Intest Res.
2019 Apr;17(2):210-217. 10.5217/ir.2018.00081.
The effect of vitamin D administration on inflammatory markers in patients with inflammatory bowel disease
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. bodnsoul@hanmail.net
- KMID: 2449962
- DOI: http://doi.org/10.5217/ir.2018.00081
Abstract
- BACKGROUND/AIMS
The exact relationship between vitamin D deficiency and inflammatory bowel disease (IBD) remains unclear. We evaluated the effect of vitamin D3 administration on inflammatory responses and disease severity in patients with IBD.
METHODS
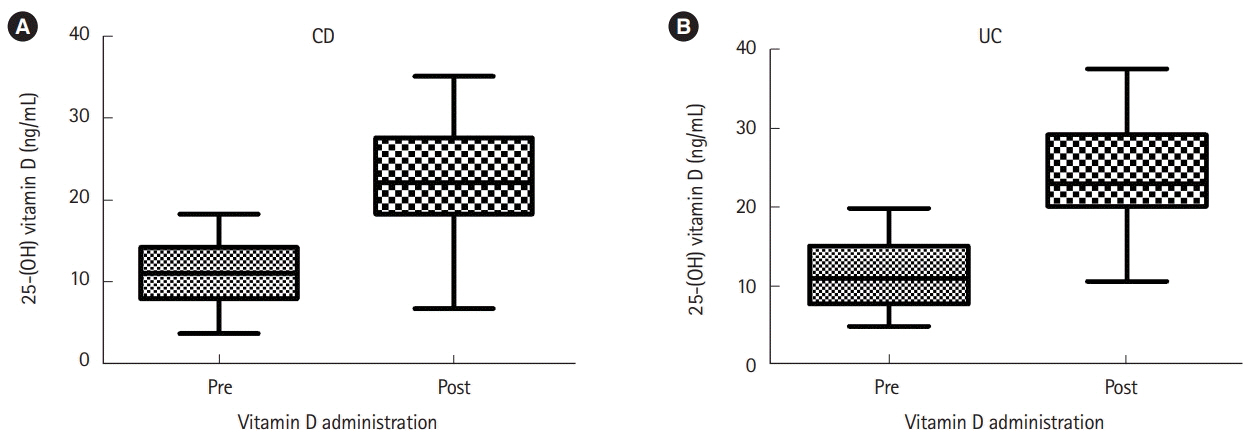
We investigated the serum 25-hydroxyvitamin D3 [25-(OH)D], C-reactive protein (CRP) levels and the partial Mayo score (PMS) in patients with IBD. Vitamin D3 was administered in patients with either vitamin D deficiency or insufficiency and CRP, serum vitamin D levels and PMS were re-examined at 6 months of administration.
RESULTS
In 88 patients with Crohn's disease (CD), a negative correlation was found between serum vitamin D and CRP. In 178 patients with ulcerative colitis (UC), serum vitamin D showed no association with CRP or PMS. Serum vitamin D increased from 11.08±3.63 to 22.69±6.11 ng/mL in 29 patients with CD and from 11.45±4.10 to 24.20±6.61 ng/mL in 41 patients with UC who received vitamin D3 treatment (P<0.001 and P<0.001, respectively). In patients with CD, median ΔCRP was -0.24 in the normalized vitamin D group and -0.11 in the non-normalized group (P=0.308). In patients with UC, median ΔCRP was −0.01 in the normalized vitamin D group and 0.06 in the non-normalized group (P=0.359).
CONCLUSIONS
Although a negative correlation was found between serum vitamin D and CRP levels in patients with CD, administration of vitamin D did not improve the CRP level in patients with CD. In patients with UC, serum vitamin D level was unrelated to CRP or PMS.
MeSH Terms
Figure
Cited by 2 articles
-
Inflammatory Bowel Disease and Vitamin D
Ki Bae Kim, Hyoung Woo Kim, Jun Su Lee, Soon Man Yoon
Korean J Gastroenterol. 2020;76(6):275-281. doi: 10.4166/kjg.2020.160.Can vitamin D supplementation help control inflammation in inflammatory bowel disease beyond its classical role in bone health?
Sung Wook Hwang
Intest Res. 2019;17(2):157-159. doi: 10.5217/ir.2019.00038.
Reference
-
1. Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009; 361:2066–2078.
Article2. Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011; 474:307–317.
Article3. Jones G, Strugnell SA, DeLuca HF. Current understanding of the molecular actions of vitamin D. Physiol Rev. 1998; 78:1193–1231.
Article4. Sadeghian M, Saneei P, Siassi F, Esmaillzadeh A. Vitamin D status in relation to Crohn’s disease: meta-analysis of observational studies. Nutrition. 2016; 32:505–514.
Article5. Han YM, Yoon H, Lim S, et al. Risk factors for vitamin d, zinc, and selenium deficiencies in Korean patients with inflammatory bowel disease. Gut Liver. 2017; May. 15. 11:363–369.
Article6. Ulitsky A, Ananthakrishnan AN, Naik A, et al. Vitamin D deficiency in patients with inflammatory bowel disease: association with disease activity and quality of life. JPEN J Parenter Enteral Nutr. 2011; 35:308–316.
Article7. Joseph AJ, George B, Pulimood AB, Seshadri MS, Chacko A. 25 (OH) vitamin D level in Crohn’s disease: association with sun exposure & disease activity. Indian J Med Res. 2009; 130:133–137.8. Garg M, Rosella O, Lubel JS, Gibson PR. Association of circulating vitamin D concentrations with intestinal but not systemic inflammation in inflammatory bowel disease. Inflamm Bowel Dis. 2013; 19:2634–2643.
Article9. Hassan V, Hassan S, Seyed-Javad P, et al. Association between serum 25 (OH) vitamin D concentrations and inflammatory bowel diseases (IBDs) activity. Med J Malaysia. 2013; 68:34–38.10. Ardesia M, Ferlazzo G, Fries W. Vitamin D and inflammatory bowel disease. Biomed Res Int. 2015; 2015:470805.
Article11. Jørgensen SP, Agnholt J, Glerup H, et al. Clinical trial: vitamin D3 treatment in Crohn’s disease: a randomized double-blind placebo-controlled study. Aliment Pharmacol Ther. 2010; 32:377–383.
Article12. Jørgensen SP, Hvas CL, Agnholt J, Christensen LA, Heickendorff L, Dahlerup JF. Active Crohn’s disease is associated with low vitamin D levels. J Crohns Colitis. 2013; 7:e407–e413.
Article13. Ham M, Longhi MS, Lahiff C, Cheifetz A, Robson S, Moss AC. Vitamin D levels in adults with Crohn’s disease are responsive to disease activity and treatment. Inflamm Bowel Dis. 2014; 20:856–860.
Article14. Kelly P, Suibhne TN, O’Morain C, O’Sullivan M. Vitamin D status and cytokine levels in patients with Crohn’s disease. Int J Vitam Nutr Res. 2011; 81:205–210.
Article15. Raftery T, Merrick M, Healy M, et al. Vitamin D status is associated with intestinal inflammation as measured by fecal calprotectin in Crohn’s disease in clinical remission. Dig Dis Sci. 2015; 60:2427–2435.
Article16. Tajika M, Matsuura A, Nakamura T, et al. Risk factors for vitamin D deficiency in patients with Crohn’s disease. J Gastroenterol. 2004; 39:527–533.
Article17. Raftery T, Martineau AR, Greiller CL, et al. Effects of vitamin D supplementation on intestinal permeability, cathelicidin and disease markers in Crohn’s disease: results from a randomised double-blind placebo-controlled study. United European Gastroenterol J. 2015; 3:294–302.
Article18. Khalili H, Huang ES, Ananthakrishnan AN, et al. Geographical variation and incidence of inflammatory bowel disease among US women. Gut. 2012; 61:1686–1692.
Article19. Prevention and management of osteoporosis. World Health Organ Tech Rep Ser. 2003; 921:1–164.20. Institute of Medicine; Food and Nutrition Board; Committee to Review Dietary Reference Intakes for Vitamin D and Calcium, et al. Dietary reference intakes for calcium and vitamin D. Washington, DC: National Academies Press (US) National Academy of Sciences;2011.21. Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R. Estimates of optimal vitamin D status. Osteoporos Int. 2005; 16:713–716.
Article22. Yang L, Weaver V, Smith JP, Bingaman S, Hartman TJ, Cantorna MT. Therapeutic effect of vitamin d supplementation in a pilot study of Crohn’s patients. Clin Transl Gastroenterol. 2013; 4:e33.
Article23. Ye L, Lin Z, Liu J, Cao Q. Vitamin D deficiency is associated with endoscopic severity in patients with Crohn’s disease. Gastroenterol Res Pract. 2017; 2017:4869718.
Article24. Klingberg E, Oleröd G, Konar J, Petzold M, Hammarsten O. Seasonal variations in serum 25-hydroxy vitamin D levels in a Swedish cohort. Endocrine. 2015; 49:800–808.
Article25. Thuesen B, Husemoen L, Fenger M, et al. Determinants of vitamin D status in a general population of Danish adults. Bone. 2012; 50:605–610.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can vitamin D supplementation help control inflammation in inflammatory bowel disease beyond its classical role in bone health?
- Inflammatory Bowel Disease and Vitamin D
- Management of Anemia in Patients with Inflammatory Bowel Disease
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence
- Association of Vitamin D with Inflammatory Bowel Disease Activity in Pediatric Patients