Korean J Radiol.
2019 Aug;20(8):1266-1274. 10.3348/kjr.2018.0742.
Prognostic Value of Radiologic Extranodal Extension in Human Papillomavirus-Related Oropharyngeal Squamous Cell Carcinoma
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jehee23@gmail.com
- 2Department of Radiology, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea.
- 3Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Otolaryngology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 5Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2453076
- DOI: http://doi.org/10.3348/kjr.2018.0742
Abstract
OBJECTIVE
To determine whether radiologic extranodal extension (ENE) appearing on pretreatment CT and MRI could predict the prognosis in patients with human papillomavirus (HPV)-related oropharyngeal squamous cell carcinoma (OPSCC).
MATERIALS AND METHODS
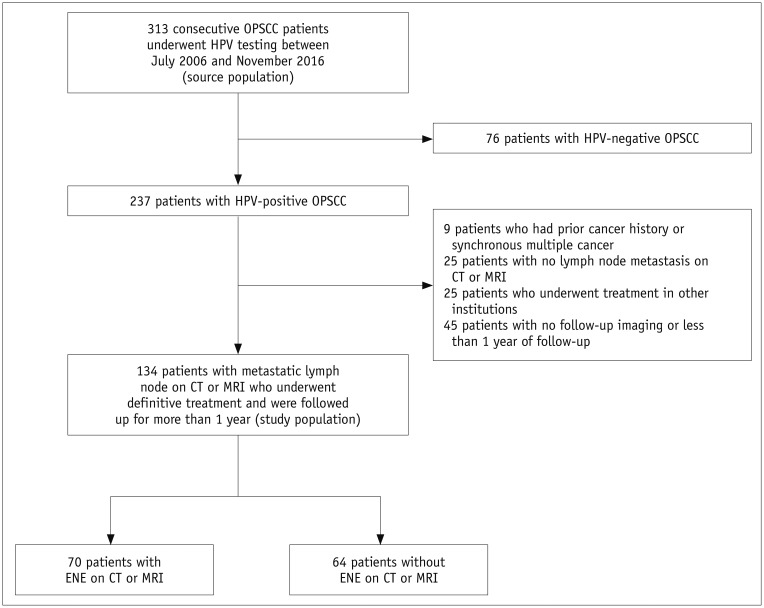
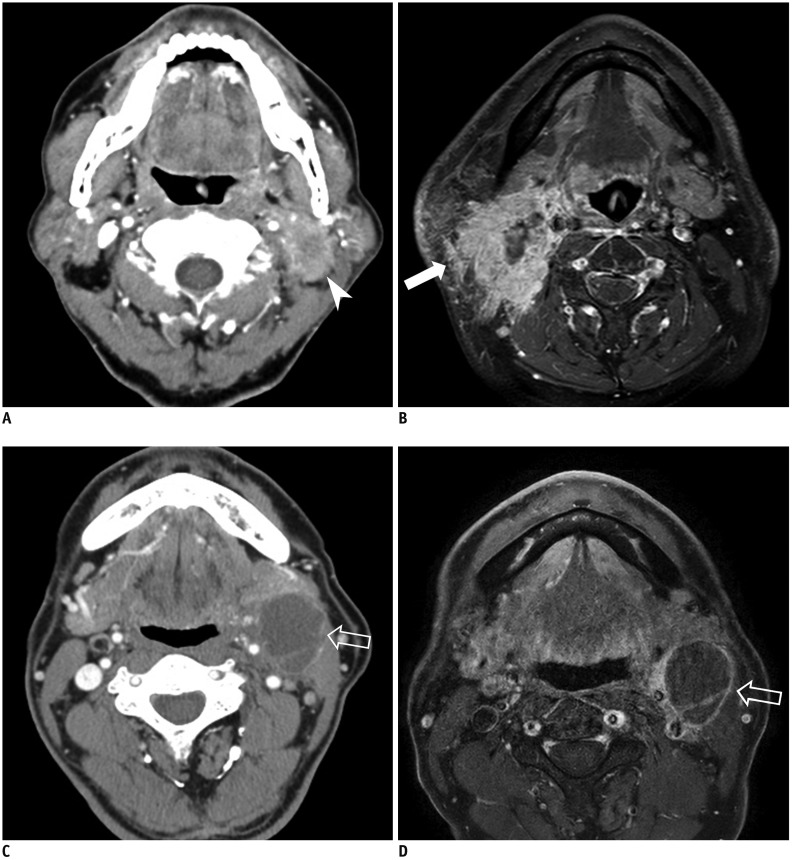
The study population was obtained from a historical cohort diagnosed with HPV-related OPSCC. A total of 134 OPSCC patients who had a metastatic lymph node on pretreatment CT or MRI were included, and radiologic ENE was evaluated by two experienced head and neck radiologists. Kaplan-Meier and multivariate Cox regression analyses were performed to evaluate the impact of radiologic ENE on progression-free survival (PFS). The diagnostic performance of CT and MRI for the diagnosis of ENE was also evaluated in patients who underwent neck dissection.
RESULTS
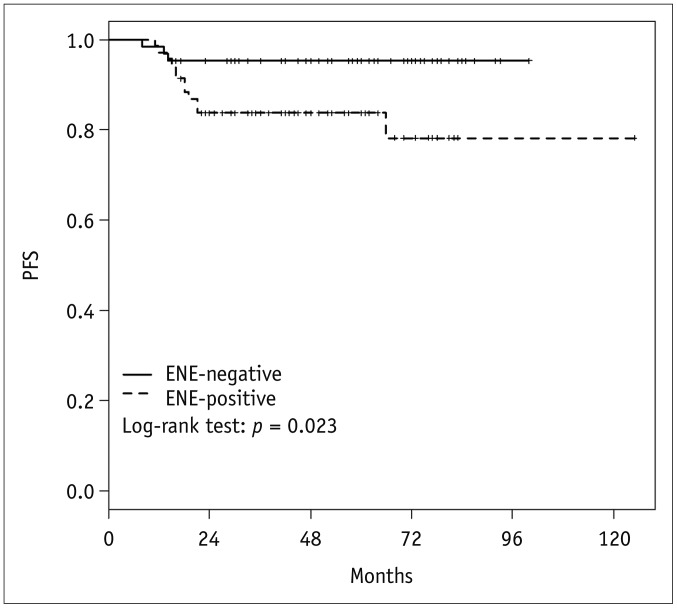
Seventy patients (52.2%) showed radiologic ENE-positive findings. Although patients showing radiologic ENE had a worse 3-year PFS (83.7% vs. 95.3%, p = 0.023), the association between radiologic ENE and PFS was not statistically significant on multivariate analysis (p = 0.141; hazard ratio, 2.68; 95% confidence interval, 0.72-9.97). CT or MRI had a sensitivity of 62%, specificity of 77.8%, and accuracy of 71.9% for predicting pathologic ENE.
CONCLUSION
Radiologic ENE on CT or MRI did not predict poor PFS in patients with HPV-related OPSCC, although there was a trend towards worse PFS. Further studies are warranted to determine whether radiologic ENE is a useful imaging biomarker to risk-stratify patients with HPV-related OPSCC.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Radiotherapy versus Surgery in Early-Stage HPV-Positive Oropharyngeal Cancer
Dong-Yun Kim, Hong-Gyun Wu, Jin Ho Kim, Joo Ho Lee, Soon-Hyun Ahn, Eun-Jae Chung, Keun-Yong Eom, Young Ho Jung, Woo-Jin Jeong, Tack-Kyun Kwon, Suzy Kim, Chan Woo Wee
Cancer Res Treat. 2022;54(2):406-416. doi: 10.4143/crt.2021.441.
Reference
-
1. Gillison ML, Chaturvedi AK, Anderson WF, Fakhry C. Epidemiology of human papillomavirus-positive head and neck squamous cell carcinoma. J Clin Oncol. 2015; 33:3235–3242. PMID: 26351338.
Article2. Pytynia KB, Dahlstrom KR, Sturgis EM. Epidemiology of HPV-associated oropharyngeal cancer. Oral Oncol. 2014; 50:380–386. PMID: 24461628.
Article3. Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. 8th ed. New York, NY: springer;2017.4. Haughey BH, Sinha P. Prognostic factors and survival unique to surgically treated p16+ oropharyngeal cancer. Laryngoscope. 2012; 122(Suppl 2):S13–S33. PMID: 22926949.
Article5. Lydiatt WM, Patel SG, O'Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, et al. Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017; 67:122–137. PMID: 28128848.
Article6. Wreesmann VB, Katabi N, Palmer FL, Montero PH, Migliacci JC, Gönen M, et al. Influence of extracapsular nodal spread extent on prognosis of oral squamous cell carcinoma. Head Neck. 2016; 38(Suppl 1):E1192–E1199. PMID: 26514096.
Article7. Sinha P, Lewis JS Jr, Piccirillo JF, Kallogjeri D, Haughey BH. Extracapsular spread and adjuvant therapy in human papillomavirus-related, p16-positive oropharyngeal carcinoma. Cancer. 2012; 118:3519–3530. PMID: 22086669.
Article8. Myers JN, Greenberg JS, Mo V, Roberts D. Extracapsular spread. A significant predictor of treatment failure in patients with squamous cell carcinoma of the tongue. Cancer. 2001; 92:3030–3036. PMID: 11753980.9. Prabhu RS, Magliocca KR, Hanasoge S, Aiken AH, Hudgins PA, Hall WA, et al. Accuracy of computed tomography for predicting pathologic nodal extracapsular extension in patients with head-and-neck cancer undergoing initial surgical resection. Int J Radiat Oncol Biol Phys. 2014; 88:122–129. PMID: 24331658.
Article10. Ragin CC, Taioli E. Survival of squamous cell carcinoma of the head and neck in relation to human papillomavirus infection: review and meta-analysis. Int J Cancer. 2007; 121:1813–1820. PMID: 17546592.
Article11. Kaka AS, Kumar B, Kumar P, Wakely PE Jr, Kirsch CM, Old MO, et al. Highly aggressive human papillomavirus-related oropharyngeal cancer: clinical, radiologic, and pathologic characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:327–335. PMID: 23770280.
Article12. Spector ME, Gallagher KK, Light E, Ibrahim M, Chanowski EJ, Moyer JS, et al. University of Michigan Head Neck Specialized Program of Research Excellence (SPORE) Program. Matted nodes: poor prognostic marker in oropharyngeal squamous cell carcinoma independent of HPV and EGFR status. Head Neck. 2012; 34:1727–1733. PMID: 22247002.
Article13. Huang SH, Perez-Ordonez B, Liu FF, Waldron J, Ringash J, Irish J, et al. Atypical clinical behavior of p16-confirmed HPV-related oropharyngeal squamous cell carcinoma treated with radical radiotherapy. Int J Radiat Oncol Biol Phys. 2012; 82:276–283. PMID: 20950953.
Article14. Rath TJ, Narayanan S, Hughes MA, Ferris RL, Chiosea SI, Branstetter BF 4th. Solid lymph nodes as an imaging biomarker for risk stratification in human papillomavirus-related oropharyngeal squamous cell carcinoma. AJNR Am J Neuroradiol. 2017; 38:1405–1410. PMID: 28450437.
Article15. Liu JT, Kann BH, De B, Buckstein M, Bakst RL, Genden EM, et al. Prognostic value of radiographic extracapsular extension in locally advanced head and neck squamous cell cancers. Oral Oncol. 2016; 52:52–57. PMID: 26728104.
Article16. Lee KC, Moon WK, Chung JW, Choi SH, Cho N, Cha JH, et al. Assessment of lymph node metastases by contrast-enhanced MR imaging in a head and neck cancer model. Korean J Radiol. 2007; 8:9–14. PMID: 17277558.
Article17. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. STROBE Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007; 4:e297. PMID: 17941715.18. Lee S, Lee SW, Park S, Yoon SM, Park JH, Song SY, et al. Refining prognostic stratification of human papilloma-virusrelated oropharyngeal squamous cell carcinoma: different prognosis between T1 and T2. Radiat Oncol J. 2017; 35:233–240. PMID: 29037027.
Article19. Sargent DJ, Wieand HS, Haller DG, Gray R, Benedetti JK, Buyse M, et al. Disease-free survival versus overall survival as a primary end point for adjuvant colon cancer studies: individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol. 2005; 23:8664–8670. PMID: 16260700.
Article20. Chai RL, Rath TJ, Johnson JT, Ferris RL, Kubicek GJ, Duvvuri U, et al. Accuracy of computed tomography in the prediction of extracapsular spread of lymph node metastases in squamous cell carcinoma of the head and neck. JAMA Otolaryngol Head Neck Surg. 2013; 139:1187–1194. PMID: 24076619.
Article21. Souter MA, Allison RS, Clarkson JH, Cowan IA, Coates MH, Wells JE. Sensitivity and specificity of computed tomography for detection of extranodal spread from metastatic head and neck squamous cell carcinoma. J Laryngol Otol. 2009; 123:778–782. PMID: 19134244.
Article22. Som PM, Brandwein-Gensler MS. Lymph nodes of the neck. In : Som PM, Curtin HD, editors. Head and neck imaging. 5th ed. St. Louis, MO: Mosby;2011. p. 2287–2384.23. Patel MR, Hudgins PA, Beitler JJ, Magliocca KR, Griffith CC, Liu Y, et al. Radiographic imaging does not reliably predict macroscopic extranodal extension in human papilloma virus-associated oropharyngeal cancer. ORL J Otorhinolaryngol Relat Spec. 2018; 80:85–95. PMID: 29969771.
Article24. Huang YH, Yeh CH, Cheng NM, Lin CY, Wang HM, Ko SF, et al. Cystic nodal metastasis in patients with oropharyngeal squamous cell carcinoma receiving chemoradiotherapy: relationship with human papillomavirus status and failure patterns. PLoS One. 2017; 12:e0180779. PMID: 28686646.
Article25. Kundel HL, Polansky M. Measurement of observer agreement. Radiology. 2003; 228:303–308. PMID: 12819342.
Article26. Kim S, Lee JW, Chai JW, Yoo HJ, Kang Y, Seo J, et al. A new MRI grading system for cervical foraminal stenosis based on axial T2-weighted images. Korean J Radiol. 2015; 16:1294–1302. PMID: 26576119.
Article27. Park JE, Han K, Sung YS, Chung MS, Koo HJ, Yoon HM, et al. Selection and reporting of statistical methods to assess reliability of a diagnostic test: conformity to recommended methods in a peer-reviewed journal. Korean J Radiol. 2017; 18:888–897. PMID: 29089821.
Article28. Geltzeiler M, Clayburgh D, Gleysteen J, Gross ND, Hamilton B, Andersen P, et al. Predictors of extracapsular extension in HPV-associated oropharyngeal cancer treated surgically. Oral Oncol. 2017; 65:89–93. PMID: 28109475.
Article29. Mermod M, Tolstonog G, Simon C, Monnier Y. Extracapsular spread in head and neck squamous cell carcinoma: a systematic review and meta-analysis. Oral Oncol. 2016; 62:60–71. PMID: 27865373.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Synchronous Verrucous Carcinoma and Squamous Cell Carcinoma of Penis by Different Human Papillomavirus Infections
- Warty Squamous Cell Carcinoma of the Vulva in Older Women: Association with Human Papillomavirus
- Investigating Trk Protein Expression between Oropharyngeal and Non-oropharyngeal Squamous Cell Carcinoma: Clinical Implications and Possible Roles of Human Papillomavirus Infection
- Pediatric vulvar squamous cell carcinoma in a liver transplantation recipient: a case report
- Squamous Cell Carcinoma of the Cervix with Intraepithelial Extension to the Endometrium: A Case Report