Clin Endosc.
2019 Mar;52(2):175-181. 10.5946/ce.2018.110.
The Utility of Endoscopic Ultrasound in Patients with Isolated Elevations in Serum Amylase and/or Lipase
- Affiliations
-
- 1Division of Digestive Diseases, Department of Medicine, Columbia University Irving Medical Center, New York, NY, USA. Lalitha.Sitaraman@gmail.com
- 2Division of Digestive and Liver Diseases, Columbia University Irving Medical Center, New York, NY, USA.
- KMID: 2447675
- DOI: http://doi.org/10.5946/ce.2018.110
Abstract
- BACKGROUND/AIMS
The aim of this study was to describe the diagnostic yield of endoscopic ultrasound (EUS) in patients with isolated elevated levels of amylase and/or lipase.
METHODS
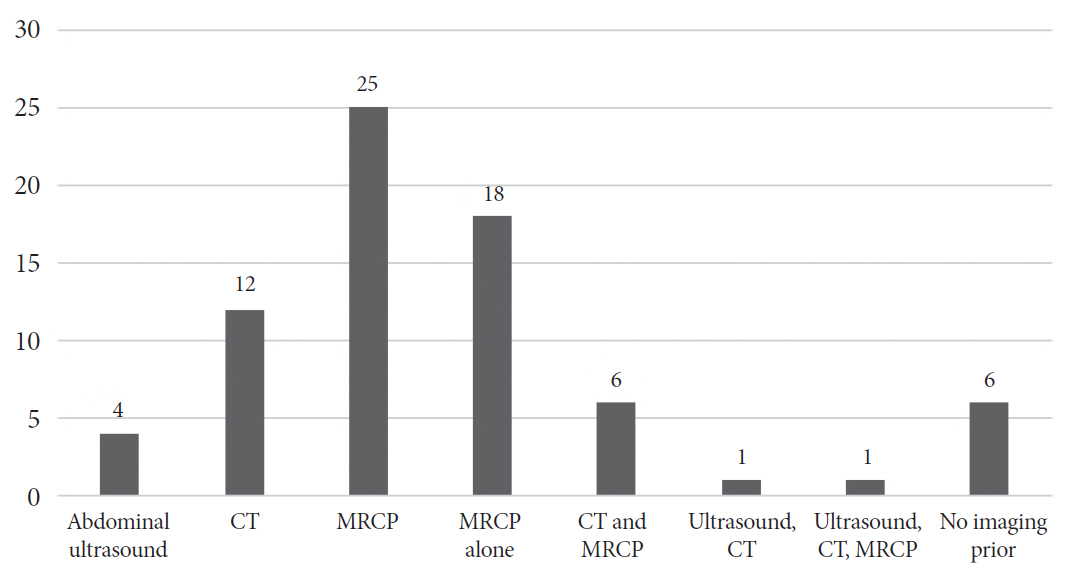
A retrospective chart review was conducted at a large academic medical center from 2000 to 2016. Patients were selected based on having elevated amylase, lipase, or both, but without a diagnosis of pancreatitis or known pancreatobiliary disease. Patients were excluded if they had abnormal liver function tests or abnormal imaging of the pancreas.
RESULTS
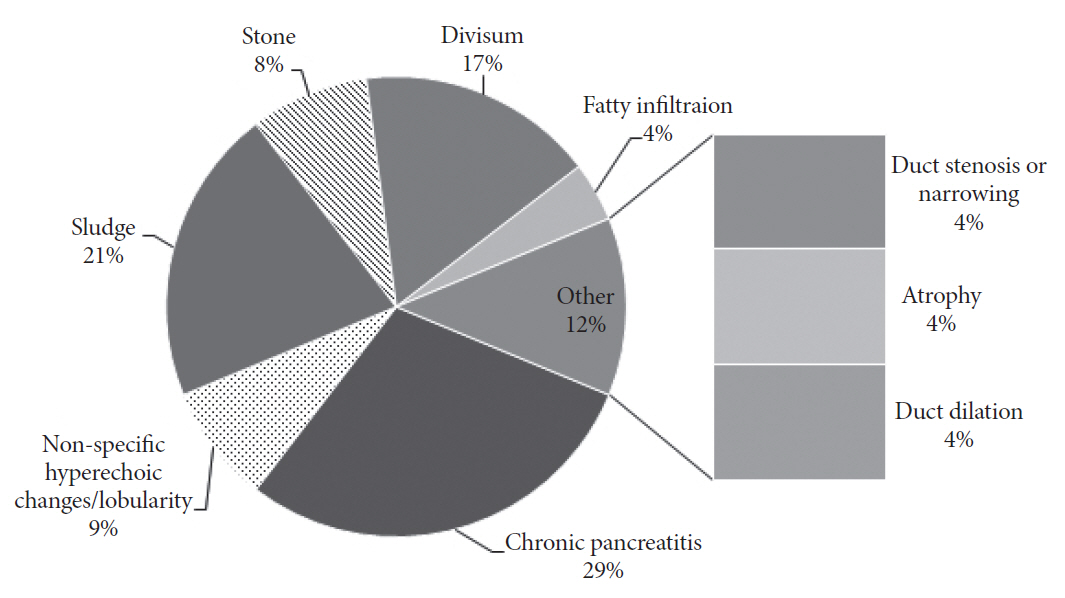
Of 299 EUS procedures performed, 38 met inclusion criteria. Symptoms were present in 31 patients, most frequently abdominal pain (87%). In 20 patients (53%), initial EUS most commonly found chronic pancreatitis (n=7; 18%), sludge (5; 13%), or new diagnosis of pancreas divisum (3; 8%). In the asymptomatic patients (7), 3 had a finding on EUS, most importantly sludge (2), stone (1), and pancreas divisum (1). No patients were diagnosed with a mass or pancreatic cyst. During the follow up period, 6 patients (22%) had cholecystectomy.
CONCLUSIONS
In our study of patients with isolated elevations in amylase and/or lipase without acute pancreatitis who underwent EUS, approximately 50% had a pancreatobiliary finding, most commonly chronic pancreatitis or biliary sludge.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Do Patients with Pancreatic Hyperenzymemia without Abnormal Imaging Need Additional Endoscopic Ultrasound?
Jung Wan Choe, Jong Jin Hyun
Clin Endosc. 2019;52(2):97-99. doi: 10.5946/ce.2019.044.
Reference
-
1. Muniraj T, Dang S, Pitchumoni CS. Pancreatitis or not?--elevated lipase and amylase in ICU patients. J Crit Care. 2015; 30:1370–1375.2. Frulloni L, Patrizi F, Bernardoni L, Cavallini G. Pancreatic hyperenzymemia: clinical significance and diagnostic approach. JOP. 2005; 6:536–551.3. Vonlaufen A, Wilson JS, Apte MV. Molecular mechanisms of pancreatitis: current opinion. J Gastroenterol Hepatol. 2008; 23:1339–1348.
Article4. Warshaw AL, Lee KH. Macroamylasemia and other chronic nonspecific hyperamylasemias: chemical oddities or clinical entities? Am J Surg. 1978; 135:488–493.
Article5. Gullo L. Chronic nonpathological hyperamylasemia of pancreatic origin. Gastroenterology. 1996; 110:1905–1908.
Article6. Gullo L. Benign pancreatic hyperenzymemia. Dig Liver Dis. 2007; 39:698–702.
Article7. Catalano MF, Sahai A, Levy M, et al. EUS-based criteria for the diagnosis of chronic pancreatitis: the Rosemont classification. Gastrointest Endosc. 2009; 69:1251–1261.
Article8. Ito T. Can measurement of chemokines become useful biological and functional markers of early-stage chronic pancreatitis? J Gastroenterol. 2007; 42 Suppl 17:72–77.
Article9. Stevens T, Conwell DL, Zuccaro G. Pathogenesis of chronic pancreatitis: an evidence-based review of past theories and recent developments. Am J Gastroenterol. 2004; 99:2256–2270.
Article10. Duggan SN. Negotiating the complexities of exocrine and endocrine dysfunction in chronic pancreatitis. Proc Nutr Soc. 2017; 76:484–494.
Article11. Duggan SN, Ni Chonchubhair HM, Lawal O, O’Connor DB, Conlon KC. Chronic pancreatitis: a diagnostic dilemma. World J Gastroenterol. 2016; 22:2304–2313.
Article12. Conwell DL, Lee LS, Yadav D, et al. American pancreatic association practice guidelines in chronic pancreatitis: evidence-based report on diagnostic guidelines. Pancreas. 2014; 43:1143–1162.13. Yadav D, Timmons L, Benson JT, Dierkhising RA, Chari ST. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am J Gastroenterol. 2011; 106:2192–2199.
Article14. Cotton PB. Congenital anomaly of pancreas divisum as cause of obstructive pain and pancreatitis. Gut. 1980; 21:105–114.
Article15. DiMagno MJ, Wamsteker EJ. Pancreas divisum. Curr Gastroenterol Rep. 2011; 13:150–156.
Article16. Adike A, El Kurdi BI, Gaddam S, et al. Pancreatitis in patients with pancreas divisum. Pancreas. 2017; 46:e80–e81.
Article17. Burtin P, Person B, Charneau J, Boyer J. Pancreas divisum and pancreatitis: a coincidental association? Endoscopy. 1991; 23:55–58.
Article18. Di Leo M, Petrone MC, Zuppardo RA, et al. Pancreatic morpho-functional imaging as a diagnostic approach for chronic asymptomatic pancreatic hyperenzymemia. Dig Liver Dis. 2016; 48:1330–1335.
Article19. Amodio A, Manfredi R, Katsotourchi AM, et al. Prospective evaluation of subjects with chronic asymptomatic pancreatic hyperenzymemia. Am J Gastroenterol. 2012; 107:1089–1095.
Article20. Berk JE, Kizu H, Wilding P, Searcy RL. Macroamylasemia: a newly recognized cause for elevated serum amylase activity. N Engl J Med. 1967; 277:941–946.21. Völzke H, Lüdemann J, Mayerle J, Kraft M, John U, Lerch MM. Prevalence and determinants of increased serum lipase levels in a general population. Pancreas. 2008; 37:411–417.
Article22. Sharma A, Masood U, Khan B, Chawla K, Manocha D. Pancreatitis with normal lipase and amylase in setting of end-stage renal disease. Am J Emerg Med. 2017; 35:1387.e3–1387.e4.
Article23. Ustohal L, Mayerova M, Valkova B, Sedlakova H, Kasparek T. Asymptomatic elevation of amylase and lipase after olanzapine treatment. J Clin Psychopharmacol. 2016; 36:181–183.
Article24. Szoke D, Ridolfo A, Valente C, Galli M, Panteghini M. Frequency of pancreatic hyperamylasemia in human immunodeficiency virus-positive patients in the highly active antiretroviral therapy era. Am J Clin Pathol. 2016; 145:128–133.
Article25. Pezzilli R. Alcohol abuse and pancreatic diseases: an overview. Recent Pat Inflamm Allergy Drug Discov. 2015; 9:102–106.
Article26. Saumoy M, Kahaleh M. Safety and complications of interventional endoscopic ultrasound. Clin Endosc. 2018; 51:235–238.
Article27. Das A, Sivak MV Jr, Chak A. Cervical esophageal perforation during EUS: a national survey. Gastrointest Endosc. 2001; 53:599–602.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Systematic Approach to Patients with Elevated Levels of Serum Amylase or Lipase
- Changing patterns of Pancreatic enzyme after Distal Gastrectomy and the Effect of Protease Inhibitor Treatment
- Pancreatic Enzyme Elevations in Korean Chronic Renal Failure Patients
- Evaluation of the Clinical Usefulness for Pancreatic Amylase in Acute Pancreatitis
- Usefulness of Lipase Test for the Diagnosis of Acute Pancreatitis