Gwangju, Korea. chna@chosun.ac.kr
- KMID: 2456237
- DOI: http://doi.org/10.5021/ad.2019.31.5.571
Abstract
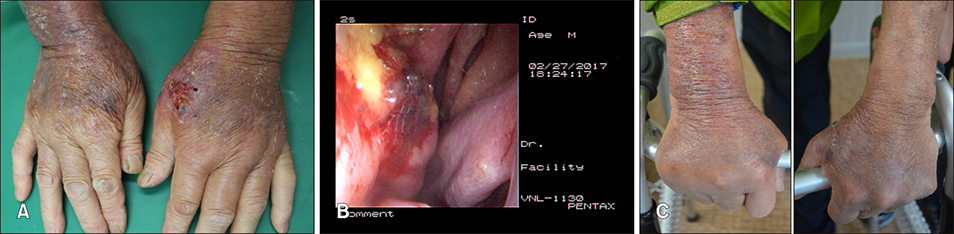
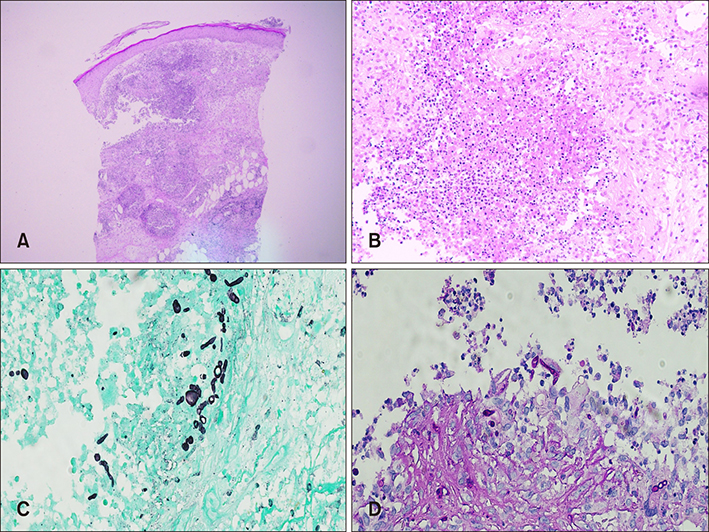
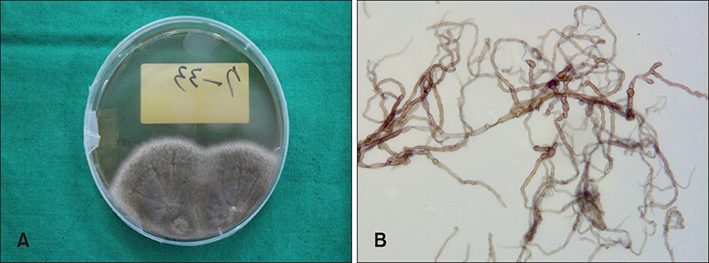
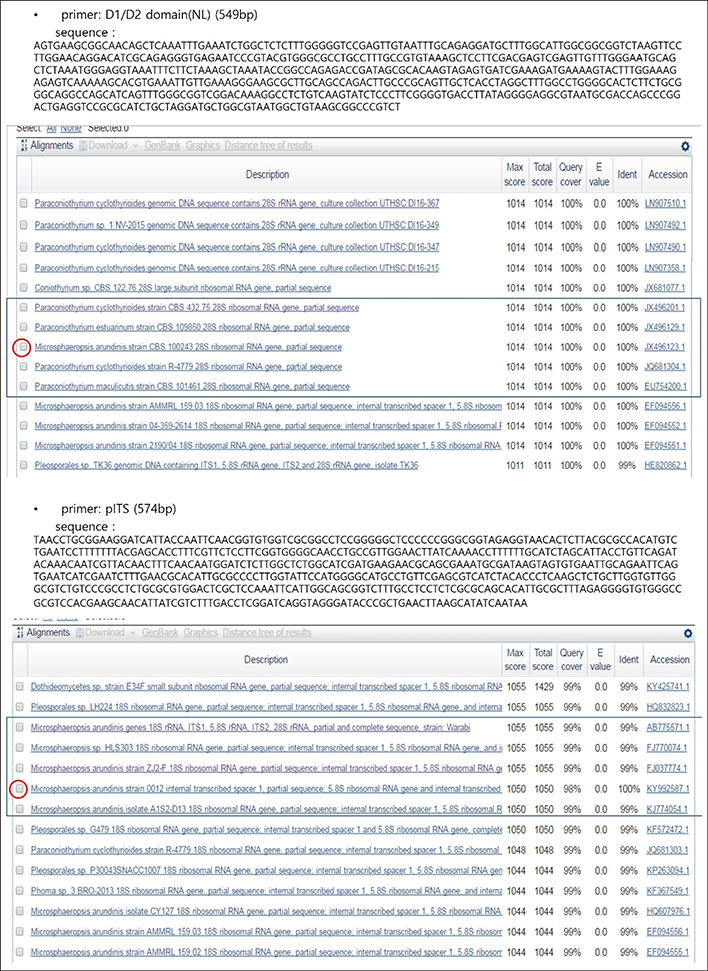
- Microsphaeropsis arundinis is a dematiaceous fungus capable of causing soft tissue infections known as phaeohyphomycosis, mostly in immunocompromised individuals. These infections arise from the traumatic inoculation of fungal materials into the subcutis, and can spread to adjacent subcutaneous tissues or via the lymphatics in a sporotrichoid manner. A 76-year-old man presented with diffuse erythematous plaques and swelling on both forearms and dorsal hands, and rhinalgia. He had been undergoing treatment for hypertension, angina pectoris, and diabetes. Histopathologic examinations of the skin, painful nasal septum, and molecular identification using internal transcribed spacer regions confirmed a diagnosis of subcutaneous and intranasal phaeohyphomycosis caused by M. arundinis. The patient was treated with oral itraconazole for over 5 months, and no recurrence was observed until the time of writing this manuscript. We report a rare case of subcutaneous and intranasal phaeohyphomycosis caused by M. arundinis and propose that confirmation of the causative strains is necessary, as it could affect the prognosis and treatment of the disease.
MeSH Terms
Figure
Reference
-
1. Pendle S, Weeks K, Priest M, Gill A, Hudson B, Kotsiou G, et al. Phaeohyphomycotic soft tissue infections caused by the coelomycetous fungus Microsphaeropsis arundinis. J Clin Microbiol. 2004; 42:5315–5319.
Article2. Asahina A, Kobayashi M, Nakano K, Saito I, Yarita K, Kamei K, et al. Deep cutaneous infection with Microsphaeropsis arundinis: report of two Japanese cases. Acta Derm Venereol. 2015; 95:855–857.
Article3. Hall MR, Brumble LM, Mayes MA, Snow JL, Keeling JH. Cutaneous Microsphaeropsis arundinis infection initially interpreted as squamous cell carcinoma. Int J Dermatol. 2013; 52:84–86.
Article4. Kim MN, Shin JH, Sung H, Lee K, Kim EC, Ryoo N, et al. Candida haemulonii and closely related species at 5 university hospitals in Korea: identification, antifungal susceptibility, and clinical features. Clin Infect Dis. 2009; 48:e57–e61.5. Crawford SJ, Chen SC, Halliday C, Rangan GK, Gottlieb T, Reid AB. Microsphaeropsis arundinis skin and soft tissue infection in renal transplant recipients: three case reports and a review of the literature. Transpl Infect Dis. 2015; 17:915–920.
Article6. Lee KC, Kim MJ, Chae SY, Lee HS, Jang YH, Lee SJ, et al. A case of phaeohyphomycosis caused by Exophiala lecaniicorni. Ann Dermatol. 2016; 28:385–387.
Article7. Ryu TH, Kwon IH, Choi JE, Ahn HH, Kye YC, Seo SH. A case of subcutaneous phaeohyphomycosis caused by Exophiala oligosperma showing multiple cysts. Korean J Dermatol. 2017; 55:259–263.8. Suh MK, Kwon SW, Kim TH, Sun YW, Lim JW, Ha GY, et al. A case of subcutaneous phaeohyphomycosis caused by Exophiala jeanselmei. Korean J Dermatol. 2005; 43:124–127.9. Ajello L, Georg LK, Steigbigel RT, Wang CJ. A case of phaeohyphomycosis caused by a new species of Phialophora. Mycologia. 1974; 66:490–498.
Article10. Sutton DA. Coelomycetous fungi in human disease. A review: clinical entities, pathogenesis, identification and therapy. Rev Iberoam Micol. 1999; 16:171–179.11. Stchigel AM, Sutton DA. Coelomycete fungi in the clinical lab. Curr Fungal Infect Rep. 2013; 7:171–191.
Article12. Chowdhary A, Meis JF, Guarro J, de Hoog GS, Kathuria S, Arendrup MC, et al. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of systemic phaeohyphomycosis: diseases caused by black fungi. Clin Microbiol Infect. 2014; 20 Suppl 3:47–75.
Article13. Ostrosky-Zeichner L, Alexander BD, Kett DH, Vazquez J, Pappas PG, Saeki F, et al. Multicenter clinical evaluation of the (1--〉3) beta-D-glucan assay as an aid to diagnosis of fungal infections in humans. Clin Infect Dis. 2005; 41:654–659.
Article14. Perusquía-Ortiz AM, Vázquez-González D, Bonifaz A. Opportunistic filamentous mycoses: aspergillosis, mucormycosis, phaeohyphomycosis and hyalohyphomycosis. J Dtsch Dermatol Ges. 2012; 10:611–621. quiz 621-622.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Subcutaneous Phaeohyphomycosis Caused by Exophiala oligosperma Showing Multiple Cysts
- Phaeohyphomycosis Due to Exophiala dermatitidis Successfully Treated with Itraconazole
- A Case of Rhinocerebral Mucormycosis Misdiagnosed as Herpes Zoster
- The First Case of Phaeohyphomycosis Caused by Exophiala xenobiotica in an Immunocompetent Patient in Korea
- A Case of Nasal Septal and Oral Cavity Abscesses Resulting from Mucormycosis in an Immunocompromised Patient