Clin Endosc.
2019 Mar;52(2):152-158. 10.5946/ce.2018.125.
Predictive Factors for Inaccurate Diagnosis of Swollen Lymph Nodes in Endoscopic Ultrasound-Guided Fine Needle Aspiration
- Affiliations
-
- 1Department of Gastroenterology, Sendai City Medical Center, Sendai, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan. y_f1105@yahoo.co.jp
- 2Department of Gastroenterology and Hepatology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan.
- KMID: 2447672
- DOI: http://doi.org/10.5946/ce.2018.125
Abstract
- BACKGROUND/AIMS
This study aimed to identify the predictive factors for inaccurate endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) diagnosis of swollen lymph nodes without rapid on-site cytopathological evaluation.
METHODS
Eighty-three consecutive patients who underwent EUS-FNA for abdominal or mediastinal lymph nodes from January 2008 to June 2017 were included from a prospectively maintained EUS-FNA database and retrospectively reviewed. The sensitivity, specificity, and accuracy of EUS-FNA for the detection of neoplastic diseases were calculated. Candidate factors for inaccurate diagnosis (lymph node size and location, needle type, puncture route, number of passes, and causative disease) were evaluated by comparison between accurately diagnosed cases and others.
RESULTS
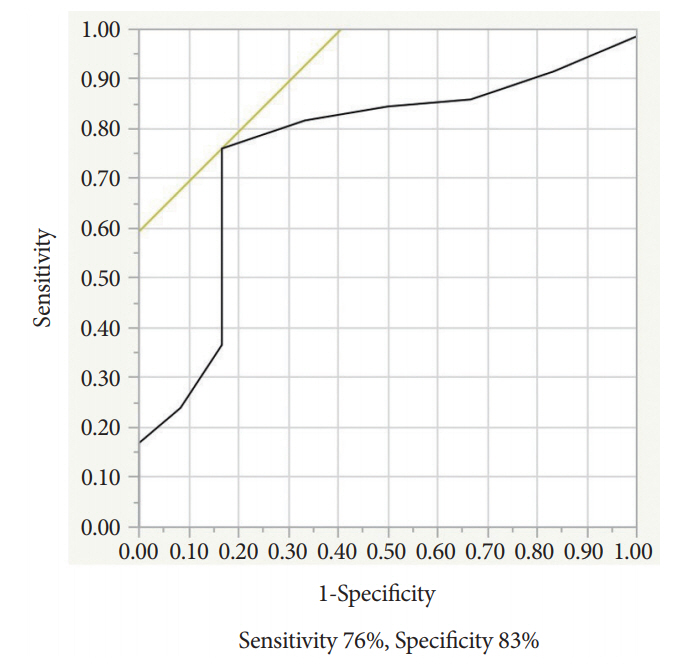
The final diagnosis of the punctured lymph node was classified as neoplastic (65 cases: a metastatic lymph node, malignant lymphoma, or Crow-Fukase syndrome) or non-neoplastic (18 cases: a reactive node or amyloidosis). The sensitivity, specificity, and accuracy were 83%, 94%, and 86%, respectively. On multivariate analyses, small size of the lymph node was the sole predictive factor for inaccurate EUS-FNA diagnosis with a significant difference (odds ratios, 19.8; 95% confidence intervals, 3.15-124; p=0.0015).
CONCLUSIONS
The lymph node size of <16 mm was the only independent factor associated with inaccurate EUS-FNA diagnosis of swollen lymph nodes.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
How to Improve the Diagnostic Accuracy of EUS-FNA in Abdominal and Mediastinal Lymphadenopathy?
Tae Hyeon Kim
Clin Endosc. 2019;52(2):93-94. doi: 10.5946/ce.2019.048.
Reference
-
1. Wiersema MJ, Hawes RH, Tao LC, et al. Endoscopic ultrasonography as an adjunct to fine needle aspiration cytology of the upper and lower gastrointestinal tract. Gastrointest Endosc. 1992; 38:35–39.
Article2. Ardengh JC, Bammann RH, Giovani M, Venco F, Parada AA. Endoscopic ultrasound-guided biopsies for mediastinal lesions and lymph node diagnosis and staging. Clinics (Sao Paulo). 2011; 66:1579–1583.
Article3. Akahoshi K, Oya M, Koga T, et al. Clinical usefulness of endoscopic ultrasound-guided fine needle aspiration for gastric subepithelial lesions smaller than 2 cm. J Gastrointestin Liver Dis. 2014; 23:405–412.
Article4. Eckardt AJ, Jenssen C. Current endoscopic ultrasound-guided approach to incidental subepithelial lesions: optimal or optional? Ann Gastroenterol. 2015; 28:160–172.5. Mekky MA, Yamao K, Sawaki A, et al. Diagnostic utility of EUS-guided FNA in patients with gastric submucosal tumors. Gastrointest Endosc. 2010; 71:913–919.
Article6. Kaushik N, Khalid A, Brody D, McGrath K. EUS-guided paracentesis for the diagnosis of malignant ascites. Gastrointest Endosc. 2006; 64:908–913.
Article7. DeWitt J, Yu M, Al-Haddad MA, Sherman S, McHenry L, Leblanc JK. Survival in patients with pancreatic cancer after the diagnosis of malignant ascites or liver metastases by EUS-FNA. Gastrointest Endosc. 2010; 71:260–265.
Article8. DeWitt J, LeBlanc J, McHenry L, McGreevy K, Sherman S. Endoscopic ultrasound-guided fine-needle aspiration of ascites. Clin Gastroenterol Hepatol. 2007; 5:609–615.
Article9. Weilert F, Bhat YM, Binmoeller KF, et al. EUS-FNA is superior to ERCP-based tissue sampling in suspected malignant biliary obstruction: results of a prospective, single-blind, comparative study. Gastrointest Endosc. 2014; 80:97–104.
Article10. Kim HJ, Lee SK, Jang JW, et al. Diagnostic role of endoscopic ultrasonography-guided fine needle aspiration of gallbladder lesions. Hepatogastroenterology. 2012; 59:1691–1695.
Article11. Hijioka S, Hara K, Mizuno N, et al. Diagnostic yield of endoscopic retrograde cholangiography and of EUS-guided fine needle aspiration sampling in gallbladder carcinomas. J Hepatobiliary Pancreat Sci. 2012; 19:650–655.
Article12. Ogura T, Kurisu Y, Masuda D, et al. Can endoscopic ultrasound-guided fine needle aspiration offer clinical benefit for thick-walled gallbladders? Dig Dis Sci. 2014; 59:1917–1924.
Article13. Yasuda I, Tsurumi H, Omar S, et al. Endoscopic ultrasound-guided fine-needle aspiration biopsy for lymphadenopathy of unknown origin. Endoscopy. 2006; 38:919–924.
Article14. Nakahara O, Yamao K, Bhatia V, et al. Usefulness of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) for undiagnosed intra-abdominal lymphadenopathy. J Gastroenterol. 2009; 44:562–567.
Article15. Naini BV, Apple SK, Presley M, Moatamed NA. A correlation study on diagnostic endoscopic ultrasound-guided fine-needle aspiration of lymph nodes with histological and clinical diagnoses, the UCLA Medical Center experience. Diagn Cytopathol. 2008; 36:460–466.
Article16. Kurita A, Kodama Y, Nakamoto Y, et al. Impact of EUS-FNA for preoperative para-aortic lymph node staging in patients with pancreatobiliary cancer. Gastrointest Endosc. 2016; 84:467–475.e1.
Article17. Korenblit J, Anantharaman A, Loren DE, Kowalski TE, Siddiqui AA. The role of endoscopic ultrasound-guided fine needle aspiration (eusfna) for the diagnosis of intra-abdominal lymphadenopathy of unknown origin. J Interv Gastroenterol. 2012; 2:172–176.
Article18. Lee YN, Moon JH, Kim HK, et al. A triple approach for diagnostic assessment of endoscopic ultrasound-guided fine needle aspiration in pancreatic solid masses and lymph nodes. Dig Dis Sci. 2014; 59:2286–2293.
Article19. Iwashita T, Yasuda I, Doi S, et al. Endoscopic ultrasound-guided fine-needle aspiration in patients with lymphadenopathy suspected of recurrent malignancy after curative treatment. J Gastroenterol. 2009; 44:190–196.
Article20. Chen J, Yang R, Lu Y, Xia Y, Zhou H. Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration for solid pancreatic lesion: a systematic review. J Cancer Res Clin Oncol. 2012; 138:1433–1441.
Article21. Puli SR, Bechtold ML, Buxbaum JL, Eloubeidi MA. How good is endoscopic ultrasound-guided fine-needle aspiration in diagnosing the correct etiology for a solid pancreatic mass?: a meta-analysis and systematic review. Pancreas. 2013; 42:20–26.22. Banafea O, Mghanga FP, Zhao J, Zhao R, Zhu L. Endoscopic ultrasonography with fine-needle aspiration for histological diagnosis of solid pancreatic masses: a meta-analysis of diagnostic accuracy studies. BMC Gastroenterol. 2016; 16:108.
Article23. Savides TJ. Tricks for improving EUS-FNA accuracy and maximizing cellular yield. Gastrointest Endosc. 2009; 69(2 Suppl):S130–S133.
Article24. Matynia AP, Schmidt RL, Barraza G, Layfield LJ, Siddiqui AA, Adler DG. Impact of rapid on-site evaluation on the adequacy of endoscopic-ultrasound guided fine-needle aspiration of solid pancreatic lesions: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2014; 29:697–705.
Article25. Hébert-Magee S, Bae S, Varadarajulu S, et al. The presence of a cytopathologist increases the diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration cytology for pancreatic adenocarcinoma: a meta-analysis. Cytopathology. 2013; 24:159–171.
Article26. Cleveland P, Gill KR, Coe SG, et al. An evaluation of risk factors for inadequate cytology in EUS-guided FNA of pancreatic tumors and lymph nodes. Gastrointest Endosc. 2010; 71:1194–1199.
Article27. Kappelle WFW, Van Leerdam ME, Schwartz MP, et al. Rapid on-site evaluation during endoscopic ultrasound-guided fine-needle aspiration of lymph nodes does not increase diagnostic yield: a randomized, multicenter trial. Am J Gastroenterol. 2018; 113:677–685.
Article28. Noda Y, Fujita N, Kobayashi G, et al. Diagnostic efficacy of the cell block method in comparison with smear cytology of tissue samples obtained by endoscopic ultrasound-guided fine-needle aspiration. J Gastroenterol. 2010; 45:868–875.
Article29. LeBlanc JK, Ciaccia D, Al-Assi MT, et al. Optimal number of EUS-guided fine needle passes needed to obtain a correct diagnosis. Gastrointest Endosc. 2004; 59:475–481.
Article30. Wallace MB, Kennedy T, Durkalski V, et al. Randomized controlled trial of EUS-guided fine needle aspiration techniques for the detection of malignant lymphadenopathy. Gastrointest Endosc. 2001; 54:441–447.
Article31. Pellisé Urquiza M, Fernández-Esparrach G, Solé M, et al. Endoscopic ultrasound-guided fine needle aspiration: predictive factors of accurate diagnosis and cost-minimization analysis of on-site pathologist. Gastroenterol Hepatol. 2007; 30:319–324.
Article32. Chin YK, Iglesias-Garcia J, de la Iglesia D, et al. Accuracy of endoscopic ultrasound-guided tissue acquisition in the evaluation of lymph nodes enlargement in the absence of on-site pathologist. World J Gastroenterol. 2017; 23:5755–5763.
Article33. Klapman JB, Logrono R, Dye CE, Waxman I. Clinical impact of onsite cytopathology interpretation on endoscopic ultrasound-guided fine needle aspiration. Am J Gastroenterol. 2003; 98:1289–1294.
Article34. Jhala NC, Jhala D, Eltoum I, et al. Endoscopic ultrasound-guided fine-needle aspiration biopsy: a powerful tool to obtain samples from small lesions. Cancer. 2004; 102:239–246.
Article35. Alsohaibani F, Girgis S, Sandha GS. Does onsite cytotechnology evaluation improve the accuracy of endoscopic ultrasound-guided fine-needle aspiration biopsy? Can J Gastroenterol. 2009; 23:26–30.
Article36. Jeong SH, Yoon HH, Kim EJ, Kim YJ, Kim YS, Cho JH. High-resolution endoscopic ultrasound imaging and the number of needle passages are significant factors predicting high yield of endoscopic ultrasound-guided fine needle aspiration for pancreatic solid masses without an on-site cytopathologist. Medicine (Baltimore). 2017; 96:e5782.
Article37. Ribeiro A, Vazquez-Sequeiros E, Wiersema LM, Wang KK, Clain JE, Wiersema MJ. EUS-guided fine-needle aspiration combined with flow cytometry and immunocytochemistry in the diagnosis of lymphoma. Gastrointest Endosc. 2001; 53:485–491.
Article38. Faries MB, Bedrosian I, Reynolds C, Nguyen HQ, Alavi A, Czerniecki BJ. Active macromolecule uptake by lymph node antigen-presenting cells: a novel mechanism in determining sentinel lymph node status. Ann Surg Oncol. 2000; 7:98–105.
Article39. Carter BA, Jensen RA, Simpson JF, Page DL. Benign transport of breast epithelium into axillary lymph nodes after biopsy. Am J Clin Pathol. 2000; 113:259–265.
Article40. Hartveit F. Micrometastases to the axilla in breast cancer: their size and season of presentation. Invasion Metastasis. 1996; 16:144–149.41. Wiersema MJ, Hassig WM, Hawes RH, Wonn MJ. Mediastinal lymph node detection with endosonography. Gastrointest Endosc. 1993; 39:788–793.
Article42. Catalano MF, Sivak MV Jr, Rice T, Gragg LA, Van Dam J. Endosonographic features predictive of lymph node metastasis. Gastrointest Endosc. 1994; 40:442–446.
Article43. Bhutani MS, Hawes RH, Hoffman BJ. A comparison of the accuracy of echo features during endoscopic ultrasound (EUS) and EUS-guided fine-needle aspiration for diagnosis of malignant lymph node invasion. Gastrointest Endosc. 1997; 45:474–479.
Article44. Choudhary NS, Bodh V, Kumar N, et al. Yield of endoscopic ultrasound-guided fine needle aspiration for subcentimetric lymph nodes: a comparison to larger nodes. Endosc Ultrasound. 2017; 6:168–173.
Article45. Sazuka T, Akai T, Uesato M, et al. Assessment for diagnosis of lymph node metastasis in esophageal cancer using endoscopic ultrasound elastography. Esophagus. 2016; 13:254–263.
Article46. Rubaltelli L, Khadivi Y, Tregnaghi A, et al. Evaluation of lymph node perfusion using continuous mode harmonic ultrasonography with a second-generation contrast agent. J Ultrasound Med. 2004; 23:829–836.
Article47. Hocke M, Ignee A, Dietrich C. Role of contrast-enhanced endoscopic ultrasound in lymph nodes. Endosc Ultrasound. 2017; 6:4–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Ultrasound-Guided Fine Needle Aspiration in Breast Lesions
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?
- Endoscopic Ultrasound-Fine Needle Aspiration versus Core Biopsy for the Diagnosis of Subepithelial Tumors
- How Can We Get the Best Results with Endoscopic Ultrasound-Guided Fine Needle Aspiration?
- The Role of EBUS-TBNA in the Diagnosis and Staging of Lung Cancer