J Pathol Transl Med.
2019 May;53(3):164-172. 10.4132/jptm.2019.02.12.
Potential Role for a Panel of Immunohistochemical Markers in the Management of Endometrial Carcinoma
- Affiliations
-
- 1Department of Pathology, Faculty of Medicine, Mansoura University, Mansoura, Egypt. marafa8@yahoo.com
- 2Department of Pathology, College of Medicine and Health Sciences, Sultan Qaboos University, Muscat, Oman.
- 3Department of Clinical Oncology and Nuclear Medicine, Faculty of Medicine, Mansoura University, Mansoura, Egypt.
- 4Department of Obstetrics and Gynecology, Faculty of Medicine, Mansoura University, Mansoura, Egypt.
- KMID: 2449339
- DOI: http://doi.org/10.4132/jptm.2019.02.12
Abstract
- BACKGROUND
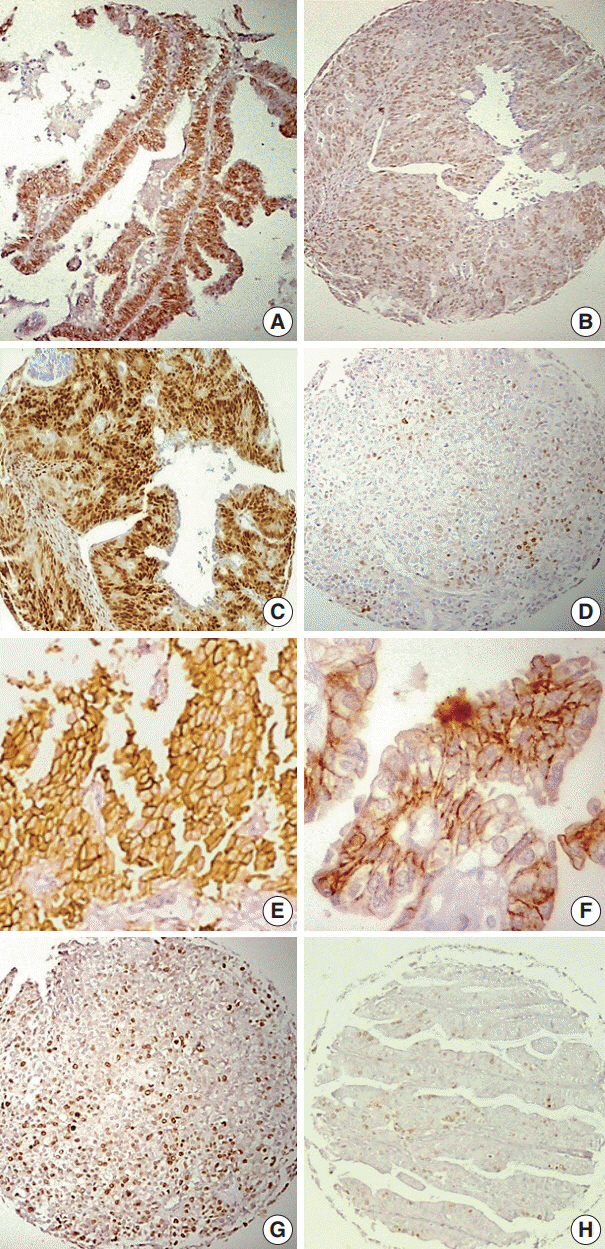
In order to improve the efficacy of endometrial carcinoma (EC) treatment, identifying prognostic factors for high risk patients is a high research priority. This study aimed to assess the relationships among the expression of estrogen receptors (ER), progesterone receptors (PR), human epidermal growth factor receptor 2 (HER2), Ki-67, and the different histopathological prognostic parameters in EC and to assess the value of these in the management of EC.
METHODS
We examined 109 cases of EC. Immunohistochemistry for ER, PR, HER2, and Ki-67 were evaluated in relation to age, tumor size, International Federation of Gynecology and Obstetrics (FIGO) stage and grade, depth of infiltration, cervical and ovarian involvement, lymphovascular space invasion (LVSI), and lymph node (LN) metastasis.
RESULTS
The mean age of patients in this study was 59.8 ± 8.2 years. Low ER and PR expression scores and high Ki-67 expression showed highly significant associations with non-endometrioid histology (p = .007, p < .001, and p < .001, respectively) and poor differentiation (p = .007, p < .001, and p <. 001, respectively). Low PR score showed a significant association with advanced stage (p = .009). Low ER score was highly associated with LVSI (p = .006), and low PR scores were associated significantly with LN metastasis (p = .026). HER2 expression was significantly related to advanced stages (p = .04), increased depth of infiltration (p = .02), LVSI (p = .017), ovarian involvement (p = .038), and LN metastasis (p = .038). There was a close relationship between HER2 expression and uterine cervical involvement (p = .009). Higher Ki-67 values were associated with LN involvement (p = .012).
CONCLUSIONS
The over-expression of HER2 and Ki-67 and low expression of ER and PR indicate a more malignant EC behavior. An immunohistochemical panel for the identification of high risk tumors can contribute significantly to prognostic assessments.
Keyword
MeSH Terms
Figure
Reference
-
1. Le Gallo M, Bell DW. The emerging genomic landscape of endometrial cancer. Clin Chem. 2014; 60:98–110.
Article2. Llaurado M, Ruiz A, Majem B, et al. Molecular bases of endometrial cancer: new roles for new actors in the diagnosis and the therapy of the disease. Mol Cell Endocrinol. 2012; 358:244–55.3. Backes FJ, Walker CJ, Goodfellow PJ, et al. Estrogen receptor-alpha as a predictive biomarker in endometrioid endometrial cancer. Gynecol Oncol. 2016; 141:312–7.
Article4. Yu CG, Jiang XY, Li B, Gan L, Huang JF. Expression of ER, PR, CerbB-2 and Ki-67 in endometrial carcinoma and their relationships with the clinicopathological features. Asian Pac J Cancer Prev. 2015; 16:6789–94.
Article5. Arafa M, Somja J, Dehan P, et al. Current concepts in the pathology and epigenetics of endometrial carcinoma. Pathology. 2010; 42:613–7.
Article6. Markova I, Duskova M, Lubusky M, et al. Selected immunohistochemical prognostic factors in endometrial cancer. Int J Gynecol Cancer. 2010; 20:576–82.
Article7. Lapinska-Szumczyk S, Supernat A, Majewska H, et al. HER2-positive endometrial cancer subtype carries poor prognosis. Clin Transl Sci. 2014; 7:482–8.8. Cancer Genome Atlas Research Network, Kandoth C, Schultz N, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013; 497:67–73.
Article9. Faria SC, Sagebiel T, Balachandran A, Devine C, Lal C, Bhosale PR. Imaging in endometrial carcinoma. Indian J Radiol Imaging. 2015; 25:137–47.
Article10. Li M, Zhao L, Qi W, et al. Clinical implications and prognostic value of five biomarkers in endometrial carcinoma. Chin Ger J Clin Oncol. 2013; 12:586–91.
Article11. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009; 105:103–4.
Article12. Arafa M, Boniver J, Delvenne P. Progression model tissue microarray (TMA) for the study of uterine carcinomas. Dis Markers. 2010; 28:267–72.
Article13. Zannoni GF, Vellone VG, Arena V, et al. Does high-grade endometrioid carcinoma (grade 3 FIGO) belong to type I or type II endometrial cancer? A clinical-pathological and immunohistochemical study. Virchows Arch. 2010; 457:27–34.
Article14. Kounelis S, Kapranos N, Kouri E, Coppola D, Papadaki H, Jones MW. Immunohistochemical profile of endometrial adenocarcinoma: a study of 61 cases and review of the literature. Mod Pathol. 2000; 13:379–88.
Article15. Brunelli M, Manfrin E, Martignoni G, et al. HER-2/neu assessment in breast cancer using the original FDA and new ASCO/CAP guideline recommendations: impact on selecting patients for herceptin therapy. Am J Clin Pathol. 2008; 129:907–11.16. Binder PS, Mutch DG. Update on prognostic markers for endometrial cancer. Womens Health (Lond). 2014; 10:277–88.
Article17. Rutgers JK. Update on pathology, staging and molecular pathology of endometrial (uterine corpus) adenocarcinoma. Future Oncol. 2015; 11:3207–18.
Article18. Maiques O, Cuevas D, Garcia Dios DA, et al. FISH analysis of PTEN in endometrial carcinoma. Comparison with SNP arrays and MLPA. Histopathology. 2014; 65:371–88.19. Garg K, Soslow RA. Strategies for distinguishing low-grade endometrioid and serous carcinomas of endometrium. Adv Anat Pathol. 2012; 19:1–10.
Article20. Koh WJ, Greer BE, Abu-Rustum NR, et al. Uterine neoplasms, version 1.2014. J Natl Compr Canc Netw. 2014; 12:248–80.21. Ferrandina G, Ranelletti FO, Gallotta V, et al. Expression of cyclooxygenase-2 (COX-2), receptors for estrogen (ER), and progesterone (PR), p53, ki67, and neu protein in endometrial cancer. Gynecol Oncol. 2005; 98:383–9.
Article22. Jazaeri AA, Nunes KJ, Dalton MS, Xu M, Shupnik MA, Rice LW. Well-differentiated endometrial adenocarcinomas and poorly differentiated mixed mullerian tumors have altered ER and PR isoform expression. Oncogene. 2001; 20:6965–9.
Article23. Zhang Y, Zhao D, Gong C, et al. Prognostic role of hormone receptors in endometrial cancer: a systematic review and meta-analysis. World J Surg Oncol. 2015; 13:208.
Article24. Engelsen IB, Stefansson IM, Akslen LA, Salvesen HB. GATA3 expression in estrogen receptor alpha-negative endometrial carcinomas identifies aggressive tumors with high proliferation and poor patient survival. Am J Obstet Gynecol. 2008; 199:543.e1–7.25. Tomica D, Ramic S, Danolic D, et al. A correlation between the expression of estrogen receptors and progesterone receptors in cancer cells and in the myometrium and prognostic factors in endometrial cancer. Coll Antropol. 2014; 38:129–34.26. Srijaipracharoen S, Tangjitgamol S, Tanvanich S, et al. Expression of ER, PR, and Her-2/neu in endometrial cancer: a clinicopathological study. Asian Pac J Cancer Prev. 2010; 11:215–20.27. Sivridis E, Giatromanolaki A, Koukourakis M, Anastasiadis P. Endometrial carcinoma: association of steroid hormone receptor expression with low angiogenesis and bcl-2 expression. Virchows Arch. 2001; 438:470–7.
Article28. Kobel M, Atenafu EG, Rambau PF, et al. Progesterone receptor expression is associated with longer overall survival within highgrade histotypes of endometrial carcinoma: a Canadian high risk endometrial cancer consortium (CHREC) study. Gynecol Oncol. 2016; 141:559–63.29. Stoian SC, Simionescu C, Margaritescu C, Stepan A, Nurciu M. Endometrial carcinomas: correlation between ER, PR, Ki67 status and histopathological prognostic parameters. Rom J Morphol Embryol. 2011; 52:631–6.30. Morrison C, Zanagnolo V, Ramirez N, et al. HER-2 is an independent prognostic factor in endometrial cancer: association with outcome in a large cohort of surgically staged patients. J Clin Oncol. 2006; 24:2376–85.
Article31. Ioffe OB, Papadimitriou JC, Drachenberg CB. Correlation of proliferation indices, apoptosis, and related oncogene expression (bcl-2 and c-erbB-2) and p53 in proliferative, hyperplastic, and malignant endometrium. Hum Pathol. 1998; 29:1150–9.
Article32. Williams JA Jr, Wang ZR, Parrish RS, Hazlett LJ, Smith ST, Young SR. Fluorescence in situ hybridization analysis of HER-2/neu, cmyc, and p53 in endometrial cancer. Exp Mol Pathol. 1999; 67:135–43.
Article33. Gul AE, Keser SH, Barisik NO, et al. The relationship of cerb B 2 expression with estrogen receptor and progesterone receptor and prognostic parameters in endometrial carcinomas. Diagn Pathol. 2010; 5:13.
Article34. Salvesen HB, Iversen OE, Akslen LA. Prognostic significance of angiogenesis and Ki-67, p53, and p21 expression: a populationbased endometrial carcinoma study. J Clin Oncol. 1999; 17:1382–90.
Article35. Geisler JP, Geisler HE, Miller GA, Wiemann MC, Zhou Z, Crabtree W. MIB-1 in endometrial carcinoma: prognostic significance with 5-year follow-up. Gynecol Oncol. 1999; 75:432–6.
Article36. Pansare V, Munkarah AR, Schimp V, et al. Increased expression of hypoxia-inducible factor 1alpha in type I and type II endometrial carcinomas. Mod Pathol. 2007; 20:35–43.37. Goebel EA, Vidal A, Matias-Guiu X, Blake Gilks C. The evolution of endometrial carcinoma classification through application of immunohistochemistry and molecular diagnostics: past, present and future. Virchows Arch. 2018; 472:885–96.
Article38. Sundar S, Balega J, Crosbie E, et al. BGCS uterine cancer guidelines: Recommendations for practice. Eur J Obstet Gynecol Reprod Biol. 2017; 213:71–97.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation between the overexpression of epidermal growth factor receptor and mesenchymal makers in endometrial carcinoma
- A Case of Recurrent Endometrial Carcinoma at the Vagina
- Present status and future direction of clinical trials in advanced endometrial carcinoma
- Distinction of Pulmonary Large Cell Neuroendocrine Carcinoma from Small Cell Lung Carcinoma Using a Panel of Bcl-2, p63, and 34betaE12
- Bcl-2 Expression in Endometrial Hyperplasia and Carcinoma