Pediatr Infect Vaccine.
2019 Apr;26(1):22-31. 10.14776/piv.2019.26.e3.
Campylobacter Enteritis: Clinical Features and Laboratory Findings in Children Treated at a Single Hospital
- Affiliations
-
- 1Department of Pediatrics, Nowon Eulji Medical Center, Eulji University, Seoul, the Republic of Korea. aym3216@eulji.ac.kr
- 2Eulji University, College of Medicine, Daejeon, the Republic of Korea.
- 3Infectious Disease Team, Seoul Metropolitan Government Research Institute of Public Health and Environment, Seoul, the Republic of Korea.
- 4Department of Pediatrics, Eulji University School of Medicine, Daejeon, the Republic of Korea.
- KMID: 2443162
- DOI: http://doi.org/10.14776/piv.2019.26.e3
Abstract
- PURPOSE
Campylobacter species are common causes of bacterial enteritis. There is limited knowledge on its prevalence and clinical features because of its fastidious culture conditions. The purpose of this study was to identify the clinical features of Campylobacter enteritis in children.
METHODS
We obtained stool specimens from patients diagnosed with acute gastroenteritis in the Department of Pediatrics, Nowon Eulji Medical Center (NEMC) and identified the pathogens by performing cultures or polymerase chain reactions (PCR). We retrospectively reviewed the medical records of patients with Campylobacter enteritis at NEMC between January 2012 and December 2017.
RESULTS
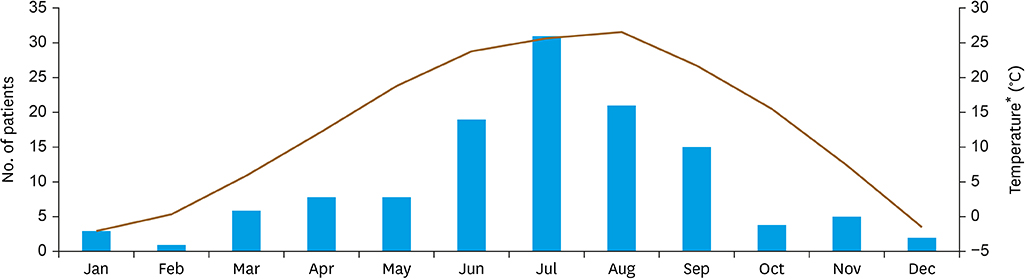
Overall, 123 patients were diagnosed with Campylobacter enteritis (60 by culture and PCR in EnterNet and 110 by multiplex PCR). The median (interquartile range [IQR]) age of patients was 12 years (IQR, 8 to 16 years). The disease occurred all year round, but 69.9% from June to September. Symptoms included diarrhea (97.6%), fever (96.7%), abdominal pain (94.3%), vomiting (37.4%), and headache (34.1%). Compared with other treatments, treatment with azithromycin was associated with a shorter hospitalization period (P<0.05).
CONCLUSIONS
Campylobacter enteritis is common during summer and mostly infects adolescent patients. It causes severe abdominal pain and fever preceding the onset of diarrhea. Prompt diagnosis and appropriate use of antibiotics reduces the duration of the disease.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim SY, Kim HJ, Shin EH, Eun BW, Ahn YM, Song MO. Etiology and clinical features of acute bacterial gastroenteritis in children mananged at a secondary hospital. Pediatr Infect Vaccine. 2017; 24:95–101.
Article2. Skirrow MB. Campylobacter enteritis: a “new” disease. BMJ. 1977; 2:9–11.3. Blaser MJ. Epidemiologic and clinical features of Campylobacter jejuni infections. J Infect Dis. 1997; 176:Suppl 2. S103–S105.4. Hou FQ, Sun XT, Wang GQ. Clinical manifestations of Campylobacter jejuni infection in adolescents and adults, and change in antibiotic resistance of the pathogen over the past 16 years. Scand J Infect Dis. 2012; 44:439–443.
Article5. Karmali MA, Fleming PC. Campylobacter enteritis in children. J Pediatr. 1979; 94:527–533.6. Skirrow MB. A demographic survey of Campylobacter, salmonella and shigella infections in England. A public health laboratory service survey. Epidemiol Infect. 1987; 99:647–657.
Article7. Feodoroff B, Lauhio A, Ellström P, Rautelin H. A nationwide study of Campylobacter jejuni and Campylobacter coli bacteremia in Finland over a 10-year period, 1998–2007, with special reference to clinical characteristics and antimicrobial susceptibility. Clin Infect Dis. 2011; 53:e99–e106.8. Fitzgerald C. Campylobacter. Clin Lab Med. 2015; 35:289–298.
Article9. Grzybowska-Chlebowczyk U, Kalita B, Flak-Wancerz A, Jasielska M, Więcek S, Wojcieszyn M, et al. Clinical course of Campylobacter infections in children. Pediatr Pol. 2013; 88:329–334.10. Borgnolo G, Barbone F, Guidobaldi G, Olivo G. C-reactive protein in viral and bacterial gastroenteritis in childhood. Acta Paediatr. 1996; 85:670–674.
Article11. Yoon CS. Ultrasonography of gastrointestinal emergencies in infantile and pedeatric patients. J Korean Soc Med Ultrasound. 2001; 20:239–256.12. Ma SH. Acute infectious diarrhea in pediatirc patients. Korean J Pediatr. 2005; 48:235–250.13. Kim SM, Choi MR, Kwon PS, Song HJ, Jang IH, Chong YS. Prevalence and antimicrobial susceptibility of Campylobacter coli isolates from swine. J Bacteriol Virol. 2011; 41:27–35.
Article14. de Boer RF, Ott A, Güren P, van Zanten E, van Belkum A, Kooistra-Smid AM. Detection of Campylobacter species and Arcobacter butzleri in stool samples by use of real-time multiplex PCR. J Clin Microbiol. 2013; 51:253–259.
Article15. Gormley FJ, Macrae M, Forbes KJ, Ogden ID, Dallas JF, Strachan NJ. Has retail chicken played a role in the decline of human campylobacteriosis? Appl Environ Microbiol. 2008; 74:383–390.
Article16. Sheppard SK, Dallas JF, Strachan NJ, MacRae M, McCarthy ND, Wilson DJ, et al. Campylobacter genotyping to determine the source of human infection. Clin Infect Dis. 2009; 48:1072–1078.
Article17. Oporto B, Esteban JI, Aduriz G, Juste RA, Hurtado A. Prevalence and strain diversity of thermophilic campylobacters in cattle, sheep and swine farms. J Appl Microbiol. 2007; 103:977–984.
Article18. Fullerton KE, Ingram LA, Jones TF, Anderson BJ, McCarthy PV, Hurd S, et al. Sporadic Campylobacter infection in infants: a population-based surveillance case-control study. Pediatr Infect Dis J. 2007; 26:19–24.19. Ruiz-Palacios GM, Calva JJ, Pickering LK, Lopez-Vidal Y, Volkow P, Pezzarossi H, et al. Protection of breast-fed infants against Campylobacter diarrhea by antibodies in human milk. J Pediatr. 1990; 116:707–713.
Article