J Endocr Surg.
2019 Jun;19(2):35-44. 10.16956/jes.2019.19.2.35.
Parathyroid Cancer: Comparison with Benign Hyperparathyroidism
- Affiliations
-
- 1Department of Pathology, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- 2Department of Surgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea. dryooseung@gilhospital.com, dryooseung@hanmail.net
- 3Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- KMID: 2450488
- DOI: http://doi.org/10.16956/jes.2019.19.2.35
Abstract
- PURPOSE
The preoperative diagnosis of parathyroid cancer (PC) is challenging. The purpose of this study was to identify the differences between PC and benign primary hyperparathyroidism.
METHODS
The medical records of 85 hyperparathyroidism patients that underwent surgery between 2001 and 2017 were retrospectively reviewed.
RESULTS
Seven of the 85 were diagnosed with PC. Mean age was 53.0±13.0 years and 66 (77.6%) were women. Follow-up duration was 52.9±44.4 months. Tumors were larger (3.50±1.26 cm vs. 2.10±0.84 cm, P=0.002), and intact parathyroid hormone (iPTH) (1,142.8±524.5 pg/mL vs. 461.2±513.5 pg/mL, P=0.002) and alkaline phosphatase (ALP) (398.6±493.6 U/L vs. 166.7±181.1 U/L, P=0.01) levels were higher in cancer patients than in benign primary hyperparathyroidism. Intraoperatively, adhesion to surrounding soft tissue or the thyroid gland was detected more frequently in cancer (85.7% vs. 12.8%, P<0.001). Two patients experienced recurrences and one of them died from PC.
CONCLUSION
PC patients had larger tumors size, and higher serum iPTH and ALP levels. Intraoperative detection of adhesion to surrounding soft tissue/thyroid importantly raised suspicion of PC. Surgeons operating for hyperparathyroidism should be prepared to perform an appropriate en bloc resection initially upon suspicion of PC.
MeSH Terms
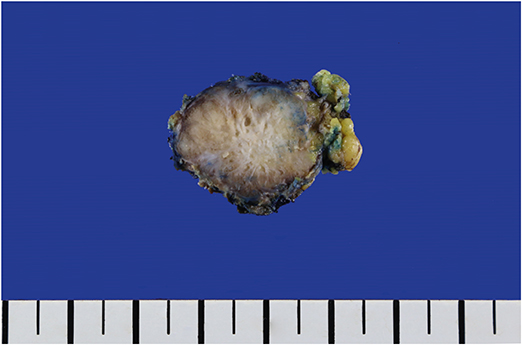
Figure
Reference
-
1. Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL. Sabiston Textbook of Surgery: the Biological Basis of Modern Surgical Practice. 20th ed. Philadelphia (PA): Elsevier Saunders;2017.2. Korea Central Cancer Registry. National Cancer Center (KR). Ministry of Health and Welfare (KR). Annual Report of Cancer Statistics in Korea in 2015. Goyang: Korea Central Cancer Registry;2017.3. Lloyd RV, Osamura RY, Klöppel G, Rosai J. World Health Organization. International Agency for Research on Cancer. WHO Classification of Tumours of Endocrine Organs. 4th ed. Lyon: International Agency for Research on Cancer;2017.4. Al-Kurd A, Mekel M, Mazeh H. Parathyroid carcinoma. Surg Oncol. 2014; 23:107–114.
Article5. Owen RP, Silver CE, Pellitteri PK, Shaha AR, Devaney KO, Werner JA, et al. Parathyroid carcinoma: a review. Head Neck. 2011; 33:429–436.
Article6. Talat N, Schulte KM. Clinical presentation, staging and long-term evolution of parathyroid cancer. Ann Surg Oncol. 2010; 17:2156–2174.
Article7. Schulte KM, Talat N, Galata G, Gilbert J, Miell J, Hofbauer LC, et al. Oncologic resection achieving R0 margins improves disease-free survival in parathyroid cancer. Ann Surg Oncol. 2014; 21:1891–1897.
Article8. Givi B, Shah JP. Parathyroid carcinoma. Clin Oncol (R Coll Radiol). 2010; 22:498–507.
Article9. Ricci G, Assenza M, Barreca M, Liotta G, Paganelli L, Serao A, et al. Parathyroid carcinoma: the importance of high clinical suspicion for a correct management. Int J Surg Oncol. 2012; 2012:649148.
Article10. Shane E. Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab. 2001; 86:485–493.11. Kassahun WT, Jonas S. Focus on parathyroid carcinoma. Int J Surg. 2011; 9:13–19.
Article12. Duan K, Mete Ö. Parathyroid carcinoma: diagnosis and clinical implications. Turk Patoloji Derg. 2015; 31:Suppl 1. 80–97.
Article13. Kim BS, Ryu HS, Kang KH, Park SJ. Parathyroid carcinoma in tertiary hyperparathyroidism. Asian J Surg. 2016; 39:255–259.
Article14. Takada D, Tsukamoto T, Fuse M, Kada S, Yanagita M. The use of cinacalcet hinders the diagnosis of parathyroid carcinoma in a chronic dialysis patient: a case report. BMC Nephrol. 2017; 18:315.
Article15. Bossola M, Tazza L, Ferrante A, Giungi S, Carbone A, Gui D, et al. Parathyroid carcinoma in a chronic hemodialysis patient: case report and review of the literature. Tumori. 2005; 91:558–562.
Article16. Falvo L, Catania A, Palermo S, Sorrenti S, Bonifazi AP, De Stefano M, et al. Bilateral synchronous parathyroid carcinoma in a patient on long-term hemodialysis: presentation of a rare clinical case and review literature. Int Surg. 2005; 90:18–22.17. Zivaljevic V, Krgovic K, Tatic S, Havelka M, Dimitrijevic Z, Diklic A, et al. Parathyroid cancer in a hemodialysis patient: a case report. Tumori. 2002; 88:430–432.
Article18. Bondeson L, Sandelin K, Grimelius L. Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol. 1993; 17:820–829.
Article19. Snover DC, Foucar K. Mitotic activity in benign parathyroid disease. Am J Clin Pathol. 1981; 75:345–347.
Article20. Ippolito G, Palazzo FF, Sebag F, De Micco C, Henry JF. Intraoperative diagnosis and treatment of parathyroid cancer and atypical parathyroid adenoma. Br J Surg. 2007; 94:566–570.
Article21. DeLellis RA. Parathyroid tumors and related disorders. Mod Pathol. 2011; 24:Suppl 2. S78–S93.
Article22. Stojadinovic A, Hoos A, Nissan A, Dudas ME, Cordon-Cardo C, Shaha AR, et al. Parathyroid neoplasms: clinical, histopathological, and tissue microarray-based molecular analysis. Hum Pathol. 2003; 34:54–64.
Article23. Fernandez-Ranvier GG, Khanafshar E, Tacha D, Wong M, Kebebew E, Duh QY, et al. Defining a molecular phenotype for benign and malignant parathyroid tumors. Cancer. 2009; 115:334–344.
Article24. Baek CO, Kim KH, Song SK. Synchronous parathyroid carcinoma and papillary thyroid carcinoma in a patient with long-standing schizophrenia. Korean J Intern Med. 2017; 32:1104–1107.
Article25. Chaychi L, Belbruno K, Golding A, Memoli V. Unusual manifestation of parathyroid carcinoma in the setting of papillary thyroid cancer. Endocr Pract. 2010; 16:664–668.
Article26. Savli H, Sevinc A, Sari R, Ozen S, Buyukberber S, Ertas E. Occult parathyroid carcinoma in a patient with papillary thyroid carcinoma and Hashimoto's thyroiditis. J Endocrinol Invest. 2001; 24:42–44.
Article27. Kim JK, Chai YJ, Chung JK, Hwang KT, Heo SC, Kim SJ, et al. The prevalence of primary hyperparathyroidism in Korea: a population-based analysis from patient medical records. Ann Surg Treat Res. 2018; 94:235–239.
Article28. Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS, et al. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006; 21:171–177.
Article29. Adami S, Marcocci C, Gatti D. Epidemiology of primary hyperparathyroidism in Europe. J Bone Miner Res. 2002; 17:Suppl 2. N18–N23.30. Yu N, Donnan PT, Murphy MJ, Leese GP. Epidemiology of primary hyperparathyroidism in Tayside, Scotland, UK. Clin Endocrinol (Oxf). 2009; 71:485–493.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parathyroid Adenoma without Hyperparathyroidism Presenting as a Large Neck Mass
- Benign Recurrent Primary Hyperparathyroidism After Parathyroid Carcinoma
- Coexistence of Parathyroid and Papillary Thyroid Carcinoma
- A Case Report of Primary Hyperparathyroidism Caused by Parathyroid Carcinoma
- A Case of Functioning Parathyroid Cancer with Hypokalemia