J Dent Rehabil Appl Sci.
2020 Dec;36(4):222-231. 10.14368/jdras.2020.36.4.222.
Concept and application of implant connection systems: Part II. Placement and restoration of external connection implant and tissue level implant
- Affiliations
-
- 1Department of Prosthodontics and Research Institute of Oral Science, College of Dentistry, Gangneung-Wonju National University, Gangneung, Republic of Korea
- KMID: 2512117
- DOI: http://doi.org/10.14368/jdras.2020.36.4.222
Abstract
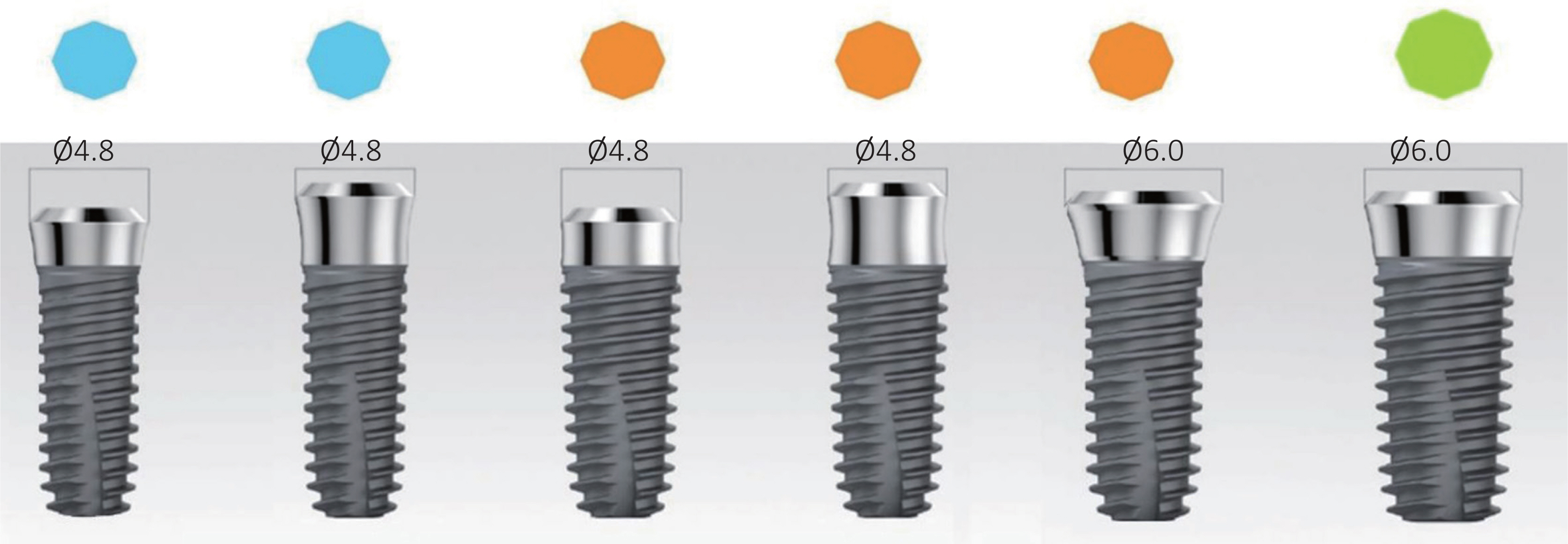
- To use the external connection implant (EXT) appropriately, the inter-implant distance should be carefully considered during placement, and the bones raised above the implants should be trimmed during the second surgery. The hex abutment is more useful than the non-hex abutment. EXT is particularly useful when the inter-arch space is limited. The tissue level (TL, internal butt connection) implant has a biomechanical advantage of coronal wall thickness and a biological advantage of an inherent transmucosal smooth surface. During TL implant restoration, an abutment can be selected using the abutment and fixture margins with considerations for the inter-arch space. Since no single type of implant can satisfy all the cases, it is necessary to select the appropriate type, considering the occlusal force and the bone condition.
Keyword
Figure
Reference
-
References
1. Weng D, Nagata MJ, Bell M, Bosco AF, de Melo LG, Richter EJ. 2008; Influence of microgap location and configuration on the periimplant bone morphology in submerged implants. An experimental study in dogs. Clin Oral Implants Res. 19:1141–7. DOI: 10.1111/j.1600-0501.2008.01564.x. PMID: 18983317.2. Weng D, Nagata MJ, Bell M, de Melo LG, Bosco AF. 2010; Influence of microgap location and configuration on peri-implant bone morphology in nonsubmerged implants: an experimental study in dogs. Int J Oral axillofac Implants. 25:540–7. PMID: 20556253.3. Theoharidou A, Petridis HP, Tzannas K, Garefis P. 2008; Abutment screw loosening in single-implant restorations: a systematic review. Int J Oral Maxillofac Implants. 23:681–90. PMID: 18807565.4. Yi Y, Koak JY, Kim SK, Lee SJ, Heo SJ. 2018; Comparison of implant component fractures in external and internal type: A 12-year retrospective study. J Adv Prosthodont. 10:155–62. DOI: 10.4047/jap.2018.10.2.155. PMID: 29713437. PMCID: PMC5917108.5. Pessoa RS, Muraru L, Júnior EM, Vaz LG, Sloten JV, Duyck J, Jaecques SVN. 2010; Influence of implant connection type on the biomechanical environment of immediately placed implants - CT-based nonlinear, three-dimensional finite element analysis. Clin Implant Dent Relat Res. 12:219–34. DOI: 10.1111/j.1708-8208.2009.00155.x. PMID: 19438946.6. Asvanund P, Morgano SM. 2011; Photoelastic stress analysis of external versus internal implant-abutment connections. J Prosthet Dent. 106:266–71. DOI: 10.1016/S0022-3913(11)60128-5. PMID: 21962585.7. de Almeida Prado Naves Carneiro T, Dietrich L, Prudente MS, da Silva Neto JP, do Prado CJ, de Araújo CA, das Neves FD. 2016; Fracture Resistance of Internal Conical and External Hexagon: Regular and Narrow Implant-Abutment Assemblies. Implant Dent. 25:510–4. DOI: 10.1097/ID.0000000000000446. PMID: 27280738.8. Monje A, Galindo-Moreno P, Tözüm TF, Wang HL. Suárez-López del Amo F. 2016; Into the Paradigm of Local Factors as Contributors for Peri-implant Disease: Short Communication. Int J Oral Maxillofac Implants. 31:288–92. DOI: 10.11607/jomi.4265. PMID: 27004275.9. Tarnow DP, Cho SC, Wallace SS. 2000; The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 71:546–9. DOI: 10.1902/jop.2000.71.4.546. PMID: 10807116.10. Cardaropoli G, Wennström JL, Lekholm U. 2003; Periimplant bone alterations in relation to inter-unit distances. A 3-year retrospective study. Clin Oral Implants Res. 14:430–6. DOI: 10.1034/j.1600-0501.2003.00895.x. PMID: 12869005.11. Jo DW, Yi YJ, Kwon MJ, Kim YK. 2014; Correlation between interimplant distance and crestal bone loss in internal connection implants with platform switching. Int J Oral Maxillofac Implants. 29:296–302. DOI: 10.11607/jomi.3141. PMID: 24683554.12. Lee H, So JS, Hochstedler JL, Ercoli C. 2008; The accuracy of implant impressions: a systematic review. J Prosthet Dent. 100:285–91. DOI: 10.1016/S0022-3913(08)60208-5. PMID: 18922257.13. Gracis S, Michalakis K, Vigolo P, von Steyern PV, Zwahlen M, Sailer I. 2012; Internal vs. external connections for abutments/reconstructions: a systematic review. Clin Oral Implants Res. 23 Suppl 6:202–16. DOI: 10.1111/j.1600-0501.2012.02556.x. PMID: 23062143.14. Cardoso M, Torres MF, Lourenço EJ, de Moraes Telles D, Rodrigues RCS, Ribeiro RF. 2012; Torque removal evaluation of prosthetic screws after tightening and loosening cycles: an in vitro study. Clin Oral Implants Res. 23:475–80. DOI: 10.1111/j.1600-0501.2011.02165.x. PMID: 21457352.15. Ko KH, Park JH, Cho LR. 2019; Considerations for fabrication of cad-cam abutments: Part I. Selection of titanium block and fabrication process. Implantology. 23:46–58. DOI: 10.32542/implantology.2019005.16. Ko KH, Park JH, Cho LR. 2019; Considerations for fabrication of cad-cam abutments: Part II. Designing abutment. Implantology. 23:112–25. DOI: 10.32542/implantology.2019010.17. Hermann JS, Buser D, Schenk RK, Cochran DL. 2000; Crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged and submerged implants in the canine mandible. J Periodontol. 71:1412–24. DOI: 10.1902/jop.2000.71.9.1412. PMID: 11022770.18. Hermann JS, Buser D, Schenk RK, Schoolfield JD, Cochran DL. 2001; Biologic Width around one- and twopiece titanium implants. Clin Oral Implants Res. 12:559–71. DOI: 10.1034/j.1600-0501.2001.120603.x. PMID: 11737099.19. Behneke A, Behneke N. d'Hoedt B. 2002; A 5-year longitudinal study of the clinical effectiveness of ITI solid-screw implants in the treatment of mandibular edentulism. Int J Oral Maxillofac Implants. 17:799–810. PMID: 12507239.20. Buser D, von Arx T. 2000; Surgical procedures in partially edentulous patients with ITI implants. Clin Oral Implants Res. 11 Suppl 1:83–100. DOI: 10.1034/j.1600-0501.2000.011S1083.x. PMID: 11168259.21. Buser D, Mericske-Stern R, Dula K, Kang NP. 1999; Clinical experience with one-stage, non-submerged dental implants. Adv Dent Res. 13:153–61. DOI: 10.1177/08959374990130010501. PMID: 11276738.22. Morton D, Gallucci G, Lin WS, Pjetursson B, Polido W, Roehling S, Sailer I, Aghaloo T, Albera H, Bohner L, Braut V, Buser D, Chen S, Dawson A, Eckert S, Gahlert M, Hamilton A, Jaffin R, Jarry C, Karayazgan B, Laine J, Martin W, Rahman L, Schlegel A, Shiota M, Stilwell C, Vorster C, Zembic A, Zhou W. 2018; Group 2 ITI Consensus Report: Prosthodontics and implant dentistry. Clin Oral Implants Res. 29 Suppl 16:215–23. DOI: 10.1111/clr.13298. PMID: 30328196.23. Alves CC, Muñoz F, Cantalapiedra A, Ramos I, Neves M, Blanco J. 2015; Marginal bone and soft tissue behavior following platform switching abutment connection/disconnection-a dog model study. Clin Oral Implants Res. 26:983–91. DOI: 10.1111/clr.12385. PMID: 24735458.24. Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, Van't Hof MA, Witter DJ, Kalk W, Jansen JA. 2000; Biting and Chewing in Overdentures, Full Dentures, and Natural Dentitions. J Dent Res. 79:1519–24. DOI: 10.1177/00220345000790071501. PMID: 11005738.25. Morneburg TR, Pröschel PA. 2002; Measurement of masticatory forces and implant loads: a methodologic clinical study. Int J Prosthodont. 15:20–7. PMID: 11887595.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concept and application of implant connection systems: Part I. Placement and restoration of internal conical connection implant
- Considerations in implant crestal module to preserve peri-implant tissue
- Retrospective study on marginal bone resorption around immediately loaded implants
- Stress analysis of supporting tissues and implants according to implant fixture shapes and implant-abutment connections
- The influence of implant fixture-abutment connection design on screw loosening