Perinatology.
2019 Jun;30(2):83-92. 10.14734/PN.2019.30.2.83.
Feasibility and Functional Evaluation of Noninvasive Ventilation Capable Equipment from the Delivery Room to Neonatal Intensive Care Unit: A Bench Study
- Affiliations
-
- 1Department of Pediatrics, Gachon University College of Medicine, Incheon, Korea. sondw@gilhospital.com
- 2Department of Obstetrics and Gynecology, Gachon University College of Medicine, Incheon, Korea.
- KMID: 2453043
- DOI: http://doi.org/10.14734/PN.2019.30.2.83
Abstract
OBJECTIVE
The use of noninvasive ventilation (NIV) for newborns requiring respiratory support in delivery room (DR) is recommended. However, the details related to such use are not well established. A bench investigation on the performance of available NIV equipment was conducted.
METHODS
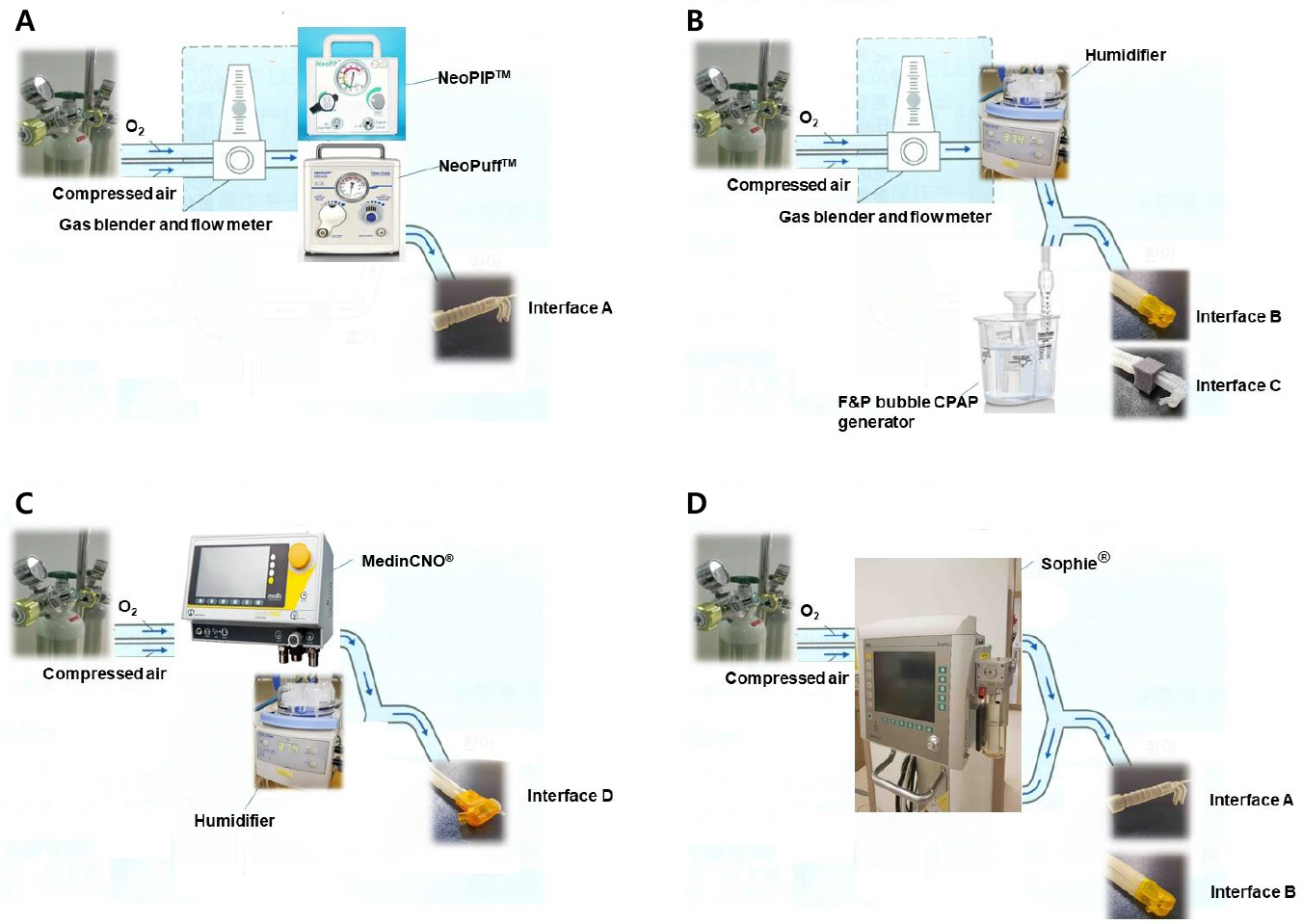
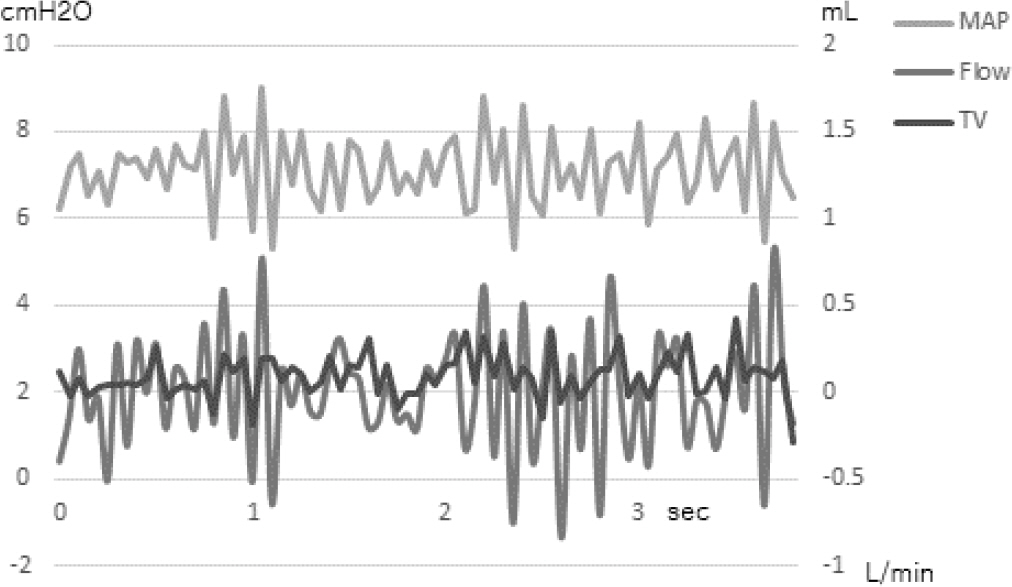
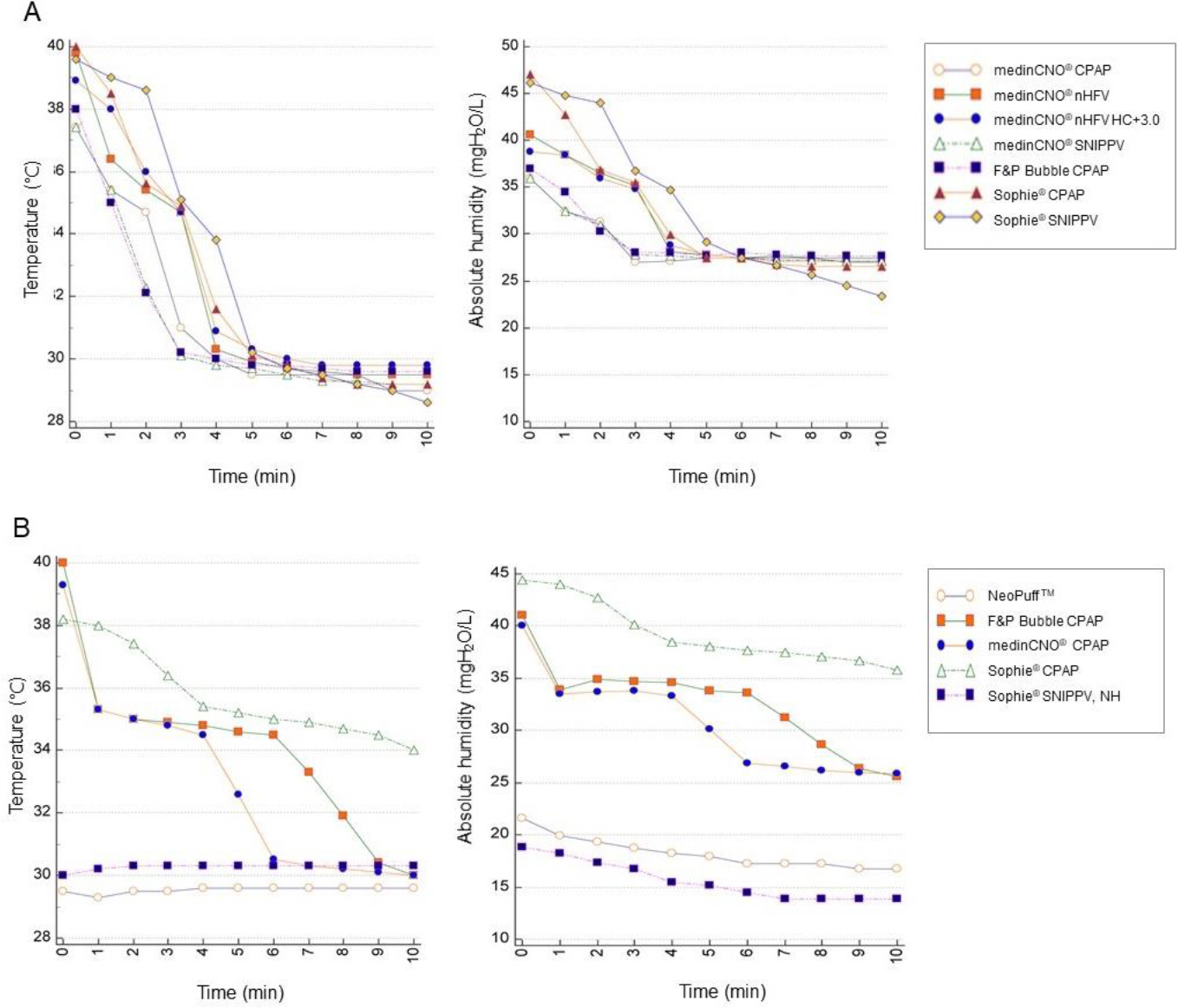
Two T-piece resuscitators (TPRs) and three ventilators were tested with a Neonatal Lung Simulator which is capable of recording the pressure, flow, and volume. We measured the pressurization and delivered volume (DV) of nasal continuous positive airway pressure (nCPAP), bubble CPAP (bCPAP)/nasal high-frequency ventilation (nHFV), and synchronized nasal intermittent positive pressure ventilation (SNIPPV) in apneic and breathing models. Temperature and absolute humidity (AH) at the Y-piece were checked for 10 minutes in each setting while the Y-piece on an open bassinet or in a preheated incubator.
RESULTS
The pressurization was well achieved with every combination except for TPRs on nCPAP. DV was well provided using bCPAP/nHFV and SNIPPV in the breathing model. With bCPAP, DV decreased significantly in apneic model. On the bassinet, temperature and AH dropped to ambient temperature and approximately 25 mgH₂O/L within 4 minutes, respectively. In the incubator, temperature and AH on all pre-humidified machines were maintained above 34℃ and 30 mgH₂O/L for 5 minutes, respectively. Those without pre-humidification were below 30℃ and less than 20 mgH₂O/L, respectively.
CONCLUSION
Other combination of device/equipment than TPR tested seemed more feasible for nCPAP. The use of equipment with backup ventilation and heated-humidified gas in preheated incubators would be more appropriate NIV for premature infants in DR and during transport.
MeSH Terms
-
Continuous Positive Airway Pressure
Delivery Rooms*
Equipment Design
High-Frequency Ventilation
Humans
Humidity
Incubators
Infant, Newborn
Infant, Premature
Intensive Care, Neonatal*
Intermittent Positive-Pressure Ventilation
Lung
Noninvasive Ventilation*
Respiration
Transportation
Ventilation
Ventilators, Mechanical
Figure
Reference
-
References
1. Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010; 362:1970–9.
Article2. Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. Part 13: neonatal resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(18 Suppl 2):S543–60.3. Diblasi RM. Nasal continuous positive airway pressure (CPAP) for the respiratory care of the newborn infant. Respir Care. 2009; 54:1209–35.4. Avery ME, Tooley WH, Keller JB, Hurd SS, Bryan MH, Cotton RB, et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987; 79:26–30.
Article5. Subramaniam P, Ho JJ, Davis PG. Prophylactic nasal continuous positive airway pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2016; 6:CD001243.
Article6. Lemyre B, Laughon M, Bose C, Davis PG. Early nasal intermittent positive pressure ventilation (NIPPV) versus early nasal continuous positive airway pressure (NCPAP) for preterm infants. Cochrane Database Syst Rev. 2016; 12:CD005384.
Article7. Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB, et al. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008; 358:700–8.
Article8. Shim GH. Update of minimally invasive surfactant therapy. Korean J Pediatr. 2017; 60:273–81.
Article9. Rigo V, Lefebvre C, Broux I. Surfactant instillation in spontaneously breathing preterm infants: a systematic review and meta-analysis. Eur J Pediatr. 2016; 175:1933–42.
Article10. Aldana-Aguirre JC, Pinto M, Featherstone RM, Kumar M. Less invasive surfactant administration versus intubation for surfactant delivery in preterm infants with respiratory distress syndrome: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2017; 102:F17–23.
Article11. Isayama T, Iwami H, McDonald S, Beyene J. Association of noninvasive ventilation strategies with mortality and bronchopulmonary dysplasia among preterm infants: a systematic review and meta-analysis. JAMA. 2016; 316:611–24.12. Yeo CL, Biswas A, Ee TT, Chinnadurai A, Baral VR, Chang AS, et al. Singapore neonatal resuscitation guidelines 2016. Singapore Med J. 2017; 58:391–403.
Article13. Perlman JM, Wyllie J, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R, et al. Part 7: neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015; 132(16 Suppl 1):S204–41.14. Doctor TN, Foster JP, Tan K, Todd DA, McGrory L, Stewart A. Heated and humidified inspired gas through heated humidifiers in comparison to non‐heated and non‐humidified gas in hospitalised neonates receiving respiratory support. Cochrane Database Syst Rev. 2017; 2:CD012549.
Article15. Schulze A. Respiratory gas conditioning and humidification. Clin Perinatol. 2007; 34:19–33. v.
Article16. Greenspan JS, Wolfson MR, Shaffer TH. Airway responsiveness to low inspired gas temperature in preterm neonates. J Pediatr. 1991; 118:443–5.
Article17. Tarnow-Mordi WO, Reid E, Griffiths P, Wilkinson AR. Low inspired gas temperature and respiratory complications in very low birth weight infants. J Pediatr. 1989; 114:438–42.
Article18. Shearman AD, Hou D, Dunster KR, Jardine L. Heating of gases during neonatal resuscitation: a bench study. Resuscitation. 2012; 83:369–73.
Article19. Farley RC, Gibbons K, Jardine LA, Shearman AD. Effect of flow rate, humidifier dome and water volume on maximising heated, humidified gas use for neonatal resuscitation. Resuscitation. 2013; 84:1428–32.
Article20. McFadden ER Jr. Heat and water exchange in human airways. Am Rev Respir Dis. 1992; 146(5 Pt 2):S8–10.
Article21. Ullrich TL, Czernik C, Buhrer C, Schmalisch G, Fischer HS. Nasal high-frequency oscillatory ventilation impairs heated humidification: a neonatal bench study. Pediatr Pulmonol. 2017; 52:1455–60.
Article22. Bailes SA, Firestone KS, Dunn DK, McNinch NL, Brown MF, Volsko TA. Evaluating the effect of flow and interface type on pressures delivered with bubble CPAP in a simulated model. Respir Care. 2016; 61:333–9.
Article23. Sivieri EM, Gerdes JS, Abbasi S. Effect of HFNC flow rate, cannula size, and nares diameter on generated airway pressures: an in vitro study. Pediatr Pulmonol. 2013; 48:506–14.
Article24. Ahluwalia JS, Morley CJ, Mockridge JN. Computerised determination of spontaneous inspiratory and expiratory times in premature neonates during intermittent positive pressure ventilation. II: results from 20 babies. Arch Dis Child Fetal Neonatal Ed. 1994; 71:F161–4.
Article25. Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, et al. European consensus guidelines on the management o frespiratory distress syndrome – 2016 update. Neonatology. 2017; 111:107–25.26. de Almeida MFB, Guinsburg R, Sancho GA, Rosa IRM, Lamy ZC, Martinez FE, et al. Hypothermia and early neonatal mortality in preterm infants. J Pediatr. 2014; 164:271–5. e1.
Article27. te Pas AB, Lopriore E, Dito I, Morley CJ, Walther FJ. Humidified and heated air during stabilization at birth improves temperature in preterm infants. Pediatrics. 2010; 125:e1427–32.
Article28. Williams R, Rankin N, Smith T, Galler D, Seakins P. Relationship between the humidity and temperature of inspired gas and the function of the airway mucosa. Crit Care Med. 1996; 24:1920–9.
Article29. Dawson JA, Owen LS, Middleburgh R, Davis PG. Quantifying temperature and relative humidity of medical gases used for newborn resuscitation. J Paediatr Child Health. 2014; 50:24–6.
Article30. Yamada Y, Kyuno T, Suzuki S, Ito T, Kato I, Togari H. A drop in gas temperature in the external part of the endotracheal tube is problematic during neonatal respiratory support. Pediatr Pulmonol. 2008; 43:666–73.
Article31. Nagaya K, Tsuchida E, Nohara F, Okamoto T, Azuma H. The temperature change in an endotracheal tube during high frequency ventilation using an artificial neonatal lung model with Babylog® 8000 plus. Pediatr Pulmonol. 2015; 50:173–8.32. Schaller Medizintechnik. Gina – neonatal active lung model [online]. 2016. [cited 2018 Dec 28]. Available from: URL:. https://schaller-mt.de/download/LM_En.pdf.33. Lee SH, Chae MH, Cho HJ, Ryoo E, Shim SY, Son DW. Using the high frequency ventilation during neonatal transport. J Korean Soc Neonatol. 2012; 19:221–8.
Article34. Pillow JJ, Hillman N, Moss TJ, Polglase G, Bold G, Beaumont C, et al. Bubble continuous positive airway pressure enhances lung volume and gas exchange in preterm lambs. Am J Respir Crit Care Med. 2007; 176:63–9.
Article35. Lee KS, Dunn MS, Fenwick M, Shennan AT. A comparison of underwater bubble continuous positive airway pressure with ventilator-derived continuous positive airway pressure in premature neonates ready for extubation. Biol Neonate. 1998; 73:69–75.
Article36. Poli JA, Peter Richardson CP, DiBlasi RM. Volume oscillations delivered to a lung model using 4 different bubble CPAP systems. Respir Care. 2015; 60:371–81.
Article37. Fisher & Paykel Healthcare. Bubble CPAP system setup guide [online]. 2011. [cited 2019 Jan 6]. Available from: URL:. https://resources.fphcare.com/resources/corporate/media/resources/resources/pm-185034215-a.pdf.38. Liptsen E, Aghai ZH, Pyon KH, Saslow JG, Nakhla T, Long J, et al. Work of breathing during nasal continuous positive airway pressure in preterm infants: a comparison of bubble vs variable-flow devices. J Perinatol. 2005; 25:453–8.
Article39. Schmölzer GM, Morley CJ, Wong C, Dawson JA, Kamlin CO, Donath SM, et al. Respiratory function monitor guidance of mask ventilation in the delivery room: a feasibility study. J Pediatr. 2012; 160:377–81. e2.
Article40. Oto J, Imanaka H, Nishimura M. Clinical factors affecting inspired gas humidification and oral dryness during noninvasive ventilation. J Crit Care. 2011; 26:535. e9–535.e15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Organisation of Special and Intensive Care Facilities for Babies
- Functional Analysis of Neonatal Intensive Care Centers and Effective Operation Plan
- New Modalities and Modes in Neonatal Ventilation Therapy
- Lng Injury Induced during Resuscitation of the Preterm Newborns in the Delivery Room
- Current status of neonatal intensive care units in Korea