Postoperative Thyroid-Stimulating Hormone Levels Did Not Affect Recurrence after Thyroid Lobectomy in Patients with Papillary Thyroid Cancer
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Korea Cancer Center Hospital, Seoul, Korea.
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. chorong24@gmail.com
- 3Department of Internal Medicine, Healthcare Research Institute, Seoul National University Hospital Healthcare System Gangnam Center, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea. hoonsung80@gmail.com
- KMID: 2450515
- DOI: http://doi.org/10.3803/EnM.2019.34.2.150
Abstract
- BACKGROUND
Thyroid-stimulating hormone (TSH) suppression is recommended for patients who undergo thyroidectomy for differentiated thyroid cancer (DTC). However, the impact of TSH suppression on clinical outcomes in low-risk DTC remains uncertain. Therefore, we investigated the effects of postoperative TSH levels on recurrence in patients with low-risk DTC after thyroid lobectomy.
METHODS
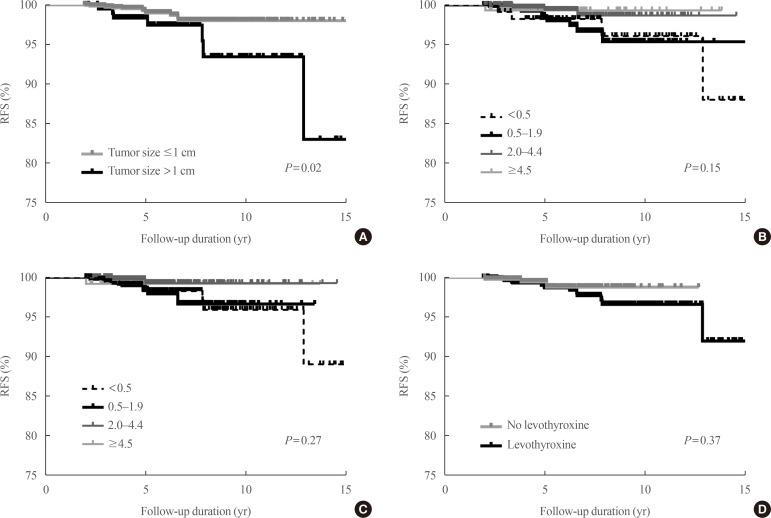
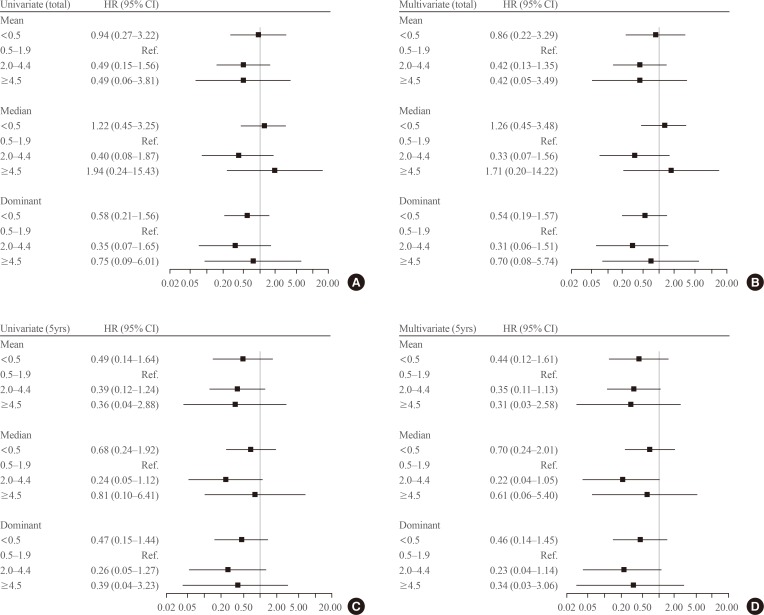
Patients (n=1,528) who underwent thyroid lobectomy for papillary thyroid carcinoma between 2000 and 2012 were included in this study. According to the mean and dominant TSH values during the entire follow-up period or 5 years, patients were divided into four groups (<0.5, 0.5 to 1.9, 2.0 to 4.4, and ≥4.5 mIU/L). Recurrence-free survival was compared among the groups.
RESULTS
During the 5.6 years of follow-up, 21 patients (1.4%) experienced recurrence. Mean TSH levels were within the recommended low-normal range (0.5 to 1.9 mIU/L) during the total follow-up period or 5 years in 38.1% or 36.0% of patients. The mean and dominant TSH values did not affect recurrence-free survival. Adjustment for other risk factors did not alter the results.
CONCLUSION
Serum TSH levels did not affect short-term recurrence in patients with low-risk DTC after thyroid lobectomy. TSH suppression should be conducted more selectively.
MeSH Terms
Figure
Cited by 4 articles
-
Annual Neck Ultrasonography Surveillance between 3 to 12 Years after Thyroid Lobectomy for Papillary Thyroid Microcarcinoma
Jin Gu Kang, Jung Eun Choi, Soo Jung Lee, Su Hwan Kang
Int J Thyroidol. 2020;13(2):142-149. doi: 10.11106/ijt.2020.13.2.142.A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka Hee Yi, Sue K. Park, Eun-Jae Jung, June Young Choi, Ja Seong Bae, Joon Hwa Hong, Kee-Hyun Nam, Young Ki Lee, Hyeong Won Yu, Sujeong Go, Young Mi Kang
Endocrinol Metab. 2021;36(3):574-581. doi: 10.3803/EnM.2020.943.Risk of Subsequent Primary Cancers in Thyroid Cancer Survivors according to the Dose of Levothyroxine: A Nationwide Cohort Study
Min-Su Kim, Jang Won Lee, Min Kyung Hyun, Young Shin Song
Endocrinol Metab. 2024;39(2):288-299. doi: 10.3803/EnM.2023.1815.Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part II. Follow-up Surveillance after Initial Treatment 2024
Mijin Kim, Ji-In Bang, Ho-Cheol Kang, Sun Wook Kim, Dong Gyu Na, Young Joo Park, Youngduk Seo, Young Shin Song, So Won Oh, Sang-Woo Lee, Eun Kyung Lee, Ji Ye Lee, Dong-Jun Lim, Ari Chong, Yun Jae Chung, Chae Moon Hong, Min Kyoung Lee, Bo Hyun Kim
Int J Thyroidol. 2024;17(1):115-146. doi: 10.11106/ijt.2024.17.1.115.
Reference
-
1. Moon JH, Kim KM, Oh TJ, Choi SH, Lim S, Park YJ, et al. The effect of TSH suppression on vertebral trabecular bone scores in patients with differentiated thyroid carcinoma. J Clin Endocrinol Metab. 2017; 102:78–85. PMID: 27754806.2. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133. PMID: 26462967.
Article3. Pötter E, Horn R, Scheumann GF, Dralle H, Costagliola S, Ludgate M, et al. Western blot analysis of thyrotropin receptor expression in human thyroid tumours and correlation with TSH-binding. Biochem Biophys Res Commun. 1994; 205:361–367. PMID: 7999049.4. Brabant G. Thyrotropin suppressive therapy in thyroid carcinoma: what are the targets? J Clin Endocrinol Metab. 2008; 93:1167–1169. PMID: 18390811.
Article5. Cooper DS, Specker B, Ho M, Sperling M, Ladenson PW, Ross DS, et al. Thyrotropin suppression and disease progression in patients with differentiated thyroid cancer: results from the National Thyroid Cancer Treatment Cooperative Registry. Thyroid. 1998; 8:737–744. PMID: 9777742.
Article6. Jonklaas J, Sarlis NJ, Litofsky D, Ain KB, Bigos ST, Brierley JD, et al. Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid. 2006; 16:1229–1242. PMID: 17199433.
Article7. McGriff NJ, Csako G, Gourgiotis L, Lori CG, Pucino F, Sarlis NJ. Effects of thyroid hormone suppression therapy on adverse clinical outcomes in thyroid cancer. Ann Med. 2002; 34:554–564. PMID: 12553495.
Article8. Hovens GC, Stokkel MP, Kievit J, Corssmit EP, Pereira AM, Romijn JA, et al. Associations of serum thyrotropin concentrations with recurrence and death in differentiated thyroid cancer. J Clin Endocrinol Metab. 2007; 92:2610–2615. PMID: 17426094.
Article9. Parker WA, Edafe O, Balasubramanian SP. Long-term treatment-related morbidity in differentiated thyroid cancer: a systematic review of the literature. Pragmat Obs Res. 2017; 8:57–67. PMID: 28553154.
Article10. Klein Hesselink EN, Klein Hesselink MS, de Bock GH, Gansevoort RT, Bakker SJ, Vredeveld EJ, et al. Long-term cardiovascular mortality in patients with differentiated thyroid carcinoma: an observational study. J Clin Oncol. 2013; 31:4046–4053. PMID: 24101052.
Article11. Pajamaki N, Metso S, Hakala T, Ebeling T, Huhtala H, Ryodi E, et al. Long-term cardiovascular morbidity and mortality in patients treated for differentiated thyroid cancer. Clin Endocrinol (Oxf). 2018; 88:303–310. PMID: 29154445.12. Wang LY, Smith AW, Palmer FL, Tuttle RM, Mahrous A, Nixon IJ, et al. Thyrotropin suppression increases the risk of osteoporosis without decreasing recurrence in ATA low- and intermediate-risk patients with differentiated thyroid carcinoma. Thyroid. 2015; 25:300–307. PMID: 25386760.
Article13. Tournis S, Antoniou JD, Liakou CG, Christodoulou J, Papakitsou E, Galanos A, et al. Volumetric bone mineral density and bone geometry assessed by peripheral quantitative computed tomography in women with differentiated thyroid cancer under TSH suppression. Clin Endocrinol (Oxf). 2015; 82:197–204. PMID: 25040693.
Article14. Sugitani I, Fujimoto Y. Effect of postoperative thyrotropin suppressive therapy on bone mineral density in patients with papillary thyroid carcinoma: a prospective controlled study. Surgery. 2011; 150:1250–1257. PMID: 22136848.
Article15. Carhill AA, Litofsky DR, Ross DS, Jonklaas J, Cooper DS, Brierley JD, et al. Long-term outcomes following therapy in differentiated thyroid carcinoma: NTCTCS registry analysis 1987–2012. J Clin Endocrinol Metab. 2015; 100:3270–3279. PMID: 26171797.
Article16. Sugitani I, Fujimoto Y. Does postoperative thyrotropin suppression therapy truly decrease recurrence in papillary thyroid carcinoma? A randomized controlled trial. J Clin Endocrinol Metab. 2010; 95:4576–4583. PMID: 20660039.
Article17. Park S, Kim WG, Han M, Jeon MJ, Kwon H, Kim M, et al. Thyrotropin suppressive therapy for low-risk small thyroid cancer: a propensity score-matched cohort study. Thyroid. 2017; 27:1164–1170. PMID: 28699428.
Article18. Cox C, Bosley M, Southerland LB, Ahmadi S, Perkins J, Roman S, et al. Lobectomy for treatment of differentiated thyroid cancer: can patients avoid postoperative thyroid hormone supplementation and be compliant with the American Thyroid Association guidelines? Surgery. 2018; 163:75–80. PMID: 29122328.
Article19. Park S, Jeon MJ, Song E, Oh HS, Kim M, Kwon H, et al. Clinical features of early and late postoperative hypothyroidism after lobectomy. J Clin Endocrinol Metab. 2017; 102:1317–1324. PMID: 28324106.
Article20. Ebina A, Sugitani I, Fujimoto Y, Yamada K. Risk-adapted management of papillary thyroid carcinoma according to our own risk group classification system: is thyroid lobectomy the treatment of choice for low-risk patients? Surgery. 2014; 156:1579–1588. PMID: 25262223.21. Park YM, Lee DY, Oh KH, Cho JG, Baek SK, Kwon SY, et al. Clinical implications of pathologic factors after thyroid lobectomy in patients with papillary thyroid carcinoma. Oral Oncol. 2017; 75:1–5. PMID: 29224804.
Article22. Kim SK, Park I, Woo JW, Lee JH, Choe JH, Kim JH, et al. Total thyroidectomy versus lobectomy in conventional papillary thyroid microcarcinoma: analysis of 8,676 patients at a single institution. Surgery. 2017; 161:485–492. PMID: 27593085.
Article23. Matsuzu K, Sugino K, Masudo K, Nagahama M, Kitagawa W, Shibuya H, et al. Thyroid lobectomy for papillary thyroid cancer: long-term follow-up study of 1,088 cases. World J Surg. 2014; 38:68–79. PMID: 24081532.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thyroid Lobectomy as an Initial Treatment Option on 1-4 cm Papillary Cancer
- Risk Factors for Hypothyroidism after Thyroid Lobectomy with Papillary Thyroid Crcinoma according to Existence of Thyroiditis
- Postoperative Surveillance of Thyroid Cancer: in View of US
- Postoperative Surveillance of Thyroid Cancer: In View of a Radiologist
- Guidelines for the Postoperative Treatment of Thyroid Cancer: Levothyroxine and Calcium/Vitamin D Supplements