J Adv Prosthodont.
2019 Jun;11(3):147-154. 10.4047/jap.2019.11.3.147.
Influence of implant-abutment connection structure on peri-implant bone level in a second molar: A 1-year randomized controlled trial
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry and Dental Research Institute, Seoul National University, Seoul, Republic of Korea. pros53@snu.ac.kr
- 2Department of Periodontology, Seoul National University Dental Hospital, Seoul, Republic of Korea.
- 3Department of Periodontology, Seoul National University School of Dentistry, Seoul, Republic of Korea.
- 4Department of Health Policy and Management, College of Health Science, Korea University, Seoul, Republic of Korea.
- KMID: 2450990
- DOI: http://doi.org/10.4047/jap.2019.11.3.147
Abstract
- PURPOSE
This study aimed to evaluate the effect of two different implant-abutment connection structures with identical implant design on peri-implant bone level.
MATERIALS AND METHODS
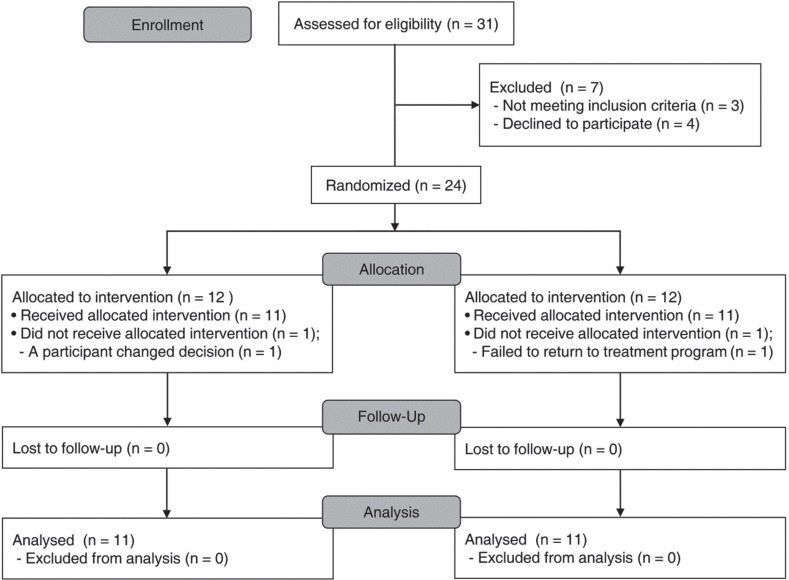
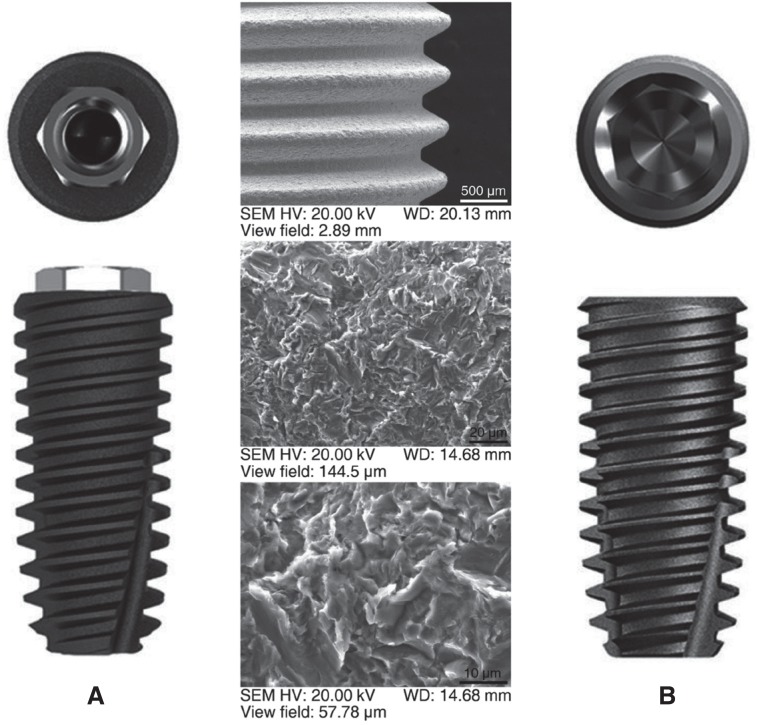
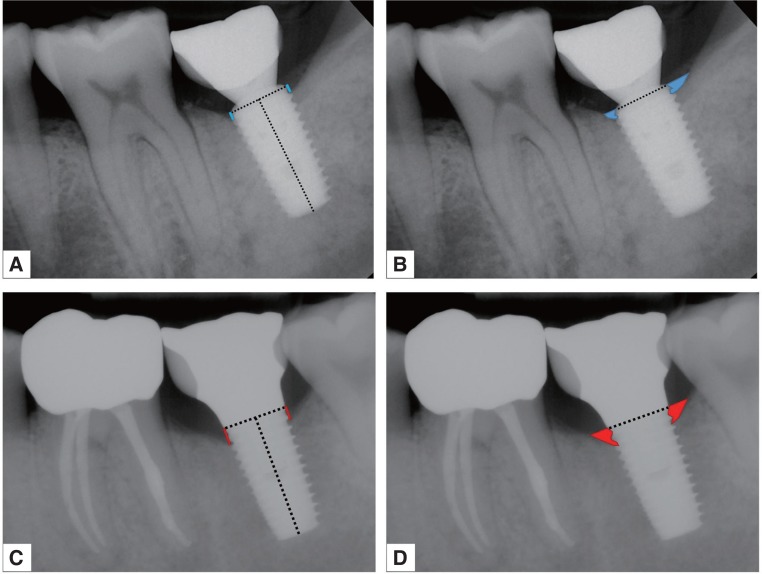
This clinical study was a patient-blind randomized controlled trial following the CONSORT 2010 checklists. This trial was conducted in 24 patients recruited between March 2013 and July 2015. Implants with internal friction connection were compared to those with external hex connection. One implant for each patient was installed, replacing the second molar. Implant-supported crowns were delivered at four months after implant insertion. Standardized periapical radiographs were taken at prosthesis delivery (baseline), and one year after delivery. On the radiographs, distance from implant shoulder to first bone-to-implant contact (DIB) and peri-implant area were measured, which were the primary and secondary outcome, respectively.
RESULTS
Eleven external and eleven internal implants were analyzed. Mean changes of DIB from baseline to 1-year postloading were 0.59 (0.95) mm for the external and 0.01 (0.68) mm for the internal connection. Although no significant differences were found between the two groups, medium effect size was found in DIB between the connections (Cohen's d = 0.67).
CONCLUSION
Considering the effect size in DIB, this study suggested the possibility of the internal friction connection structure for more effective preservation of marginal bone.
MeSH Terms
Figure
Reference
-
1. Lorenz J, Lerner H, Sader RA, Ghanaati S. Investigation of peri-implant tissue conditions and peri-implant tissue stability in implants placed with simultaneous augmentation procedure: a 3-year retrospective follow-up analysis of a newly developed bone level implant system. Int J Implant Dent. 2017; 3:41. PMID: 28875278.
Article2. Rotundo R, Pagliaro U, Bendinelli E, Esposito M, Buti J. Long-term outcomes of soft tissue augmentation around dental implants on soft and hard tissue stability: a systematic review. Clin Oral Implants Res. 2015; 26:123–138.
Article3. Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, Steigmann M, Rebaudi A, Palti A, Pikos MA, Schwartz-Arad D, Choukroun J, Gutierrez-Perez JL, Marenzi G, Valavanis DK. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008; 17:5–15. PMID: 18332753.
Article4. Albrektsson T, Buser D, Sennerby L. Crestal bone loss and oral implants. Clin Implant Dent Relat Res. 2012; 14:783–791. PMID: 23199435.
Article5. Roccuzzo M, De Angelis N, Bonino L, Aglietta M. Ten-year results of a three-arm prospective cohort study on implants in periodontally compromised patients. Part 1: implant loss and radiographic bone loss. Clin Oral Implants Res. 2010; 21:490–496. PMID: 20337668.
Article6. Vigolo P, Gracis S, Carboncini F, Mutinelli S. AIOP (Italian Academy of Prosthetic Dentistry) Clinical Research Group. Internal- vs external-connection single implants: A retrospective study in an italian population treated by certified prosthodontists. Int J Oral Maxillofac Implants. 2016; 31:1385–1396. PMID: 27861666.
Article7. Albrektsson T, Dahlin C, Jemt T, Sennerby L, Turri A, Wennerberg A. Is marginal bone loss around oral implants the result of a provoked foreign body reaction? Clin Implant Dent Relat Res. 2014; 16:155–165. PMID: 24004092.
Article8. Baffone GM, Botticelli D, Pantani F, Cardoso LC, Schweikert MT, Lang NP. Influence of various implant platform configurations on peri-implant tissue dimensions: an experimental study in dog. Clin Oral Implants Res. 2011; 22:438–444. PMID: 21561485.
Article9. Bateli M, Att W, Strub JR. Implant neck configurations for preservation of marginal bone level: a systematic review. Int J Oral Maxillofac Implants. 2011; 26:290–303. PMID: 21483882.10. Hermann JS, Buser D, Schenk RK, Higginbottom FL, Cochran DL. Biologic width around titanium implants. A physiologically formed and stable dimension over time. Clin Oral Implants Res. 2000; 11:1–11.
Article11. Broggini N, McManus LM, Hermann JS, Medina R, Schenk RK, Buser D, Cochran DL. Peri-implant inflammation defined by the implant-abutment interface. J Dent Res. 2006; 85:473–478. PMID: 16632764.
Article12. van Winkelhoff AJ, Goené RJ, Benschop C, Folmer T. Early colonization of dental implants by putative periodontal pathogens in partially edentulous patients. Clin Oral Implants Res. 2000; 11:511–520. PMID: 11168244.
Article13. Nishioka RS, de Vasconcellos LG, de Melo Nishioka GN. Comparative strain gauge analysis of external and internal hexagon, Morse taper, and influence of straight and offset implant configuration. Implant Dent. 2011; 20:e24–e32. PMID: 21448016.
Article14. Ugurel CS, Steiner M, Isik-Ozkol G, Kutay O, Kern M. Mechanical resistance of screwless morse taper and screw-retained implant-abutment connections. Clin Oral Implants Res. 2015; 26:137–142. PMID: 24313278.
Article15. Peñarrocha-Diago MA, Flichy-Fernández AJ, Alonso-González R, Peñarrocha-Oltra D, Balaguer-Martínez J, Peñarrocha-Diago M. Influence of implant neck design and implant-abutment connection type on peri-implant health. Radiological study. Clin Oral Implants Res. 2013; 24:1192–1200. PMID: 22925048.
Article16. Pozzi A, Agliardi E, Tallarico M, Barlattani A. Clinical and radiological outcomes of two implants with different prosthetic interfaces and neck configurations: randomized, controlled, split-mouth clinical trial. Clin Implant Dent Relat Res. 2014; 16:96–106. PMID: 22672713.
Article17. Shin YK, Han CH, Heo SJ, Kim S, Chun HJ. Radiographic evaluation of marginal bone level around implants with different neck designs after 1 year. Int J Oral Maxillofac Implants. 2006; 21:789–794. PMID: 17066642.18. Astrand P, Engquist B, Dahlgren S, Gröndahl K, Engquist E, Feldmann H. Astra Tech and Brånemark system implants: a 5-year prospective study of marginal bone reactions. Clin Oral Implants Res. 2004; 15:413–420. PMID: 15248875.19. Lin MI, Shen YW, Huang HL, Hsu JT, Fuh LJ. A retrospective study of implant-abutment connections on crestal bone level. J Dent Res. 2013; 92:202S–207S. PMID: 24158343.
Article20. Misch CE, Suzuki JB, Misch-Dietsh FM, Bidez MW. A positive correlation between occlusal trauma and peri-implant bone loss: literature support. Implant Dent. 2005; 14:108–116. PMID: 15968181.
Article21. Shinogaya T, Bakke M, Thomsen CE, Vilmann A, Matsumoto M. Bite force and occlusal load in healthy young subjects-a methodological study. Eur J Prosthodont Restor Dent. 2000; 8:11–15. PMID: 11307384.22. Koo KT, Lee EJ, Kim JY, Seol YJ, Han JS, Kim TI, Lee YM, Ku Y, Wikesjö UM, Rhyu IC. The effect of internal versus external abutment connection modes on crestal bone changes around dental implants: a radiographic analysis. J Periodontol. 2012; 83:1104–1109. PMID: 22145806.
Article23. Canullo L, Rosa JC, Pinto VS, Francischone CE, Götz W. Inward-inclined implant platform for the amplified platform-switching concept: 18-month follow-up report of a prospective randomized matched-pair controlled trial. Int J Oral Maxillofac Implants. 2012; 27:927–934. PMID: 22848896.24. Schulz KF, Altman DG, Moher D. CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010; 340:c332. PMID: 20332509.
Article25. Cohen J. The t test for means. In : Cohen J, editor. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Lawrence Erlbaum Associates;1988. p. 20–27.26. Crespi R, Capparè P, Gherlone E. Radiographic evaluation of marginal bone levels around platform-switched and non-platform-switched implants used in an immediate loading protocol. Int J Oral Maxillofac Implants. 2009; 24:920–926. PMID: 19865633.27. Esposito M, Maghaireh H, Pistilli R, Grusovin MG, Lee ST, Trullenque-Eriksson A, Gualini F. Dental implants with internal versus external connections: 5-year post-loading results from a pragmatic multicenter randomised controlled trial. Eur J Oral Implantol. 2016; 9:129–141. PMID: 27314118.28. De Angelis N, Nevins ML, Camelo MC, Ono Y, Campailla M, Benedicenti S. Platform switching versus conventional technique: a randomized controlled clinical trial. Int J Periodontics Restorative Dent. 2014; 34:s75–s79. PMID: 24956095.29. Pozzi A, Tallarico M, Moy PK. Three-year post-loading results of a randomised, controlled, split-mouth trial comparing implants with different prosthetic interfaces and design in partially posterior edentulous mandibles. Eur J Oral Implantol. 2014; 7:47–61. PMID: 24892113.30. Caricasulo R, Malchiodi L, Ghensi P, Fantozzi G, Cucchi A. The influence of implant-abutment connection to peri-implant bone loss: A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2018; 20:653–664. PMID: 29761902.
Article31. Lemos CAA, Verri FR, Bonfante EA, Santiago Júnior JF, Pellizzer EP. Comparison of external and internal implant-abutment connections for implant supported prostheses. A systematic review and meta-analysis. J Dent. 2018; 70:14–22. PMID: 29221955.
Article32. Palacios-Garzón N, Mauri-Obradors E, Roselló-LLabrés X, Estrugo-Devesa A, Jané-Salas E, López-López J. Comparison of marginal bone loss between implants with internal and external connections: A systematic review. Int J Oral Maxillofac Implants. 2018; 33:580–589. PMID: 29763496.
Article33. Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001; 72:1372–1383. PMID: 11699479.
Article34. Guerra E, Pereira C, Faria R, Jorge AO, Bottino MA, de Melo RM. The impact of conical and nonconical abutments on bacterial infiltration at the implant-abutment interface. Int J Periodontics Restorative Dent. 2016; 36:825–831. PMID: 27740643.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Considerations in implant crestal module to preserve peri-implant tissue
- Concept and application of implant connection systems: Part II. Placement and restoration of external connection implant and tissue level implant
- Long-term effect of implant-abutment connection type on marginal bone loss and survival of dental implants
- The influence of the implant-abutment complex on marginal bone and peri-implant conditions: A retrospective study
- Finite element stress analysis of implant prosthesis according to connection types of implant-abutment