J Clin Neurol.
2019 Jul;15(3):353-359. 10.3988/jcn.2019.15.3.353.
Cerebrospinal Fluid Levels of β-Amyloid 40 and β-Amyloid 42 are Proportionately Decreased in Amyloid Positron-Emission Tomography Negative Idiopathic Normal-Pressure Hydrocephalus Patients
- Affiliations
-
- 1Department of Neurology, Ajou University School of Medicine, Suwon, Korea. symoon.bv@gmail.com
- 2Department of Brain Science, Ajou University School of Medicine, Suwon, Korea. jaerakchang@ajou.ac.kr
- 3Department of Biomedical Sciences, Ajou University School of Medicine, Suwon, Korea.
- 4Department of Nuclear Medicine and Molecular Imaging, Ajou University School of Medicine, Suwon, Korea.
- 5Department of Neurology, Chung-Ang University College of Medicine, Seoul, Korea.
- 6Department of Anatomy, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2451120
- DOI: http://doi.org/10.3988/jcn.2019.15.3.353
Abstract
- BACKGROUND AND PURPOSE
Cerebrospinal fluid (CSF) biomarkers of Alzheimer's disease (AD) could be misleading in idiopathic normal-pressure hydrocephalus (iNPH). We therefore investigated the CSF biomarkers in 18F-florbetaben amyloid-negative positron-emission tomography (PET) [amyloid PET(−)] iNPH, amyloid-positive PET [amyloid PET(+)] AD, and cognitively normal (CN) subjects.
METHODS
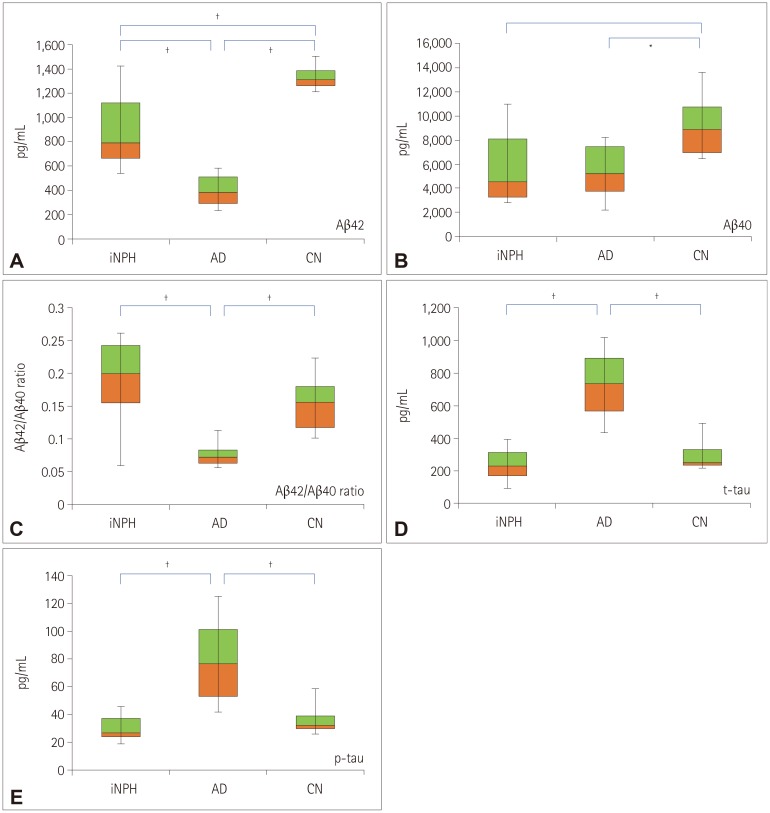
Ten amyloid PET(+) AD patients (56.7±5.6 years old, mean±standard deviation), 10 amyloid PET(−) iNPH patients (72.8±4.5 years old), and 8 CN subjects (61.2±6.5 years old) were included. We measured the levels of β-amyloid (Aβ)40, Aβ42, total tau (t-tau) protein, and phosphorylated tau (p-tau) protein in the CSF using enzyme-linked immunosorbent assays.
RESULTS
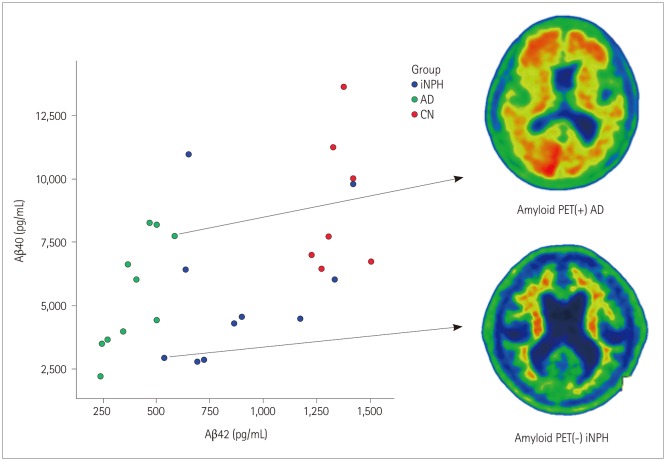
The level of Aβ42 and the Aβ42/Aβ40 ratio in the CSF were significantly lower in AD than in iNPH or CN subjects. The Aβ40 level did not differ significantly between AD and iNPH (p=1.000), but it did between AD and CN subjects (p=0.032). The levels of both t-tau and p-tau were higher in AD than in iNPH or CN subjects. The levels of Aβ42, Aβ40, t-tau, and p-tau were lower in iNPH than in CN subjects, but there was no significant difference after controlling for age.
CONCLUSIONS
Our results suggest that the mechanism underlying low CSF Aβ levels differs between amyloid PET(−) iNPH and amyloid PET(+) AD subjects. The lower levels of all CSF biomarkers in iNPH patients might be due to reduced clearances from extracellular fluid and decreased brain metabolism of the periventricular zone in iNPH resulting from glymphatic dysfunction.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Cerebrospinal Fluid Biomarkers for the Diagnosis and Classification of Alzheimer's Disease Spectrum
Jongmin Lee, Hyemin Jang, Sung Hoon Kang, Jaeho Kim, Ji Sun Kim, Jun Pyo Kim, Hee Jin Kim, Sang Won Seo, Duk L. Na
J Korean Med Sci. 2020;35(44):e361. doi: 10.3346/jkms.2020.35.e361.Cerebrospinal Fluid Biomarkers for the Diagnosis and Classification of Alzheimer's Disease Spectrum
Jongmin Lee, Hyemin Jang, Sung Hoon Kang, Jaeho Kim, Ji Sun Kim, Jun Pyo Kim, Hee Jin Kim, Sang Won Seo, Duk L. Na
J Korean Med Sci. 2020;35(44):e361. doi: 10.3346/jkms.2020.35.e361.
Reference
-
1. Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH. Symptomatic occult hydrocephalus with “normal” cerebrospinal-fluid pressure. A treatable syndrome. N Engl J Med. 1965; 273:117–126. PMID: 14303656.2. Leinonen V, Koivisto AM, Savolainen S, Rummukainen J, Tamminen JN, Tillgren T, et al. Amyloid and tau proteins in cortical brain biopsy and Alzheimer's disease. Ann Neurol. 2010; 68:446–453. PMID: 20976765.
Article3. Golomb J, Wisoff J, Miller DC, Boksay I, Kluger A, Weiner H, et al. Alzheimer's disease comorbidity in normal pressure hydrocephalus: prevalence and shunt response. J Neurol Neurosurg Psychiatry. 2000; 68:778–781. PMID: 10811706.
Article4. Blennow K, Hampel H. CSF markers for incipient Alzheimer's disease. Lancet Neurol. 2003; 2:605–613. PMID: 14505582.
Article5. Lim TS, Choi JY, Park SA, Youn YC, Lee HY, Kim BG, et al. Evaluation of coexistence of Alzheimer's disease in idiopathic normal pressure hydrocephalus using ELISA analyses for CSF biomarkers. BMC Neurol. 2014; 14:66. PMID: 24690253.
Article6. Jeppsson A, Zetterberg H, Blennow K, Wikkelsø C. Idiopathic normal-pressure hydrocephalus: pathophysiology and diagnosis by CSF biomarkers. Neurology. 2013; 80:1385–1392. PMID: 23486875.7. Kapaki EN, Paraskevas GP, Tzerakis NG, Sfagos C, Seretis A, Kararizou E, et al. Cerebrospinal fluid tau, phospho-tau181 and β-amyloid1-42 in idiopathic normal pressure hydrocephalus: a discrimination from Alzheimer's disease. Eur J Neurol. 2007; 14:168–173. PMID: 17250725.8. Jingami N, Asada-Utsugi M, Uemura K, Noto R, Takahashi M, Ozaki A, et al. Idiopathic normal pressure hydrocephalus has a different cerebrospinal fluid biomarker profile from Alzheimer's disease. J Alzheimers Dis. 2015; 45:109–115. PMID: 25428256.
Article9. Graff-Radford NR. Alzheimer CSF biomarkers may be misleading in normal-pressure hydrocephalus. Neurology. 2014; 83:1573–1575. PMID: 25332445.
Article10. Chen Z, Liu C, Zhang J, Relkin N, Xing Y, Li Y. Cerebrospinal fluid Aβ42, t-tau, and p-tau levels in the differential diagnosis of idiopathic normal-pressure hydrocephalus: a systematic review and meta-analysis. Fluids Barriers CNS. 2017; 14:13. PMID: 28486988.
Article11. Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005; 57:S4–S16. PMID: 16160425.
Article12. Larsson A, Wikkelsö C, Bilting M, Stephensen H. Clinical parameters in 74 consecutive patients shunt operated for normal pressure hydrocephalus. Acta Neurol Scand. 1991; 84:475–482. PMID: 1792852.
Article13. Krauss JK, Regel JP, Vach W, Jüngling FD, Droste DW, Wakhloo AK. Flow void of cerebrospinal fluid in idiopathic normal pressure hydrocephalus of the elderly: can it predict outcome after shunting. Neurosurgery. 1997; 40:67–73. PMID: 8971826.
Article14. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984; 34:939–944. PMID: 6610841.
Article15. Moon SY, Na DL, Seo SW, Lee JY, Ku BD, Kim SY, et al. Impact of white matter changes on activities of daily living in mild to moderate dementia. Eur Neurol. 2011; 65:223–230. PMID: 21447954.
Article16. Ahn HJ, Chin J, Park A, Lee BH, Suh MK, Seo SW, et al. Seoul Neuropsychological Screening Battery-dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J Korean Med Sci. 2010; 25:1071–1076. PMID: 20592901.
Article17. Sabri O, Seibyl J, Rowe C, Barthel H. Beta-amyloid imaging with florbetaben. Clin Transl Imaging. 2015; 3:13–26. PMID: 25741488.
Article18. Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage. 2002; 15:273–289. PMID: 11771995.
Article19. Choi WH, Um YH, Jung WS, Kim SH. Automated quantification of amyloid positron emission tomography: a comparison of PMOD and MIMneuro. Ann Nucl Med. 2016; 30:682–689. PMID: 27567617.
Article20. Santangelo R, Cecchetti G, Bernasconi MP, Cardamone R, Barbieri A, Pinto P, et al. Cerebrospinal fluid amyloid-β 42, total tau and phosphorylated tau are low in patients with normal pressure hydrocephalus: analogies and differences with Alzheimer's disease. J Alzheimers Dis. 2017; 60:183–200. PMID: 28826180.
Article21. Lewczuk P, Matzen A, Blennow K, Parnetti L, Molinuevo JL, Eusebi P, et al. Cerebrospinal fluid Aβ42/40 corresponds better than Aβ42 to amyloid PET in Alzheimer's disease. J Alzheimers Dis. 2017; 55:813–822. PMID: 27792012.22. Palmqvist S, Mattsson N, Hansson O. Alzheimer's Disease Neuroimaging Initiative. Cerebrospinal fluid analysis detects cerebral amyloid-β accumulation earlier than positron emission tomography. Brain. 2016; 139:1226–1236. PMID: 26936941.
Article23. Toledo JB, Bjerke M, Da X, Landau SM, Foster NL, Jagust W, et al. Nonlinear association between cerebrospinal fluid and florbetapir F-18 β-amyloid measures across the spectrum of Alzheimer disease. JAMA Neurol. 2015; 72:571–581. PMID: 25822737.
Article24. Sutphen CL, Jasielec MS, Shah AR, Macy EM, Xiong C, Vlassenko AG, et al. Longitudinal cerebrospinal fluid biomarker changes in preclinical Alzheimer disease during middle age. JAMA Neurol. 2015; 72:1029–1042. PMID: 26147946.
Article25. Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013; 342:373–377. PMID: 24136970.
Article26. Ju YS, Ooms SJ, Sutphen C, Macauley SL, Zangrilli MA, Jerome G, et al. Slow wave sleep disruption increases cerebrospinal fluid amyloid-β levels. Brain. 2017; 140:2104–2111. PMID: 28899014.
Article27. Paternicò D, Galluzzi S, Drago V, Bocchio-Chiavetto L, Zanardini R, Pedrini L, et al. Cerebrospinal fluid markers for Alzheimer's disease in a cognitively healthy cohort of young and old adults. Alzheimers Dement. 2012; 8:520–527. PMID: 22677492.
Article28. Sjögren M, Vanderstichele H, Agren H, Zachrisson O, Edsbagge M, Wikkelsø C, et al. Tau and Aβ42 in cerebrospinal fluid from healthy adults 21-93 years of age: establishment of reference values. Clin Chem. 2001; 47:1776–1781. PMID: 11568086.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patterns of Cerebrospinal Fluid Biomarkers and Amyloid Positron Emission Tomography in a Patient with Cerebral Amyloid Angiopathy-Related Inflammation
- Hydrocephalus in a Patient with Alzheimer's Disease
- Longitudinal Observation of Early-Onset Alzheimer’s Disease Dementia with Positive CSF Biomarkers/Negative Amyloid-β Positron-Emission Tomography
- Association between Cerebral Amyloid Deposition and Clinical Factors Including Cognitive Function in Geriatric Depression: Pilot Study Using Amyloid Positron Emission Tomography
- Cerebral Amyloid Angiopathy: Emerging Concepts