Anesth Pain Med.
2019 Apr;14(2):141-151. 10.17085/apm.2019.14.2.141.
Effect of intravenous tranexamic acid on perioperative bleeding and transfusion in spine surgery: systematic review and meta-analysis of randomized controlled trials
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. s2248@paik.ac.kr
- KMID: 2447961
- DOI: http://doi.org/10.17085/apm.2019.14.2.141
Abstract
- BACKGROUND
This study aimed to systematically review the literature investigating the effect of intravenous (IV) tranexamic acid (TXA) on the perioperative blood loss and amount of transfused blood in patients who underwent spine surgery under general anesthesia.
METHODS
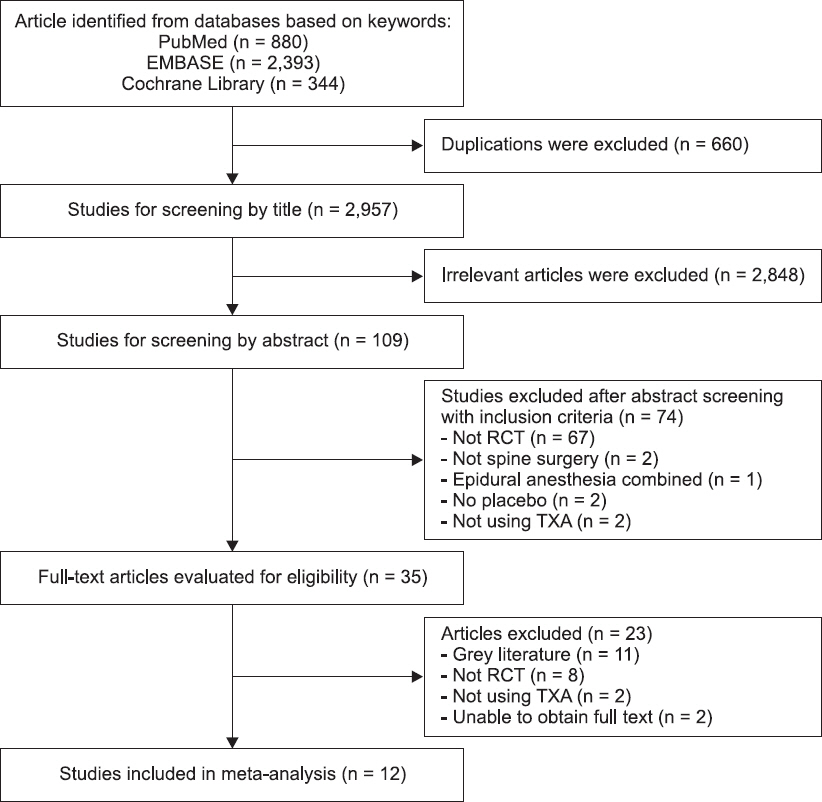
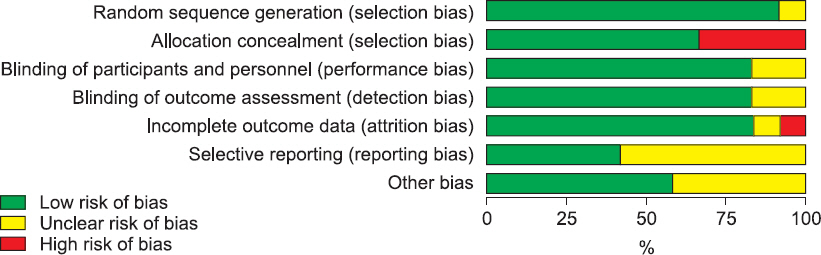
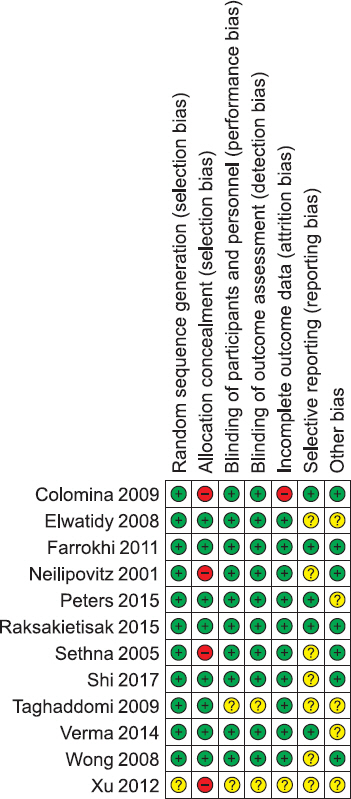
MEDLINE, EMBASE, and CENTRAL databases were searched for studies published up to June 2017. Randomized controlled trials comparing the intervention of tranexamic acid use with a placebo in corrective spine fusion surgery were included. Outcome measures included intraoperative and postoperative blood loss and perioperative blood transfusion volume. We also conducted subgroup analyses according to the dose of administration of intervention drug.
RESULTS
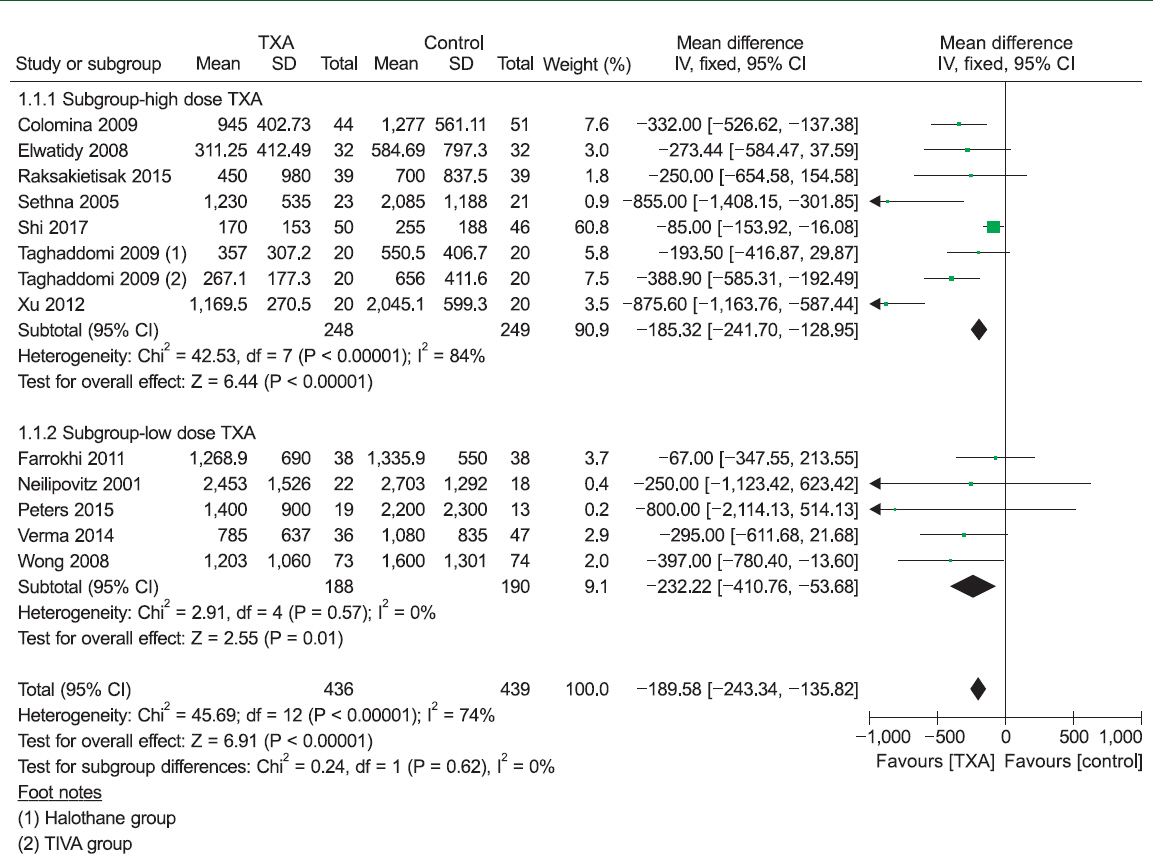
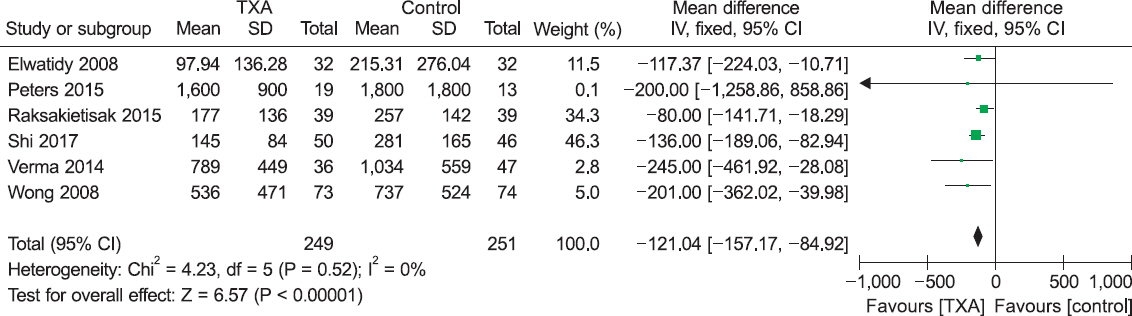
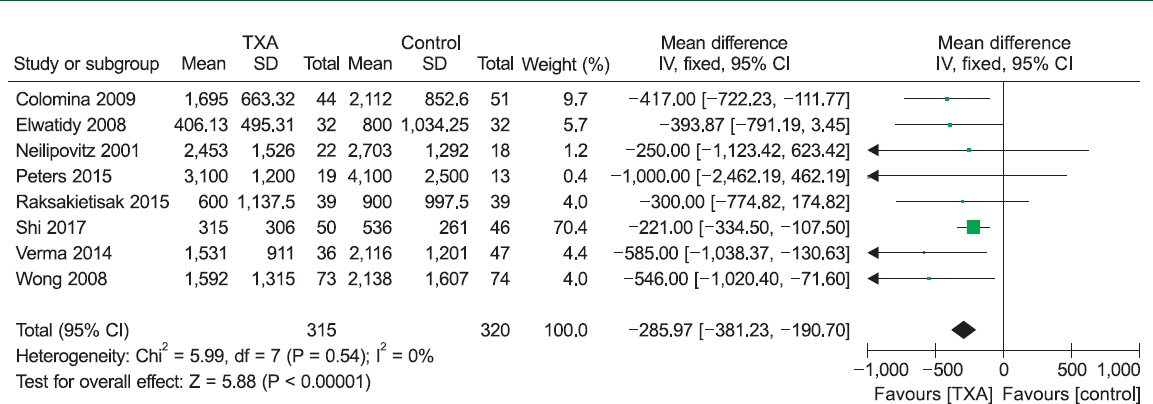
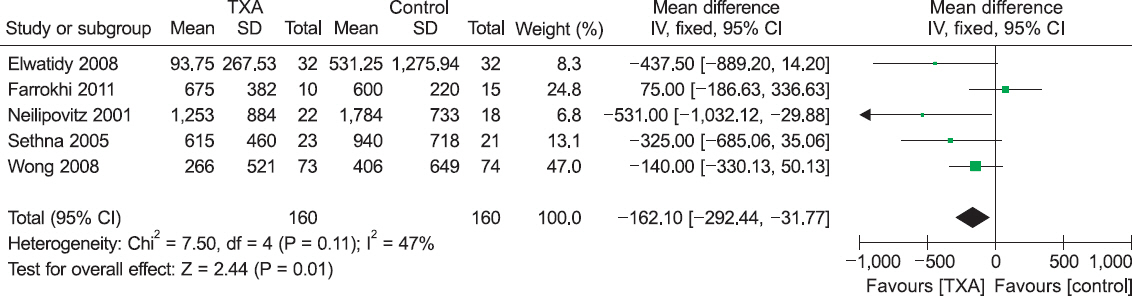
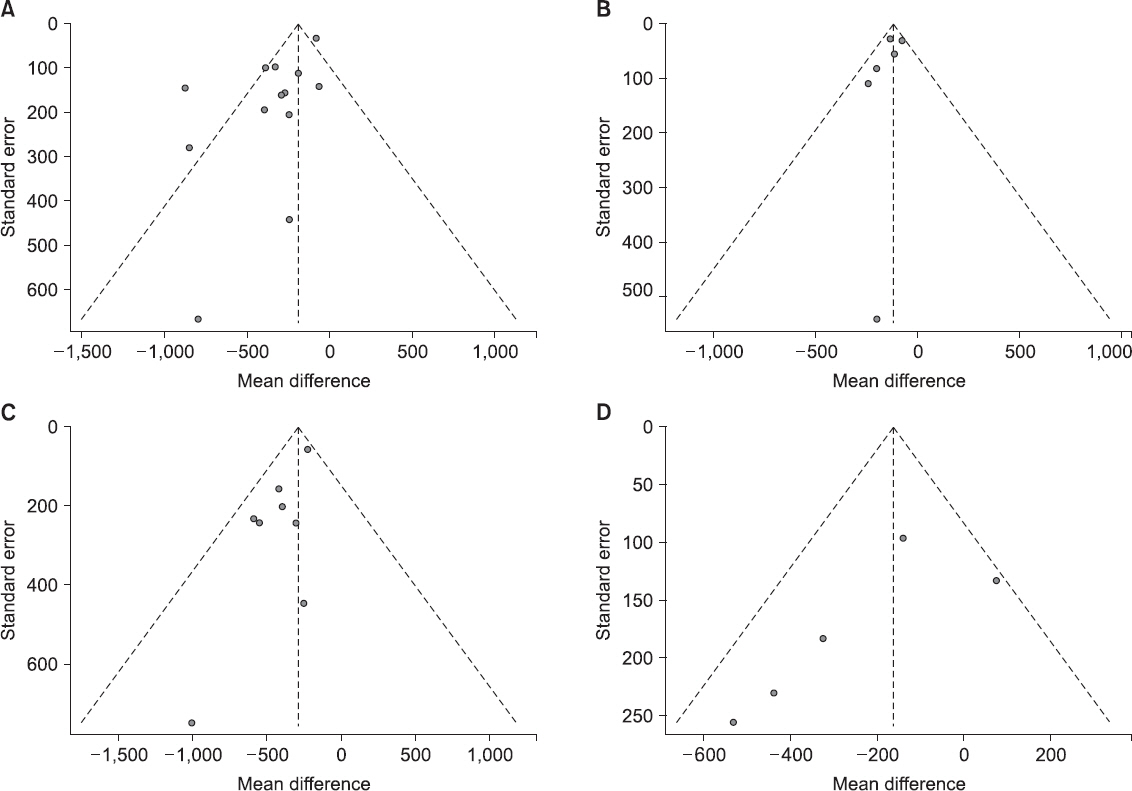
In total, 12 studies involving 875 patients were included in the final analysis. Blood loss decreased in patients treated with perioperative IV TXA by a mean volume of 189.58 ml intraoperatively (95% confidence interval [CI]: 135.82 to 243.34 ml, P < 0.001; I² = 74%), 121.04 ml postoperatively (95% CI: 84.92 to 157.17 ml, P < 0.001; I² = 0%), and 285.97 ml in total (95% CI: 190.70 to 381.23 ml, P < 0.001; I² = 0%). Perioperative transfusion volume also decreased by 162.10 ml in patients who received IV TXA (95% CI: 31.77 to 292.44 ml, P = 0.010; I² = 47%).
CONCLUSIONS
Blood loss was reduced in patients who were administered TXA during spine surgery. Additionally, the perioperative volume of blood transfusion decreased in patients who received TXA. Further research is required to confirm the optimal dosage and timing of TXA usage.
Keyword
MeSH Terms
Figure
Reference
-
1. Neilipovitz DT, Murto K, Hall L, Barrowman NJ, Splinter WM. A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg. 2001; 93:82–7. DOI: 10.1097/00000539-200107000-00018. PMID: 11429344.2. Sethna NF, Zurakowski D, Brustowicz RM, Bacsik J, Sullivan LJ, Shapiro F. Tranexamic acid reduces intraoperative blood loss in pediatric patients undergoing scoliosis surgery. Anesthesiology. 2005; 102:727–32. DOI: 10.1097/00000542-200504000-00006. PMID: 15791100.3. Wong J, El Beheiry H, Rampersaud YR, Lewis S, Ahn H, De Silva Y, et al. Tranexamic Acid reduces perioperative blood loss in adult patients having spinal fusion surgery. Anesth Analg. 2008; 107:1479–86. DOI: 10.1213/ane.0b013e3181831e44. PMID: 18931202.4. Nuttall GA, Horlocker TT, Santrach PJ, Oliver WC Jr, Dekutoski MB, Bryant S. Predictors of blood transfusions in spinal instrumentation and fusion surgery. Spine (Phila Pa 1976). 2000; 25:596–601. DOI: 10.1097/00007632-200003010-00010.5. Seicean A, Alan N, Seicean S, Neuhauser D, Weil RJ. The effect of blood transfusion on short-term, perioperative outcomes in elective spine surgery. J Clin Neurosci. 2014; 21:1579–85. DOI: 10.1016/j.jocn.2014.03.003. PMID: 24852902.6. Kebaish KM, Awad JN. Spinal epidural hematoma causing acute cauda equina syndrome. Neurosurg Focus. 2004; 16:e1. DOI: 10.3171/foc.2004.16.6.1. PMID: 27782760.7. Sokolowski MJ, Garvey TA, Perl J 2nd, Sokolowski MS, Cho W, Mehbod AA, et al. Prospective study of postoperative lumbar epidural hematoma: incidence and risk factors. Spine (Phila Pa 1976). 2008; 33:108–13. DOI: 10.1097/BRS.0b013e31815e39af. PMID: 18165756.8. Cardone D, Klein AA. Perioperative blood conservation. Eur J Anaesthesiol. 2009; 26:722–9. DOI: 10.1097/EJA.0b013e32832c5280. PMID: 19448549.9. Hardy JF, Bélisle S. Natural and synthetic antifibrinolytics: inert, poisonous or therapeutic agents? Can J Anaesth. 1997; 44:913–7. DOI: 10.1007/BF03011960. PMID: 9305552.10. Huang F, Wu D, Ma G, Yin Z, Wang Q. The use of tranexamic acid to reduce blood loss and transfusion in major orthopedic surgery: a meta-analysis. J Surg Res. 2014; 186:318–27. DOI: 10.1016/j.jss.2013.08.020. PMID: 24075404.11. Yang ZG, Chen WP, Wu LD. Effectiveness and safety of tranexamic acid in reducing blood loss in total knee arthroplasty: a metaanalysis. J Bone Joint Surg Am. 2012; 94:1153–9. DOI: 10.2106/JBJS.K.00873. PMID: 22623147.12. Sukeik M, Alshryda S, Haddad FS, Mason JM. Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg Br. 2011; 93:39–46. DOI: 10.1302/0301-620X.93B1.24984. PMID: 21196541.13. Casati V, Guzzon D, Oppizzi M, Bellotti F, Franco A, Gerli C, et al. Tranexamic acid compared with high-dose aprotinin in primary elective heart operations: effects on perioperative bleeding and allogeneic transfusions. J Thorac Cardiovasc Surg. 2000; 120:5207. DOI: 10.1067/mtc.2000.108016. PMID: 10962414.14. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009; 339:b2535. DOI: 10.1136/bmj.b2535. PMID: 19622551. PMCID: PMC2714657.15. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999; 354:1896–900. DOI: 10.1016/S0140-6736(99)04149-5.16. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration [serial on the Internet]. 2011. Mar [2017 Jun 20]. Available from www.handbook.cochrane.org .17. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5:13. DOI: 10.1186/1471-2288-5-13. PMID: 15840177. PMCID: PMC1097734.18. Elwatidy S, Jamjoom Z, Elgamal E, Zakaria A, Turkistani A, El-Dawlatly A. Efficacy and safety of prophylactic large dose of tranexamic acid in spine surgery: a prospective, randomized, double-blind, placebo-controlled study. Spine (Phila Pa 1976). 2008; 33:2577–80. DOI: 10.1097/BRS.0b013e318188b9c5. PMID: 19011538.19. Raksakietisak M, Sathitkarnmanee B, Srisaen P, Duangrat T, Chinachoti T, Rushatamukayanunt P, et al. Two doses of tranexamic acid reduce blood transfusion in complex spine surgery: a prospective randomized study. Spine (Phila Pa 1976). 2015; 40:E1257–63. DOI: 10.1097/BRS.0000000000001063. PMID: 26208230.20. Xu C, Wu A, Yue Y. Which is more effective in adolescent idiopathic scoliosis surgery: batroxobin, tranexamic acid or a combination? Arch Orthop Trauma Surg. 2012; 132:25–31. DOI: 10.1007/s00402-011-1390-6. PMID: 21909815.21. Colomina MJ, Bagó J, Vidal X, Mora L, Pellisé F. Antifibrinolytic therapy in complex spine surgery: a case-control study comparing aprotinin and tranexamic acid. Orthopedics. 2009; 32:91. PMID: 19301800.22. Taghaddomi RJ, Mashhadinezhad H, Attar ARS, Peyvandi A. The effect of intravenous tranexamic acid on blood loss in lumbar hernial disc resection under inhalation and total intravenous anesthesia. Iran Red Crescent Med J. 2009; 11:265–70.23. Farrokhi MR, Kazemi AP, Eftekharian HR, Akbari K. Efficacy of prophylactic low dose of tranexamic acid in spinal fixation surgery: a randomized clinical trial. J Neurosurg Anesthesiol. 2011; 23:290–6. DOI: 10.1097/ANA.0b013e31822914a1. PMID: 21836528.24. Peters A, Verma K, Slobodyanyuk K, Cheriyan T, Hoelscher C, Schwab F, et al. Antifibrinolytics reduce blood loss in adult spinal deformity surgery: a prospective, randomized controlled trial. Spine (Phila Pa 1976). 2015; 40:E443–9. DOI: 10.1097/BRS.0000000000000799. PMID: 25868100.25. Shi H, Ou Y, Jiang D, Quan Z, Zhao Z, Zhu Y. Tranexamic acid reduces perioperative blood loss of posterior lumbar surgery for stenosis or spondylolisthesis: a randomized trial. Medicine (Baltimore). 2017; 96:e5718. DOI: 10.1097/MD.0000000000005718. PMID: 28072709. PMCID: PMC5228669.26. Verma K, Errico T, Diefenbach C, Hoelscher C, Peters A, Dryer J, et al. The relative efficacy of antifibrinolytics in adolescent idiopathic scoliosis: a prospective randomized trial. J Bone Joint Surg Am. 2014; 96:e80. DOI: 10.2106/JBJS.L.00008. PMID: 24875032.27. Zufferey P, Merquiol F, Laporte S, Decousus H, Mismetti P, Auboyer C, et al. Do antifibrinolytics reduce allogeneic blood transfusion in orthopedic surgery? Anesthesiology. 2006; 105:1034–46. DOI: 10.1097/00000542-200611000-00026. PMID: 17065899.28. Endres S, Heinz M, Wilke A. Efficacy of tranexamic acid in reducing blood loss in posterior lumbar spine surgery for degenerative spinal stenosis with instability: a retrospective case control study. BMC Surg. 2011; 11:29. DOI: 10.1186/1471-2482-11-29. PMID: 22047046. PMCID: PMC3234174.29. Khurana A, Guha A, Saxena N, Pugh S, Ahuja S. Comparison of aprotinin and tranexamic acid in adult scoliosis correction surgery. Eur Spine J. 2012; 21:1121–6. DOI: 10.1007/s00586-012-2205-3. PMID: 22402839. PMCID: PMC3366133.30. Gill JB, Chin Y, Levin A, Feng D. The use of antifibrinolytic agents in spine surgery. A meta-analysis. J Bone Joint Surg Am. 2008; 90:2399–407. DOI: 10.2106/JBJS.G.01179. PMID: 18978408.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tranexamic Acid Versus a Placebo in Decreasing Blood Loss in Patients Undergoing Spine Surgery
- Effect of Tranexamic Acid on Blood Loss and Blood Transfusion Reduction after Total Knee Arthroplasty
- Minimal Dose of Tranexamic Acid Is Effective in Reducing Blood Loss in Complex Spine Surgeries: A Randomized Double-Blind Placebo Controlled Study
- Efficacy of Tranexamic Acid during Primary Total Knee Arthroplasty: Comparative Study between Intravenous Use and Topical Use
- Synergistic Effect of Intraarticular Tranexamic Acid Injection and the Use of Navigation in Total Knee Arthroplasty for Reducing Blood Loss