J Korean Med Sci.
2023 Mar;38(9):e67. 10.3346/jkms.2023.38.e67.
Epidemiologic and Clinical Features of Campylobacter Enteritis Before and During COVID-19 in Korea
- Affiliations
-
- 1Department of Pediatrics, Kangwon National University School of Medicine, Chuncheon, Korea
- 2Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- KMID: 2540125
- DOI: http://doi.org/10.3346/jkms.2023.38.e67
Abstract
- Background
With the increase in meals at home due to coronavirus disease 2019 (COVID-19), the pattern and incidence of enteritis seemed to change. Some types of enteritis, such as Campylobacter enteritis, appear to have increased. Our study aimed to evaluate the change in the trend of enteritis, especially Campylobacter enteritis, before COVID-19 (2016– 2019) and at the present time during COVID-19 in South Korea.
Methods
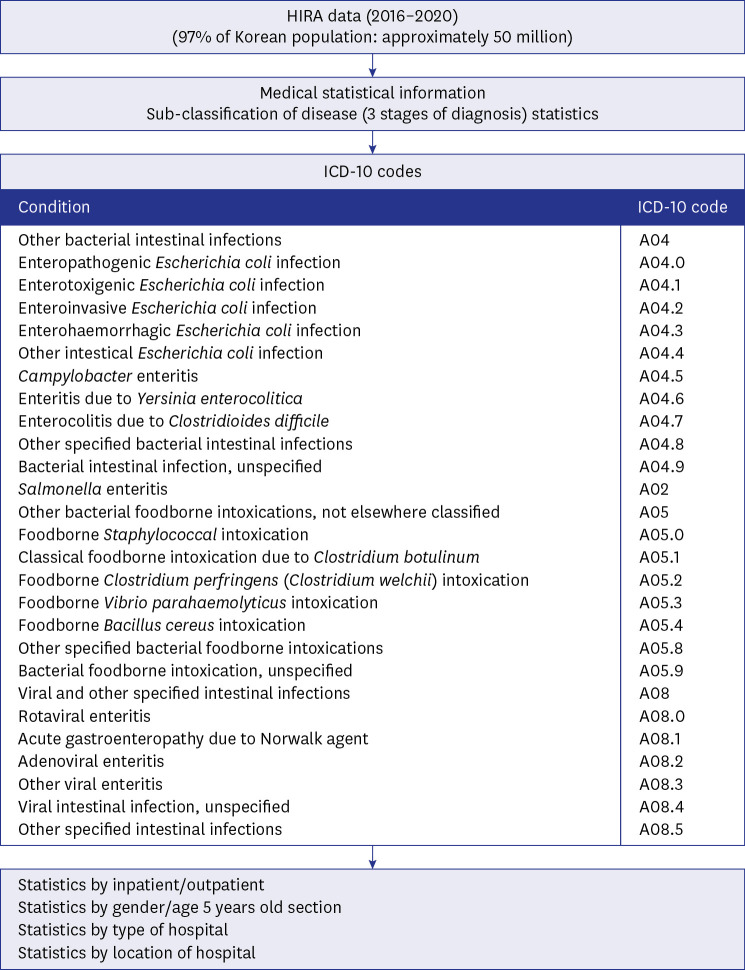
We analyzed data from the Health Insurance Review and Assessment Service. From 2016 to 2020, the International Classification of Diseases codes related to enteritis were examined to distinguish bacterial and viral enteritis and the trends of each were analyzed. The aspects of enteritis, before and after the COVID-19 outbreak, were compared.
Results
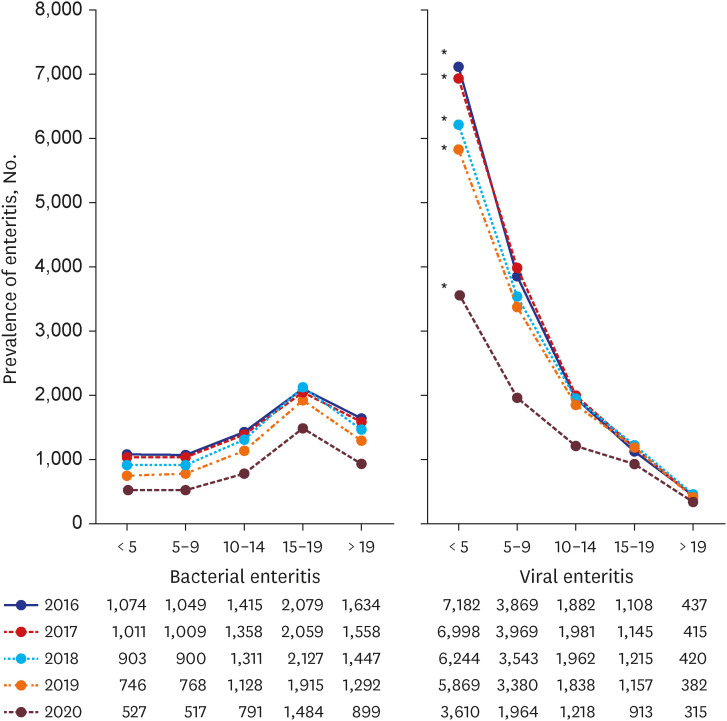
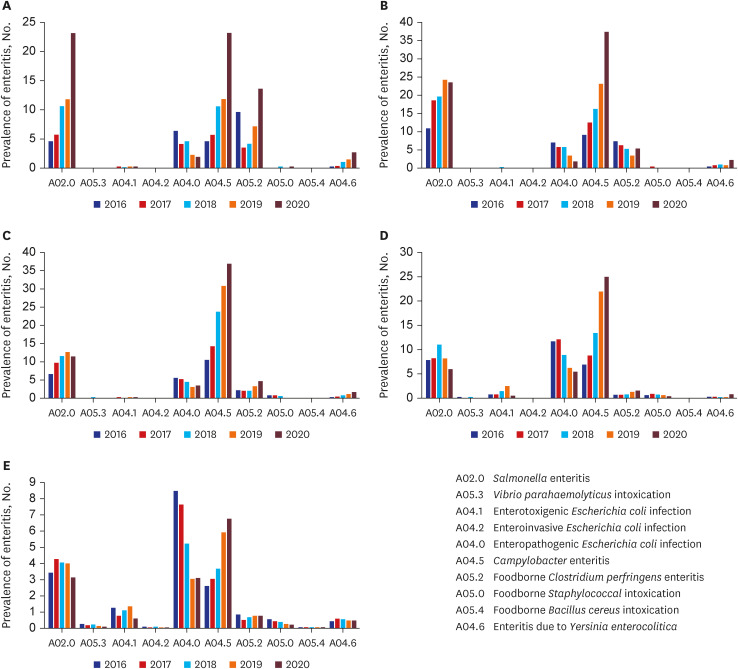
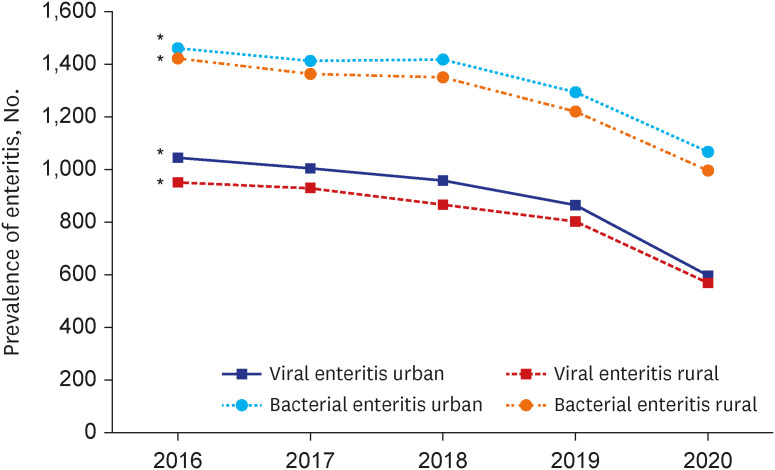
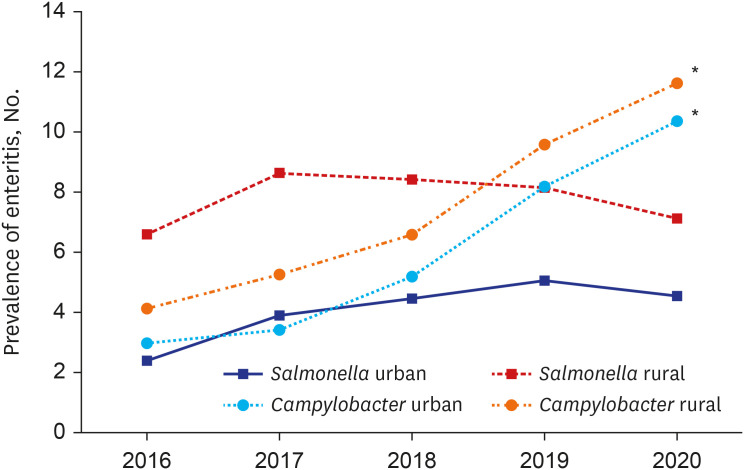
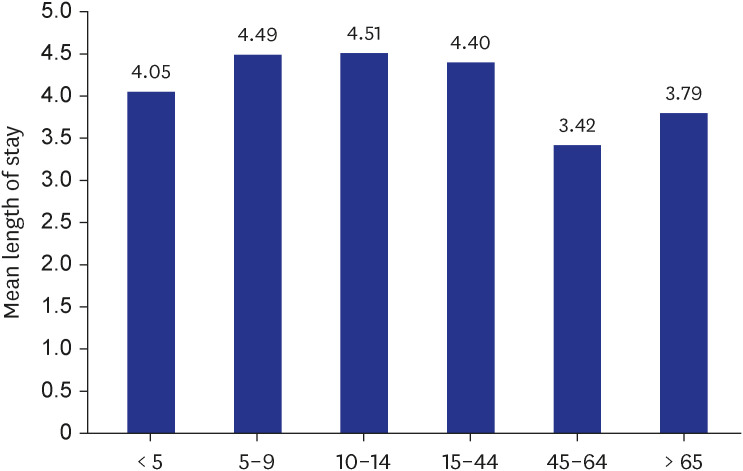
Both bacterial and viral enteritis declined in all age groups from 2016 to 2020 (P< 0.001). In 2020, the reduction rate of viral enteritis was higher than that of bacterial enteritis. However, unlike other causes of enteritis, even after COVID-19, Campylobacter enteritis increased in all age groups. An increase of Campylobacter enteritis in 2020 was particularly noticeable in children and adolescents. The prevalence of viral and bacterial enteritis was higher in urban areas than in rural areas (P < 0.001). Campylobacter enteritis was more common in the rural areas (P< 0.001).
Conclusion
Although the prevalence of bacterial and viral enteritis have decreased in COVID-19, Campylobacter enteritis has increased in all age groups and in rural areas compared to urban areas. Recognizing that the trend of Campylobacter enteritis before and during COVID-19 is helpful for future public health measures and interventions.
Keyword
Figure
Reference
-
1. Kim N, Hong S, Chun J, Hwang K. Laboratory-based surveillance of water-and food-borne infectious disease-causing bacteria in the Republic of Korea, 2016-2018. Public Health Wkly Rep. 2019; 12:898–903.2. Yoo M, Chung SH, Park YS, Oh IH, Chae WY, Kim SH, et al. Clinical characteristics of Campylobacter enterocolitis in Korean adults: a retrospective study at a single center. Korean J Gastroenterol. 2020; 75:188–197. PMID: 32326685.3. Francois Watkins LK, Laughlin ME, Joseph LA, Chen JC, Nichols M, Basler C, et al. Ongoing outbreak of extensively drug-resistant Campylobacter jejuni infections associated with US pet store puppies, 2016-2020. JAMA Netw Open. 2021; 4(9):e2125203. PMID: 34524434.4. Qayed E, Srinivasan S, Shahnavaz N. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment. 11th ed. Philadelphia, PA, USA: Elsevier Health Sciences;2020.5. Ahn SY, Park JY, Lim IS, Chae SA, Yun SW, Lee NM, et al. Changes in the occurrence of gastrointestinal infections after COVID-19 in Korea. J Korean Med Sci. 2021; 36(24):e180. PMID: 34155841.6. Pines JM, Zocchi MS, Black BS, Carlson JN, Celedon P, Moghtaderi A, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2021; 41:201–204. PMID: 33257144.7. Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020; 76(5):595–601. PMID: 33008651.8. Xiao J, Dai J, Hu J, Liu T, Gong D, Li X, et al. Co-benefits of nonpharmaceutical intervention against COVID-19 on infectious diseases in China: a large population-based observational study. Lancet Reg Health West Pac. 2021; 17:100282. PMID: 34611630.9. Ullrich A, Schranz M, Rexroth U, Hamouda O, Schaade L, Diercke M, et al. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: an analysis of national surveillance data during week 1-2016 - week 32-2020. Lancet Reg Health Eur. 2021; 6:100103. PMID: 34557831.10. Kraay AN, Han P, Kambhampati AK, Wikswo ME, Mirza SA, Lopman BA. Impact of nonpharmaceutical interventions for severe acute respiratory syndrome coronavirus 2 on norovirus outbreaks: an analysis of outbreaks reported by 9 US states. J Infect Dis. 2021; 224(1):9–13. PMID: 33606027.11. Nisavanh A, Horrigue I, Debin M, Turbelin C, Kengne-Kuetche C, Nassany O, et al. Epidemiology of acute gastroenteritis in France from November 2019-August 2021, in light of reported adherence to COVID-19 barrier measures. Sci Rep. 2022; 12(1):17504. PMID: 36261604.12. Cho SR, Chae SJ, Jung S, Choi W, Han MG, Yoo CK, et al. Trends in acute viral gastroenteritis among children aged ≤5 years through the national surveillance system in South Korea, 2013-2019. J Med Virol. 2021; 93(8):4875–4882. PMID: 33219526.13. Kim HS, Rotundo L, Nasereddin T, Ike A, Song D, Babar A, et al. Time trends and predictors of acute gastroenteritis in the United States. J Clin Gastroenterol. 2017; 51(8):693–700. PMID: 28787355.14. Sher AA, Ashraf MA, Mustafa BE, Raza MM. Epidemiological trends of foodborne Campylobacter outbreaks in the United States of America, 1998-2016. Food Microbiol. 2021; 97:103751. PMID: 33653524.15. Moffatt C. Examining the epidemiology of campylobacteriosis in Australia [dissertation]. Canberra, Australia: The Australian National University;2021.16. Bolton DJ. Campylobacter virulence and survival factors. Food Microbiol. 2015; 48:99–108. PMID: 25790997.17. Lévesque S, Fournier E, Carrier N, Frost E, Arbeit RD, Michaud S. Campylobacteriosis in urban versus rural areas: a case-case study integrated with molecular typing to validate risk factors and to attribute sources of infection. PLoS One. 2013; 8(12):e83731. PMID: 24386265.18. Rural Development Administration. Updated 2022. Accessed November 15, 2022. https://www.rda.go.kr/board/board.do?boardId=farmprmninfo&prgId=day_farmprmninfoEntry&currPage=1&dataNo=100000775354&mode=updateCnt&searchSDate=&searchEDate=&totalSearchYn=Y .19. Rha JY, Lee B, Nam Y, Yoon J. COVID-19 and changes in Korean consumers’ dietary attitudes and behaviors. Nutr Res Pract. 2021; 15(Suppl 1):S94–109. PMID: 34909136.20. Altig D, Baker S, Barrero JM, Bloom N, Bunn P, Chen S, et al. Economic uncertainty before and during the COVID-19 pandemic. J Public Econ. 2020; 191:104274. PMID: 32921841.21. Langeland S. COVID-19 lockdowns are central planning. Liberty Univ J Statesmanship Public Policy. 2021; 2(1):3.22. Unnikrishnan A, Figliozzi MA. A Study of the Impact of COVID-19 on Home Delivery Purchases and Expenditures. Portland, OR, USA: Portland State University;2020.23. Nelson W, Harris B. Campylobacteriosis rates show age-related static bimodal and seasonality trends. N Z Med J. 2011; 124(1337):33–39.24. Chen J, Sun XT, Zeng Z, Yu YY. Campylobacter enteritis in adult patients with acute diarrhea from 2005 to 2009 in Beijing, China. Chin Med J (Engl). 2011; 124(10):1508–1512. PMID: 21740807.25. Kim SG, Jung HK, Lee HL, Jang JY, Lee H, Kim CG, et al. Guidelines for the diagnosis and treatment of Helicobacter pylori infection in Korea, 2013 revised edition. J Gastroenterol Hepatol. 2014; 29(7):1371–1386. PMID: 24758240.26. Prescott SL, Wegienka G, Logan AC, Katz DL. Dysbiotic drift and biopsychosocial medicine: how the microbiome links personal, public and planetary health. Biopsychosoc Med. 2018; 12(1):7. PMID: 29743938.27. Green MS, Schwartz N, Peer V. Sex differences in campylobacteriosis incidence rates at different ages - a seven country, multi-year, meta-analysis. A potential mechanism for the infection. BMC Infect Dis. 2020; 20(1):625. PMID: 32842973.28. Gameiro CM, Romão F, Castelo-Branco C. Menopause and aging: changes in the immune system--a review. Maturitas. 2010; 67(4):316–320. PMID: 20813470.29. Sibbald CJ, Sharp JC. Campylobacter infection in urban and rural populations in Scotland. J Hyg (Lond). 1985; 95(1):87–93. PMID: 3839516.30. Lal A, Ikeda T, French N, Baker MG, Hales S. Climate variability, weather and enteric disease incidence in New Zealand: time series analysis. PLoS One. 2013; 8(12):e83484. PMID: 24376707.31. Oberheim J. Weather conditions and campylobacteriosis in Germany [dissertation]. Bonn, Germany: University of Bonn;2020.32. Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021; 11(3):e045343.33. Karikari AB, Obiri-Danso K, Frimpong EH, Krogfelt KA. Antibiotic resistance in Campylobacter isolated from patients with gastroenteritis in a teaching hospital in Ghana. Open J Med Microbiol. 2017; 7(1):1–11.34. Allos BM. Association between Campylobacter infection and Guillain-Barré syndrome. J Infect Dis. 1997; 176(Suppl 2):S125–S128. PMID: 9396695.35. Zachariah OH, Lizzy MA, Rose K, Angela MM. Multiple drug resistance of Campylobacter jejuni and Shigella isolated from diarrhoeic children at Kapsabet County referral hospital, Kenya. BMC Infect Dis. 2021; 21(1):109. PMID: 33485326.36. Cho H, Kwon JW. Prevalence of anaphylaxis and prescription rates of epinephrine auto-injectors in urban and rural areas of Korea. Korean J Intern Med. 2019; 34(3):643–650. PMID: 30360025.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neonatal Campylobacter enteritis
- An Outbreak of Campylobacter Jejuni Involving Healthcare Workers Detected by COVID-19 Healthcare Worker Symptom Surveillance
- Epidemiologic Changes in Over 10 Years of Community-Acquired Bacterial Enteritis in Children
- Campylobacter Enteritis: Clinical Features and Laboratory Findings in Children Treated at a Single Hospital
- Report on the Epidemiological Features of Coronavirus Disease 2019 (COVID-19) Outbreak in the Republic of Korea from January 19 to March 2, 2020