Yonsei Med J.
2015 May;56(3):658-665. 10.3349/ymj.2015.56.3.658.
The Effect of Specialized Continuous Renal Replacement Therapy Team in Acute Kidney Injury Patients Treatment
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. ohjmd@yuhs.ac
- KMID: 2450338
- DOI: http://doi.org/10.3349/ymj.2015.56.3.658
Abstract
- PURPOSE
Continuous renal replacement therapy (CRRT) has been established for critically ill acute kidney injury (AKI) patients. In addition, some centers consist of a specialized CRRT team (SCT) with physicians and nurses. To our best knowledge, however, ona a few studies have yet been carried out on the superiority of SCT management.
MATERIALS AND METHODS
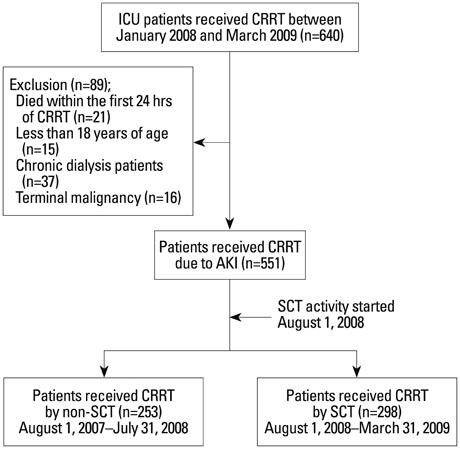
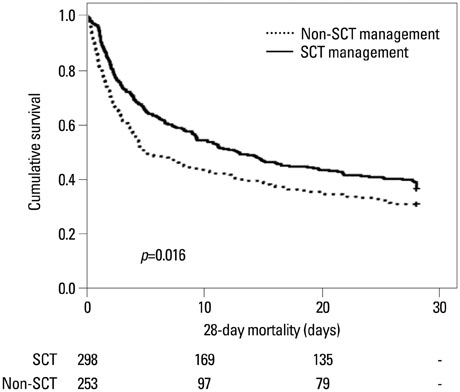
A total of 551 patients, who received CRRT between January 2008 and March 2009, were divided into two groups based on the controller of CRRT. The impact of the CRRT management on 28-day mortality was compared between two groups by Kaplan-Meier curve and Cox analysis.
RESULTS
During the study period, the number of filters used, down-time per day, and intensive care unit length of day were significantly higher in non-SCT group than in SCT group (6.2 hrs vs. 5.0 hrs, p=0.042; 5.0 hrs vs. 3.8 hrs, p<0.001; 27.5 days vs. 21.1 days, p=0.027, respectively), while net ultrafiltration rate was significantly lower in non-SCT group than SCT group (28.0 mL/kg/hr vs. 29.5 mL/kg/hr, p=0.043, respectively). In addition, 28-day mortality rate was significantly lower in SCT group than with non-SCT group (p=0.031). Moreover, Cox regression analysis showed that 28-day mortality rate was significantly lower in SCT control group, even after adjusting for age, gender, severity scores, biomarkers, risk, injury, failure, loss, and end-stage renal disease, and contributing factors (hazard ratio 0.91, p=0.046).
CONCLUSION
A well-trained CRRT team could be beneficial for mortality improvement of AKI patients requiring CRRT.
MeSH Terms
-
Acute Kidney Injury/mortality/*therapy
Adult
Aged
Aged, 80 and over
Biological Markers
Critical Illness/*mortality/therapy
Female
Humans
Intensive Care Units
Kaplan-Meier Estimate
Kidney Failure, Chronic/*therapy
Male
Middle Aged
Patient Care Team
Proportional Hazards Models
Renal Replacement Therapy/*methods
Retrospective Studies
Time Factors
Treatment Outcome
Biological Markers
Figure
Reference
-
1. Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006; 10:R73.2. Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005; 294:813–818.
Article3. Ahlström A, Tallgren M, Peltonen S, Räsänen P, Pettilä V. Survival and quality of life of patients requiring acute renal replacement therapy. Intensive Care Med. 2005; 31:1222–1228.
Article4. Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, et al. Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit Care. 2005; 9:R700–R709.5. Morgera S, Kraft AK, Siebert G, Luft FC, Neumayer HH. Long-term outcomes in acute renal failure patients treated with continuous renal replacement therapies. Am J Kidney Dis. 2002; 40:275–279.
Article6. Ostermann M, Chang RW. Correlation between parameters at initiation of renal replacement therapy and outcome in patients with acute kidney injury. Crit Care. 2009; 13:R175.
Article7. Lins RL, Elseviers MM, Van der Niepen P, Hoste E, Malbrain ML, Damas P, et al. Intermittent versus continuous renal replacement therapy for acute kidney injury patients admitted to the intensive care unit: results of a randomized clinical trial. Nephrol Dial Transplant. 2009; 24:512–518.
Article8. Allegretti AS, Steele DJ, David-Kasdan JA, Bajwa E, Niles JL, Bhan I. Continuous renal replacement therapy outcomes in acute kidney injury and end-stage renal disease: a cohort study. Crit Care. 2013; 17:R109.
Article9. Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, et al. Continuous renal replacement therapy: a worldwide practice survey. The beginning and ending supportive therapy for the kidney (B.E.S.T. kidney) investigators. Intensive Care Med. 2007; 33:1563–1570.
Article10. Oh HJ, Park JT, Kim JK, Yoo DE, Kim SJ, Han SH, et al. Red blood cell distribution width is an independent predictor of mortality in acute kidney injury patients treated with continuous renal replacement therapy. Nephrol Dial Transplant. 2012; 27:589–594.
Article11. Zhang Z, Ni H, Lu B. Variables associated with circuit life span in critically ill patients undergoing continuous renal replacement therapy: a prospective observational study. ASAIO J. 2012; 58:46–50.
Article12. Gilbert RW, Caruso DM, Foster KN, Canulla MV, Nelson ML, Gilbert EA. Development of a continuous renal replacement program in critically ill patients. Am J Surg. 2002; 184:526–532.
Article13. Meißner A, Schlenke P. Massive Bleeding and Massive Transfusion. Transfus Med Hemother. 2012; 39:73–84.
Article14. Uchino S, Fealy N, Baldwin I, Morimatsu H, Bellomo R. Continuous is not continuous: the incidence and impact of circuit "down-time" on uraemic control during continuous veno-venous haemofiltration. Intensive Care Med. 2003; 29:575–578.
Article15. Webb AR, Mythen MG, Jacobson D, Mackie IJ. Maintaining blood flow in the extracorporeal circuit: haemostasis and anticoagulation. Intensive Care Med. 1995; 21:84–93.
Article16. Baldwin IC, Elderkin TD. Continuous hemofiltration: nursing perspectives in critical care. New Horiz. 1995; 3:738–747.17. Tolwani AJ, Campbell RC, Stofan BS, Lai KR, Oster RA, Wille KM. Standard versus high-dose CVVHDF for ICU-related acute renal failure. J Am Soc Nephrol. 2008; 19:1233–1238.18. VA/NIH Acute Renal Failure Trial Network. Palevsky PM, Zhang JH, O'Connor TZ, Chertow GM, Crowley ST, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008; 359:7–20.
Article19. RENAL Replacement Therapy Study Investigators. Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, et al. Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med. 2009; 361:1627–1638.
Article20. Saudan P, Niederberger M, De Seigneux S, Romand J, Pugin J, Perneger T, et al. Adding a dialysis dose to continuous hemofiltration increases survival in patients with acute renal failure. Kidney Int. 2006; 70:1312–1317.
Article21. Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, et al. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet. 2000; 356:26–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Continuous renal replacement therapy in elderly with acute kidney injury
- Acute kidney injury and continuous renal replacement therapy in children; what pediatricians need to know
- Renal Replacement Therapy in Acute Kidney Injury: Indication, Proper Initiation, and Prescription
- Continuous Renal Replacement Therapy in Infants and Neonates
- When and why to start continuous renal replacement therapy in critically ill patients with acute kidney injury