Investig Clin Urol.
2019 May;60(3):176-183. 10.4111/icu.2019.60.3.176.
Neutrophil-to-lymphocyte ratio independently predicts advanced pathological staging and poorer survival outcomes in testicular cancer
- Affiliations
-
- 1Department of Urology, Singapore General Hospital, Singapore. yuguangtan90@gmail.com
- KMID: 2444272
- DOI: http://doi.org/10.4111/icu.2019.60.3.176
Abstract
- PURPOSE
An elevated neutrophil-to-lymphocyte ratio (NLR) has been associated with adverse outcomes in various malignancies. However, its role in prognosticating testicular cancer (TC) has not been validated. We aim to study the relationship between NLR and TC.
MATERIALS AND METHODS
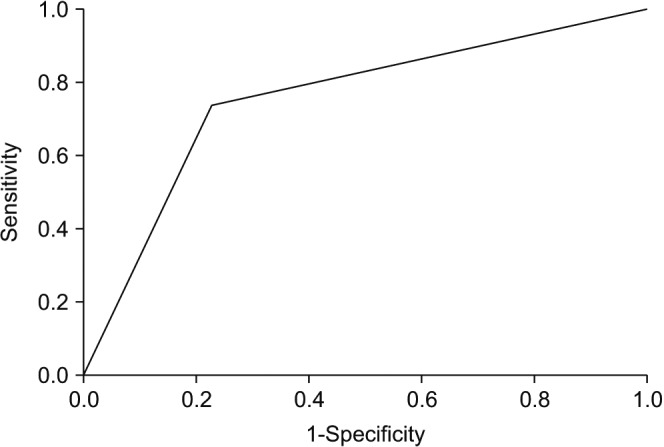
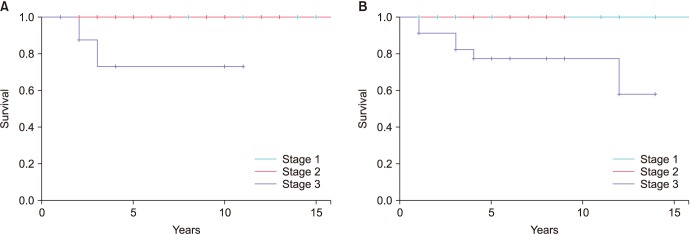
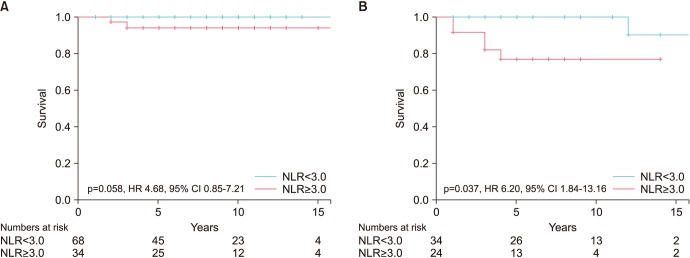
We retrospectively reviewed 160 patients with histological proven TC from January 2005 to June 2016. Youden's index was used to analyse NLR and a cut-off point of 3.0 was obtained, with statistical receiver operating characteristics of 0.755. Chi-square test, Kaplan-Meier (log rank test) and logistics regression models were used to predict NLR association with survival outcomes.
RESULTS
Median age was 34 years old (range, 17-68 years old). There were 102 pure seminomas and 58 non-seminomatous germ cell tumours. Median follow-up period was 8 years (range, 2.5-17 years). NLR ≥3.0 was independently associated with lymph node involvement (p=0.031; odds ratio [OR], 2.91; 95% confidence interval [CI], 1.67-5.83; p=0.038; OR, 4.12; 95% CI, 1.26-6.51) and metastatic disease (p=0.041; OR, 2.48; 95% CI, 1.22-3.98; p=0.043; OR, 2.21; 95% CI, 1.17-3.65) in both seminomatous and non-seminomatous germ cell tumours, translating to a more advanced disease. Moreover, NLR ≥3.0 also predicts poorer cancer specific survival in these patients.
CONCLUSIONS
NLR can be an inexpensive haematological marker in predicting advanced TC staging and poorer survival outcome. NLR complements the traditional cancer staging by identifying a group of high risk patients who may benefit from multimodal treatment and closer surveillance to achieve long term survival.
Keyword
MeSH Terms
Figure
Reference
-
1. Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013; 49:1374–1403. PMID: 23485231.
Article2. National Cancer Institute, Surveillance, Epidemiology, and End Results Program. Cancer stat facts: testicular cancer [Internet]. National Institutes of Health;updated 2017 Nov. cited 2018 May 18. Available from: https://seer.cancer.gov/statfacts/html/testis.html.3. Znaor A, Lortet-Tieulent J, Jemal A, Bray F. International variations and trends in testicular cancer incidence and mortality. Eur Urol. 2014; 65:1095–1106. PMID: 24268506.
Article4. Cancer Research UK. Testicular cancer statistics [Internet]. Cancer Research UK;updated 2018 Feb. cited 2018 May 18. Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/testicular-cancer.5. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008; 454:436–444. PMID: 18650914.
Article6. Zahorec R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001; 102:5–14. PMID: 11723675.7. Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013; 88:218–230. PMID: 23602134.
Article8. Jung MR, Park YK, Jeong O, Seon JW, Ryu SY, Kim DY, et al. Elevated preoperative neutrophil to lymphocyte ratio predicts poor survival following resection in late stage gastric cancer. J Surg Oncol. 2011; 104:504–510. PMID: 21618251.
Article9. Gomez D, Farid S, Malik HZ, Young AL, Toogood GJ, Lodge JP, et al. Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J Surg. 2008; 32:1757–1762. PMID: 18340479.
Article10. Ohno Y, Nakashima J, Ohori M, Hatano T, Tachibana M. Pretreatment neutrophil-to-lymphocyte ratio as an independent predictor of recurrence in patients with nonmetastatic renal cell carcinoma. J Urol. 2010; 184:873–878. PMID: 20643463.
Article11. Jang WS, Cho KS, Kim KH, Yoon CY, Kang YJ, Lee JY, et al. Prognostic impact of preoperative neutrophil-to-lymphocyte ratio after radical prostatectomy in localized prostate cancer. Prostate Cancer Prostatic Dis. 2016; 19:298–304. PMID: 27349499.
Article12. Viers BR, Boorjian SA, Frank I, Tarrell RF, Thapa P, Karnes RJ, et al. Pretreatment neutrophil-to-lymphocyte ratio is associated with advanced pathologic tumor stage and increased cancer-specific mortality among patients with urothelial carcinoma of the bladder undergoing radical cystectomy. Eur Urol. 2014; 66:1157–1164. PMID: 24630414.
Article13. Tan YG, Eu EWC, Huang HH, Lau WKO. High neutrophil-to-lymphocyte ratio predicts worse overall survival in patients with advanced/metastatic urothelial bladder cancer. Int J Urol. 2018; 25:232–238. PMID: 29094397.
Article14. Bolat D, Aydoğdu Ö, Polat S, Yarımoğlu S, Bozkurt İH, Yonguç T, et al. Predictive value of preoperative neutrophil-to-lymphocyte ratio on the prognosis of germ cell testicular tumors. Turk J Urol. 2017; 43:55–61. PMID: 28270952.
Article15. Jankovich M, Jankovichova T, Ondrus D, Breza J. Neutrophil-to-lymphocyte ratio as a predictor of preoperative tumor staging in testicular germ cell tumors. Bratisl Lek Listy. 2017; 118:510–512. PMID: 29061055.
Article16. Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res. 2009; 15:425–430. PMID: 19147746.
Article17. Schepisi G, Santoni M, Massari F, Gurioli G, Salvi S, Conteduca V, et al. Urothelial cancer: inflammatory mediators and implications for immunotherapy. BioDrugs. 2016; 30:263–273. PMID: 27177757.
Article18. Cho H, Hur HW, Kim SW, Kim SH, Kim JH, Kim YT, et al. Pre-treatment neutrophil to lymphocyte ratio is elevated in epithelial ovarian cancer and predicts survival after treatment. Cancer Immunol Immunother. 2009; 58:15–23. PMID: 18414853.
Article19. Kumari N, Dwarakanath BS, Das A, Bhatt AN. Role of interleukin-6 in cancer progression and therapeutic resistance. Tumour Biol. 2016; 37:11553–11572. PMID: 27260630.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Preoperative Inflammatory Parameters in Gastric Cancer Patients
- The Neutrophil-Lymphocyte Ratio and Platelet-Lymphocyte Ratio Are Prognostic Factors in Patients with Locally Advanced Pancreatic Cancer Treated with Chemoradiotherapy
- The Role of Neutrophil-to-Lymphocyte Ratio in Predicting Pathological Response for Resectable Non–Small Cell Lung Cancer Treated with Neoadjuvant Chemotherapy Combined with PD-1 Checkpoint Inhibitors
- Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio in Hepatocellular Carcinoma Treated with Stereotactic Body Radiotherapy
- The effectiveness of postoperative neutrophils to lymphocytes ratio in predicting long-term recurrence after stomach cancer surgery